J Korean Med Sci.
2023 Feb;38(8):e64. 10.3346/jkms.2023.38.e64.
Effect of a Patient Blood Management Program on the Appropriateness of Red Blood Cell Transfusion and Clinical Outcomes in Elderly Patients Undergoing Hip Fracture Surgery
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 2Department of Anesthesiology and Pain Medicine, Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 3Department of Obstetrics and Gynecology, Korea University College of Medicine, Seoul, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Korea University College of Medicine, Seoul, Korea
- 5Department of Orthopedic Surgery, Korea University College of Medicine, Seoul, Korea
- KMID: 2539633
- DOI: http://doi.org/10.3346/jkms.2023.38.e64
Abstract
- Background
Elderly patients with hip fractures frequently receive perioperative transfusions, which are associated with increased morbidity and mortality. This study aimed to evaluate the impact of a patient blood management (PBM) program on the appropriateness of red blood cell (RBC) transfusion and clinical outcomes in geriatric patients undergoing hip fracture surgery.
Methods
In 2018, the revised PBM program was implemented at the Korea University Anam Hospital, Seoul, Republic of Korea. Elderly patients aged ≥ 65 years who underwent hip fracture surgery from 2017 to 2020 were evaluated. Clinical characteristics and outcomes were analyzed according to the timing of PBM implementation (pre-PBM, early-PBM, and late-PBM). Multiveriate regression analysis was used to evaluate the risk factors of the adverse outcomes, such as in-hospital mortality or 30-day readmission.
Results
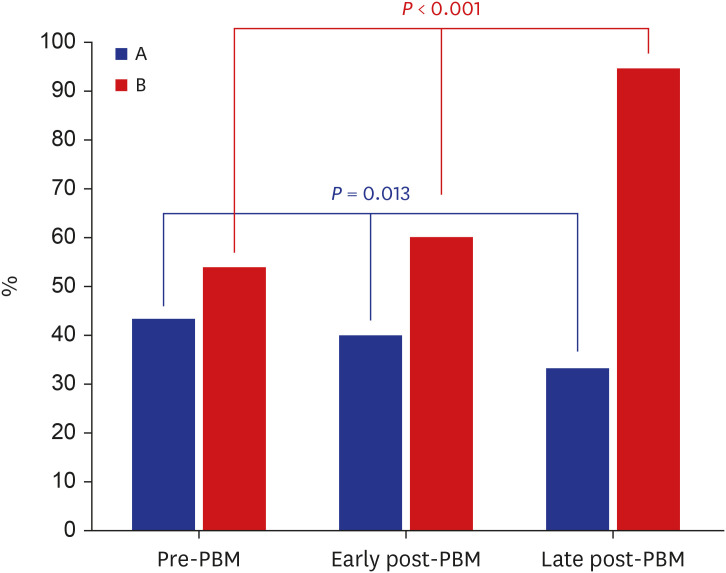
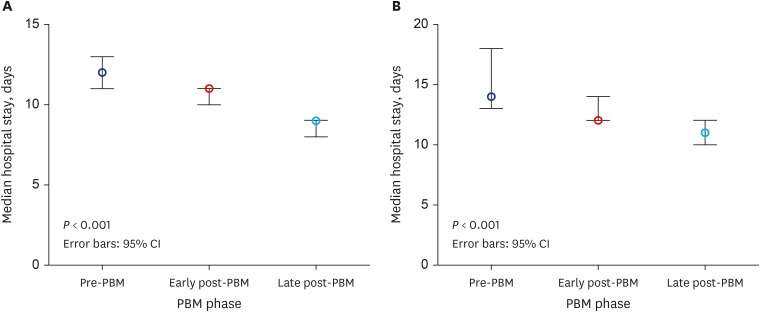
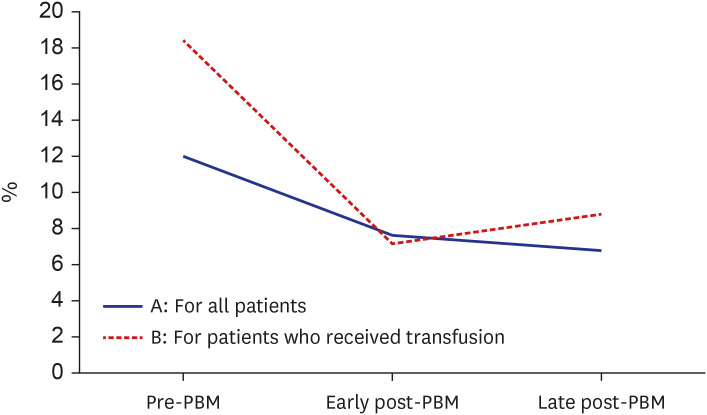
A total of 884 elderly patients were included in this study. The proportion of patients who received perioperative RBC transfusions decreased significantly (43.5%, 40.1%, and 33.2% for pre-PBM, early-PBM, and late-PBM, respectively; P = 0.013). However, the appropriateness of RBC transfusion significantly increased (54.0%, 60.1%, and 94.7%, respectively; P < 0.001). The duration of in-hospital stay and 30-day readmission rates significantly decreased. Multivariable regression analysis revealed that RBC transfusion (odds ratio, 1.815; 95% confidence interval, 1.137–2.899; P = 0.013) was significantly associated with adverse outcomes.
Conclusion
Implementing the PBM program increased the appropriateness of RBC transfusion without compromising transfusion quality and clinical outcomes. Therefore, adopting the PBM program may improve the clinical management of elderly patients following hip fracture surgery.
Keyword
Figure
Reference
-
1. Pedersen AB, Mehnert F, Overgaard S, Johnsen SP. Allogeneic blood transfusion and prognosis following total hip replacement: a population-based follow up study. BMC Musculoskelet Disord. 2009; 10(1):167. PMID: 20040083.
Article2. Smeets SJ, Verbruggen JP, Poeze M. Effect of blood transfusion on survival after hip fracture surgery. Eur J Orthop Surg Traumatol. 2018; 28(7):1297–1303. PMID: 29752534.
Article3. Verlicchi F, Desalvo F, Zanotti G, Morotti L, Tomasini I. Red cell transfusion in orthopaedic surgery: a benchmark study performed combining data from different data sources. Blood Transfus. 2011; 9(4):383–387. PMID: 21627924.4. Engoren M, Mitchell E, Perring P, Sferra J. The effect of erythrocyte blood transfusions on survival after surgery for hip fracture. J Trauma. 2008; 65(6):1411–1415. PMID: 19077635.
Article5. Spahn DR. Anemia and patient blood management in hip and knee surgery: a systematic review of the literature. Anesthesiology. 2010; 113(2):482–495. PMID: 20613475.6. Eisenstaedt R, Penninx BW, Woodman RC. Anemia in the elderly: current understanding and emerging concepts. Blood Rev. 2006; 20(4):213–226. PMID: 16472893.
Article7. Arshi A, Lai WC, Iglesias BC, McPherson EJ, Zeegen EN, Stavrakis AI, et al. Blood transfusion rates and predictors following geriatric hip fracture surgery. Hip Int. 2021; 31(2):272–279. PMID: 31912747.
Article8. Partridge J, Harari D, Gossage J, Dhesi J. Anaemia in the older surgical patient: a review of prevalence, causes, implications and management. J R Soc Med. 2013; 106(7):269–277. PMID: 23759887.
Article9. Smith GH, Tsang J, Molyneux SG, White TO. The hidden blood loss after hip fracture. Injury. 2011; 42(2):133–135. PMID: 20236640.
Article10. Koval KJ, Rosenberg AD, Zuckerman JD, Aharonoff GB, Skovron ML, Bernstein RL, et al. Does blood transfusion increase the risk of infection after hip fracture? J Orthop Trauma. 1997; 11(4):260–265. PMID: 9258823.
Article11. Shin HJ, Kim JH, Han SB, Park JH, Jang WY. Allogeneic red blood cell transfusion is an independent risk factor for 1-year mortality in elderly patients undergoing femoral neck fracture surgery: retrospective study. Medicine (Baltimore). 2020; 99(35):e21897. PMID: 32871921.12. Guo Y, Jia P, Zhang J, Wang X, Jiang H, Jiang W. Prevalence and risk factors of postoperative delirium in elderly hip fracture patients. J Int Med Res. 2016; 44(2):317–327. PMID: 26920926.
Article13. Gani F, Cerullo M, Ejaz A, Gupta PB, Demario VM, Johnston FM, et al. Implementation of a blood management program at a tertiary care hospital: effect on transfusion practices and clinical outcomes among patients undergoing surgery. Ann Surg. 2019; 269(6):1073–1079. PMID: 31082904.
Article14. Rineau E, Chaudet A, Chassier C, Bizot P, Lasocki S. Implementing a blood management protocol during the entire perioperative period allows a reduction in transfusion rate in major orthopedic surgery: a before-after study. Transfusion. 2016; 56(3):673–681. PMID: 26748489.
Article15. Shin HJ, Kim JH, Park Y, Ahn KH, Jung JS, Park JH, et al. Effect of patient blood management system and feedback programme on appropriateness of transfusion: an experience of Asia’s first Bloodless Medicine Center on a hospital basis. Transfus Med. 2021; 31(1):55–62. PMID: 33368693.
Article16. Jang SY, Cha YH, Yoo JI, Oh T, Kim JT, Park CH, et al. Blood transfusion for elderly patients with hip fracture: a nationwide cohort study. J Korean Med Sci. 2020; 35(37):e313. PMID: 32959543.
Article17. Suh YS, Lee JJ, Nho JH, Lee JJ, Won SH, Yang HJ. Transfusion trends in hip arthroplasty in Korea: a nationwide study by the Korean National Health Insurance Service. Transfusion. 2019; 59(7):2324–2333. PMID: 31022315.
Article18. Putot A, Zeller M, Perrin S, Beer JC, Ravisy J, Guenancia C, et al. Blood transfusion in elderly patients with acute myocardial infarction: data from the RICO survey. Am J Med. 2018; 131(4):422–429.e4. PMID: 29030059.
Article19. Amin RM, DeMario VM, Best MJ, Shafiq B, Hasenboehler EA, Sterling RS, et al. A restrictive hemoglobin transfusion threshold of less than 7 g/dL decreases blood utilization without compromising outcomes in patients with hip fractures. J Am Acad Orthop Surg. 2019; 27(23):887–894. PMID: 30829898.
Article20. Goodnough LT, Maggio P, Hadhazy E, Shieh L, Hernandez-Boussard T, Khari P, et al. Restrictive blood transfusion practices are associated with improved patient outcomes. Transfusion. 2014; 54(10 Pt 2):2753–2759. PMID: 24995770.
Article21. Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011; 365(26):2453–2462. PMID: 22168590.
Article22. Parker MJ. Randomised trial of blood transfusion versus a restrictive transfusion policy after hip fracture surgery. Injury. 2013; 44(12):1916–1918. PMID: 23756263.
Article23. Gregersen M, Borris LC, Damsgaard EM. Blood transfusion and overall quality of life after hip fracture in frail elderly patients--the transfusion requirements in frail elderly randomized controlled trial. J Am Med Dir Assoc. 2015; 16(9):762–766. PMID: 25933728.
Article24. Shander A, Goobie SM, Warner MA, Aapro M, Bisbe E, Perez-Calatayud AA, et al. Essential role of patient blood management in a pandemic: a call for action. Anesth Analg. 2020; 131(1):74–85. PMID: 32243296.
Article25. Cho SH. Need for patient blood management to prepare for an unstable blood supply crisis. Korean J Blood Transfus. 2021; 32(3):217–220.
Article26. Korea Centers for Disease Control and Prevention. Guidelines for Blood Transfusion. 4th ed. Cheongju, Korea: Korea Centers for Disease Control and Prevention;2016.27. Carson JL, Guyatt G, Heddle NM, Grossman BJ, Cohn CS, Fung MK, et al. Clinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA. 2016; 316(19):2025–2035. PMID: 27732721.28. Soumerai SB, Salem-Schatz S, Avorn J, Casteris CS, Ross-Degnan D, Popovsky MA. A controlled trial of educational outreach to improve blood transfusion practice. JAMA. 1993; 270(8):961–966. PMID: 8123097.
Article29. Salem-Schatz SR, Avorn J, Soumerai SB. Influence of clinical knowledge, organizational context, and practice style on transfusion decision making. Implications for practice change strategies. JAMA. 1990; 264(4):476–483. PMID: 2366281.
Article30. Liumbruno GM, Rafanelli D. Appropriateness of blood transfusion and physicians’ education: a continuous challenge for hospital transfusion committees? Blood Transfus. 2012; 10(1):1–3. PMID: 22044957.31. Haynes SL, Torella F. The role of hospital transfusion committees in blood product conservation. Transfus Med Rev. 2004; 18(2):93–104. PMID: 15067589.
Article32. Di Bartolomeo E, Merolle L, Marraccini C, Canovi L, Berni P, Guberti M, et al. Patient blood management: transfusion appropriateness in the post-operative period. Blood Transfus. 2019; 17(6):459–464. PMID: 31403929.33. Merolle L, Marraccini C, Di Bartolomeo E, Montella MT, Pertinhez TA, Baricchi R, et al. Postoperative patient blood management: transfusion appropriateness in cancer patients. Blood Transfus. 2020; 18(5):359–365. PMID: 32931414.34. Joy PJ, Bennet SJ. The appropriateness of blood transfusion following primary total hip replacement. Ann R Coll Surg Engl. 2012; 94(3):201–203. PMID: 22507728.
Article35. Park JW, Won SH, Moon SY, Lee YK, Ha YC, Koo KH. Burden and future projection of revision Total hip Arthroplasty in South Korea. BMC Musculoskelet Disord. 2021; 22(1):375. PMID: 33888097.
Article36. Gupta PB, DeMario VM, Amin RM, Gehrie EA, Goel R, Lee KH, et al. Patient blood management program improves blood use and clinical outcomes in orthopedic surgery. Anesthesiology. 2018; 129(6):1082–1091. PMID: 30124488.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Distribution of Hemoglobin Concentration before Transfusion for Evaluation of Appropriateness of Red Blood Cell Transfusion
- Patient Blood Management in Hip Replacement Arthroplasty
- Improvement of Transfusion Practice in Cardiothoracic Surgery Through Implementing a Patient Blood Management Program
- Developing a Data Visualization Program for Transfusion Appropriateness Management
- Experience in Establishing Department of Transfusion Management