J Korean Neurosurg Soc.
2023 Mar;66(2):211-218. 10.3340/jkns.2022.0156.
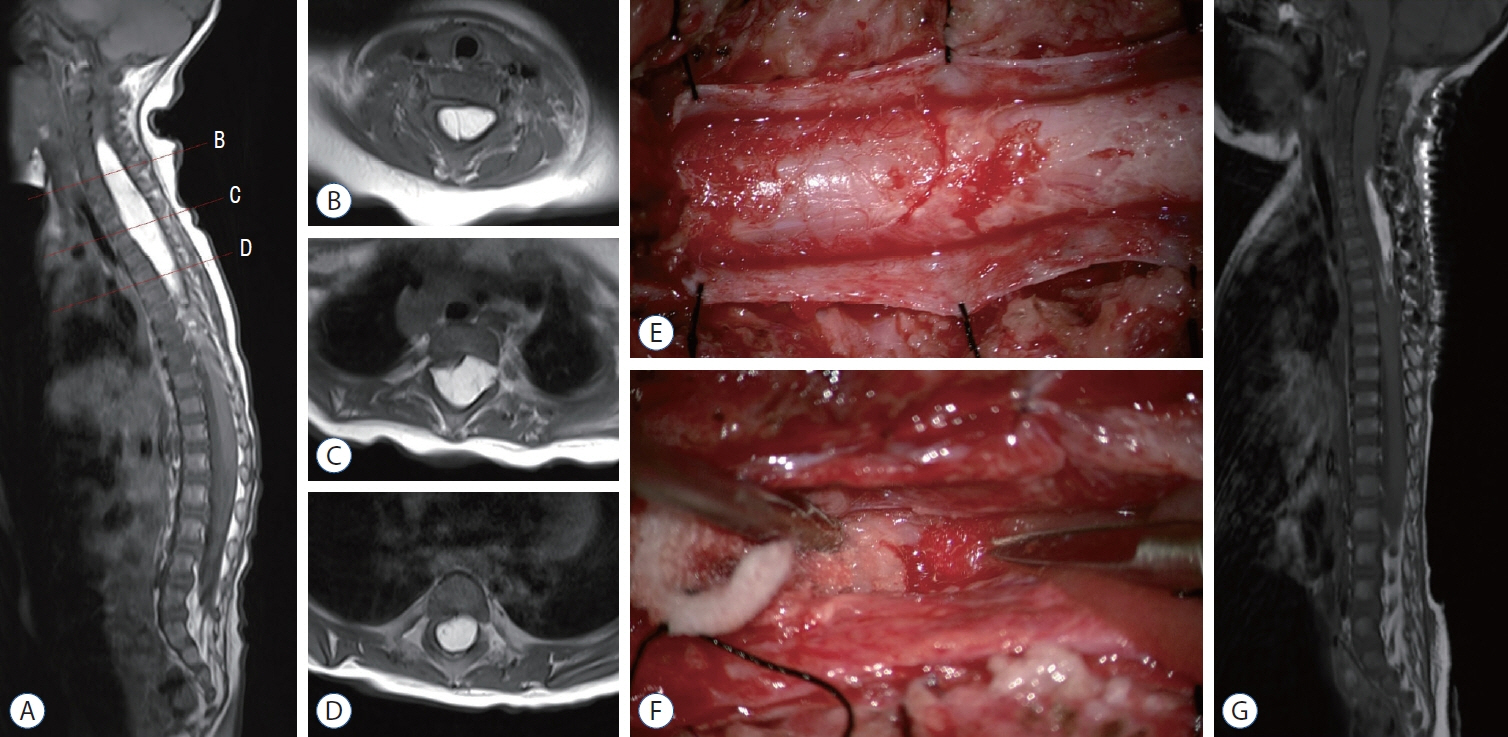
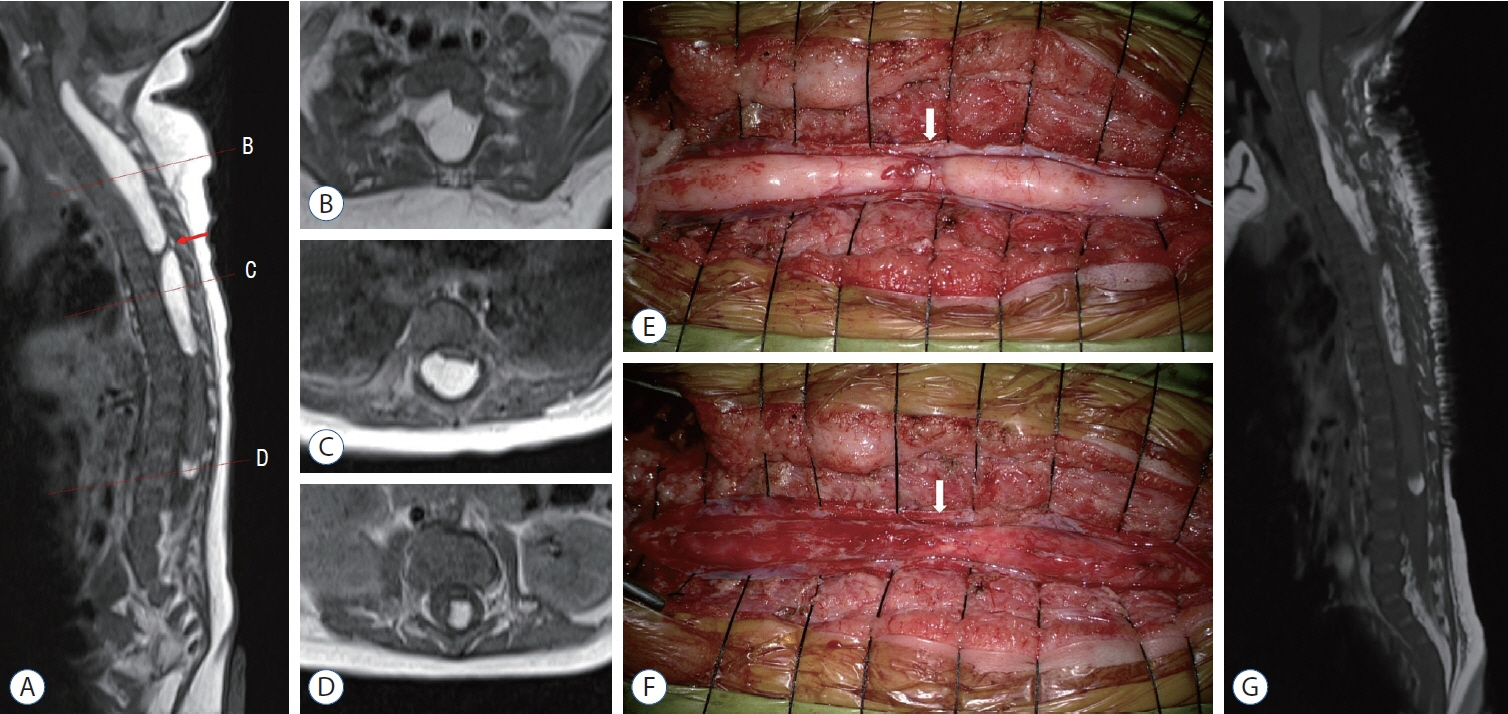
Pediatric Nondysraphic Intramedullary Lipoma : Report of Two Cases and Review of the Literature
- Affiliations
-
- 1Division of Pediatric Neurosurgery, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Pusan National University Hospital, Pusan National University School of Medicine and Biochemical Research Institute, Busan, Korea
- 3Department of Pediatrics, Chung-Ang University Hospital, College of Medicine, Chung-Ang University, Seoul, Korea
- KMID: 2539883
- DOI: http://doi.org/10.3340/jkns.2022.0156
Abstract
- Pediatric nondysraphic intramedullary lipoma is very rare, and only limited cases have been reported. In the present case, we present two infant patients with these pathologies who were surgically treated. Previous literature on 20 patients with these diseases who had undergone surgical treatments was analyzed. Surgical treatment should be considered in most symptomatic patients, and laminoplastic laminotomy and internal debulking of the lipoma under intraoperative neurophysiological monitoring are mostly recommended.
Figure
Reference
-
References
1. Abuzayed B, Alawneh K, Al Qawasmeh M, Raffee L. Nondysraphic spinal intramedullary lipoma: a rare case and management. Turk Arch Pediatr. 56:85–87. 2021.2. Bhatoe HS, Singh P, Chaturvedi A, Sahai K, Dutta V, Sahoo PK. Nondysraphic intramedullary spinal cord lipomas: a review. Neurosurg Focus. 18:ECP1. 2005.3. Bishnoi I, Singh P, Duggal G, Sorout S. A rare case of intramedullary lipoma of brainstem to thoracic cord--what to do? J Pediatr Neurosci. 15:145–149. 2020.4. Chagla AS, Balasubramaniam S, Goel AH. A massive cervicomedullary intramedullary spinal cord lipoma. J Clin Neurosci. 15:817–820. 2008.5. Chaskis C, Michotte A, Geffray F, Vangeneugden J, Desprechins B, D’Haens J. Cervical intramedullary lipoma with intracranial extension in an infant. Case illustration. J Neurosurg. 87:472. 1997.6. Fleming KL, Davidson L, Gonzalez-Gomez I, McComb JG. Nondysraphic pediatric intramedullary spinal cord lipomas: report of 5 cases. J Neurosurg Pediatr. 5:172–178. 2010.7. Kabir SM, Thompson D, Rezajooi K, Casey AT. Non-dysraphic intradural spinal cord lipoma: case series, literature review and guidelines for management. Acta Neurochir (Wien). 152:1139–1144. 2010.8. Kim CH, Wang KC, Kim SK, Chung YN, Choi YL, Chi JG, et al. Spinal intramedullary lipoma: report of three cases. Spinal Cord. 41:310–315. 2003.9. Kumar A, Chandra PS, Bisht A, Garg A, Mahapatra AK, Sharma MC. Successful surgical excision of a nondysraphic holodorsal intramedullary lipoma in a 14-month-old child. Pediatr Neurosurg. 47:272–274. 2011.10. Lee M, Rezai AR, Abbott R, Coelho DH, Epstein FJ. Intramedullary spinal cord lipomas. J Neurosurg. 82:394–400. 1995.11. Misawa H, Oda Y, Yamane K, Tetsunaga T, Ozaki T. Maximal resection of intramedullary lipoma using intraoperative ultrasonography: a technical note. Acta Med Okayama. 75:239–242. 2021.12. Morioka T, Murakami N, Shimogawa T, Mukae N, Hashiguchi K, Suzuki SO, et al. Neurosurgical management and pathology of lumbosacral lipomas with tethered cord. Neuropathology. 37:385–392. 2017.13. Morota N, Ihara S, Ogiwara H. New classification of spinal lipomas based on embryonic stage. J Neurosurg Pediatr. 19:428–439. 2017.14. Muthusubramanian V, Pande A, Vasudevan MC, Ramamurthi R. Concomitant cervical and lumbar intradural intramedullary lipoma. Surg Neurol. 69:314–317. 2008.15. Nguyen HS, Lew S. Extensive multilevel split laminotomy for debulking a cervicothoracolumbar nondysraphic intramedullary spinal-cord lipoma in a 2-month-old infant. Pediatr Neurosurg. 52:189–194. 2017.16. Sarris CE, Tomei KL, Carmel PW, Gandhi CD. Lipomyelomeningocele: pathology, treatment, and outcomes. Neurosurg Focus. 33:E3. 2012.17. Wykes V, Desai D, Thompson DN. Asymptomatic lumbosacral lipomas- -a natural history study. Childs Nerv Syst. 28:1731–1739. 2012.18. Yilmaz C, Aydemir F. Thoracic intramedullary lipoma in a 3-year-old child: spontaneous decrease in the size following incomplete resection. Asian J Neurosurg. 13:188–190. 2018.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intramedullary Spinal Cord Lipoma without Spinal Dysraphism
- Does this baby have a tail?: a case of congenital isolated perineal lipoma presenting as human pseudo-tail
- Lipoma of the Deep Neck Space
- Surgical Strategy for Colonic Intussusception Caused by a Giant Colonic Lipoma: A Report of Two Cases and a Review of the Literature
- Long Term Outcome of Non-Dysraphic Intramedullary Spinal Cord Lipomas in Adults: Case Series and Review