Anesth Pain Med.
2023 Jan;18(1):75-83. 10.17085/apm.22181.
Evaluation of distal skin temperature and tissue oxygen saturation determined by near-infrared spectroscopy for predicting ultrasound-guided lateral infraclavicular block success
- Affiliations
-
- 1Department of Anesthesiology and Reanimation, Selçuk University Faculty of Medicine, Konya, Turkey
- KMID: 2540338
- DOI: http://doi.org/10.17085/apm.22181
Abstract
- Background
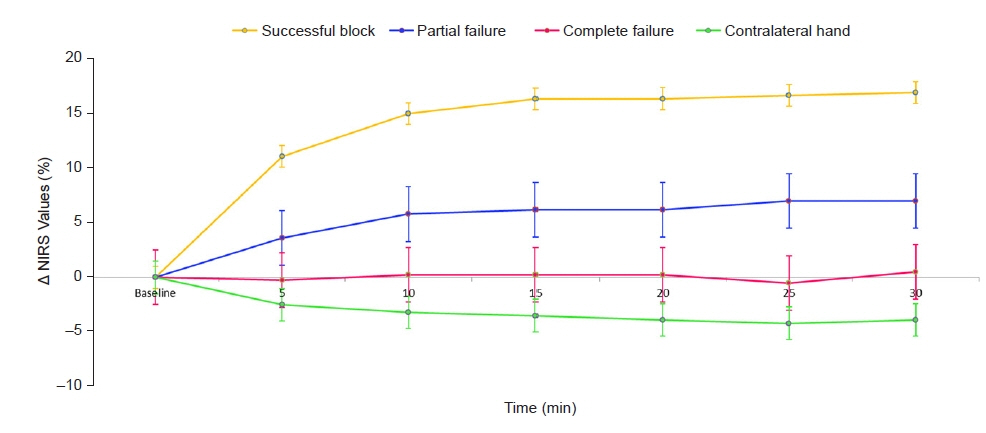
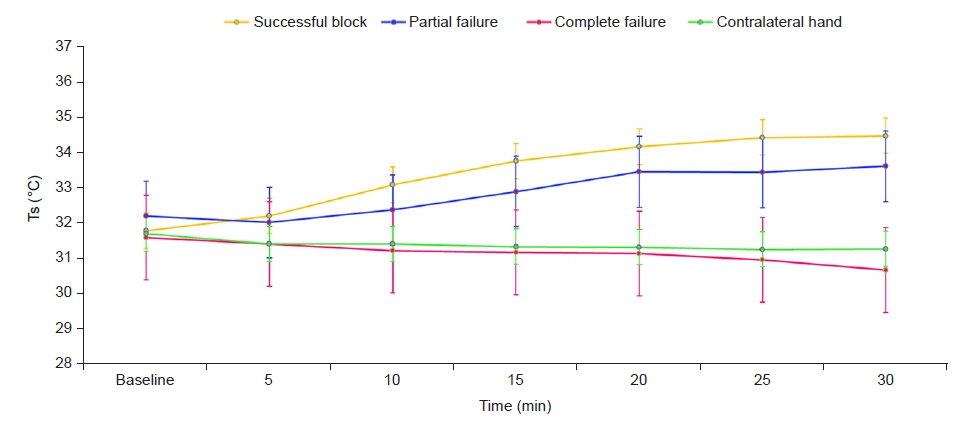
Changes in tissue oxygen saturation determined by near-infrared spectroscopy (NIRS) may help predict and determine the success of a lateral infraclavicular (LIC) block.We investigated whether evaluation of tissue oxygen saturation determined by NIRS couldbe an indicator of LIC block success.Methods: Forty patients scheduled for hand or forearm surgery under LIC block were studied. NIRS sensors were placed on the ventral aspect of both mid-forearms, and the contralateral hand was used as the control group. NIRS values were recorded before the block andat regular intervals during the following 30 min.Results: NIRS values were significantly higher in the successfully blocked patients whencompared to the complete failure, partial failure, and contralateral hand groups at the 10thmin. In the successfully blocked patients, NIRS values (mean ± SD [change in %]) increasedby 11.09 ± 4.86 (16.03%), 15.00 ± 4.53 (21.76%), 16.35 ± 5.14 (23.77%), 16.38 ± 4.88(23.85%), 16.67 ± 5.04 (24.29%), and 16.96 ± 5.71 (24.78%), respectively, from baselineto 5, 10, 15, 20, 25, and 30 min. ΔTs values were significantly higher in the successfullyblocked patients than in the complete failure patients and contralateral hand at the 30thmin. However, there was no statistically significant difference when comparing ΔTs values ofsuccessful block and partial failure block patients at the 30th min.Conclusions: We conclude that measurement of tissue oxygen saturation by NIRS withinthe scope of evaluation of the lateral infraclavicular block is a rapid, effective, and applicabletechnique.
Keyword
Figure
Reference
-
1. Sandhu NS, Manne JS, Medabalmi PK, Capan LM. Sonographically guided infraclavicular brachial plexus block in adults: a retrospective analysis of 1146 cases. J Ultrasound Med. 2006; 25:1555–61.2. Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth. 2002; 89:254–9.
Article3. Arcand G, Williams SR, Chouinard P, Boudreault D, Harris P, Ruel M, et al. Ultrasound-guided infraclavicular versus supraclavicular block. Anesth Analg. 2005; 101:886–90.
Article4. Curatolo M, Petersen-Felix S, Arendt-Nielsen L. Assessment of regional analgesia in clinical practice and research. Br Med Bull. 2005; 71:61–76.
Article5. Paqueron X, Gentili ME, Willer JC, Coriat P, Riou B. Time sequence of sensory changes after upper extremity block: swelling sensation is an early and accurate predictor of success. Anesthesiology. 2004; 101:162–8.6. Galvin EM, Niehof S, Medina HJ, Zijlstra FJ, van Bommel J, Klein J, et al. Thermographic temperature measurement compared with pinprick and cold sensation in predicting the effectiveness of regional blocks. Anesth Analg. 2006; 102:598–604.
Article7. Hermanns H, Braun S, Werdehausen R, Werner A, Lipfert P, Stevens MF. Skin temperature after interscalene brachial plexus blockade. Reg Anesth Pain Med. 2007; 32:481–7.
Article8. Minville V, Gendre A, Hirsch J, Silva S, Bourdet B, Barbero C, et al. The efficacy of skin temperature for block assessment after infraclavicular brachial plexus block. Anesth Analg. 2009; 108:1034–6.
Article9. Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009; 103 Suppl 1:i3–13.
Article10. Desgagnés MC, Lévesque S, Dion N, Nadeau MJ, Coté D, Brassard J, et al. A comparison of a single or triple injection technique for ultrasound-guided infraclavicular block: a prospective randomized controlled study. Anesth Analg. 2009; 109:668–72.
Article11. Tighe PJ, Elliott CE, Lucas SD, Boezaart AP. Noninvasive tissue oxygen saturation determined by near-infrared spectroscopy following peripheral nerve block. Acta Anaesthesiol Scand. 2011; 55:1239–46.
Article12. Lange KH, Jansen T, Asghar S, Kristensen PL, Skjønnemand M, Nørgaard P. Skin temperature measured by infrared thermography after specific ultrasound-guided blocking of the musculocutaneous, radial, ulnar, and median nerves in the upper extremity. Br J Anaesth. 2011; 106:887–95.
Article13. Yarnitsky D, Ochoa JL. Warm and cold specific somatosensory systems. Psychophysical thresholds, reaction times and peripheral conduction velocities. Brain. 1991; 114(Pt 4):1819–26.
Article14. Fowler CJ, Sitzoglou K, Ali Z, Halonen P. The conduction velocities of peripheral nerve fibres conveying sensations of warming and cooling. J Neurol Neurosurg Psychiatry. 1988; 51:1164–70.
Article15. Burke D, Mackenzie RA, Skuse NF, Lethlean AK. Cutaneous afferent activity in median and radial nerve fascicles: a microelectrode study. J Neurol Neurosurg Psychiatry. 1975; 38:855–64.
Article16. Robertson D, Biaggioni I, Burnstock G, Low PA, Paton JFR. Primer on the autonomic nervous system. 3rd ed. San Diego (CA): Academic Press;2012.17. Asghar S, Lange KHW, Lundstrøm LH. Blinded observer evaluation of distal skin temperature for predicting lateral infraclavicular block success. Anesth Analg 2015; 120: 246-51. Erratum in: Anesth Analg. 2015; 121:577.18. Asghar S, Bjerregaard LS, Lundstrøm LH, Lund J, Jenstrup MT, Lange KH. Distal infrared thermography and skin temperature after ultrasound-guided interscalene brachial plexus block: a prospective observational study. Eur J Anaesthesiol. 2014; 31:626–34.19. Okano T, Okuda Y, Kimura Y, Mishio M, Shinohara M, Kitajima T. Use of near-infrared spectroscopy to evaluate stellate ganglion block. Reg Anesth Pain Med. 2001; 26:186.
Article20. Quaresima V, Ferrari M. More on the use of near-infrared spectroscopy to evaluate stellate ganglion block. Reg Anesth Pain Med. 2002; 27:111–2.
Article21. Galvin EM, Niehof S, Verbrugge SJ, Maissan I, Jahn A, Klein J, et al. Peripheral flow index is a reliable and early indicator of regional block success. Anesth Analg. 2006; 103:239–43.
Article22. Kabon B, Fleischmann E, Treschan T, Taguchi A, Kapral S, Kurz A. Thoracic epidural anesthesia increases tissue oxygenation during major abdominal surgery. Anesth Analg. 2003; 97:1812–7.
Article23. Cui W, Kumar C, Chance B. Experimental study of migration depth for the photons measured at sample surface. Proc SPIE. 1991; 1431:180–91.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of ultrasound-guided infraclavicular brachial plexus block: a comparison with nerve stimulation method
- Cerebral Oxygen Saturation Monitoring during Carotid Endarterectomy: A case report
- The Change in Regional Cerebral Oxygen Saturation after Stellate Ganglion Block
- Clinical Application of Near-Infrared Spectroscopy in Neonates
- Ultrasound-guided Nerve Block for Skin Grafting on Large Diabetic Ulcer of Foot and Leg: A Technical Report