J Yeungnam Med Sci.
2023 Jan;40(1):96-101. 10.12701/jyms.2022.00234.
The endoscopic transnasal approach to the lesions of the craniocervical junction: two case reports
- Affiliations
-
- 1Department of Neurosurgery, Faculty of Medicine, Lebanese University, Beirut, Lebanon
- 2Department of Neurosurgery, AP-HP, Henri Mondor Hospital, Créteil, France
- KMID: 2538791
- DOI: http://doi.org/10.12701/jyms.2022.00234
Abstract
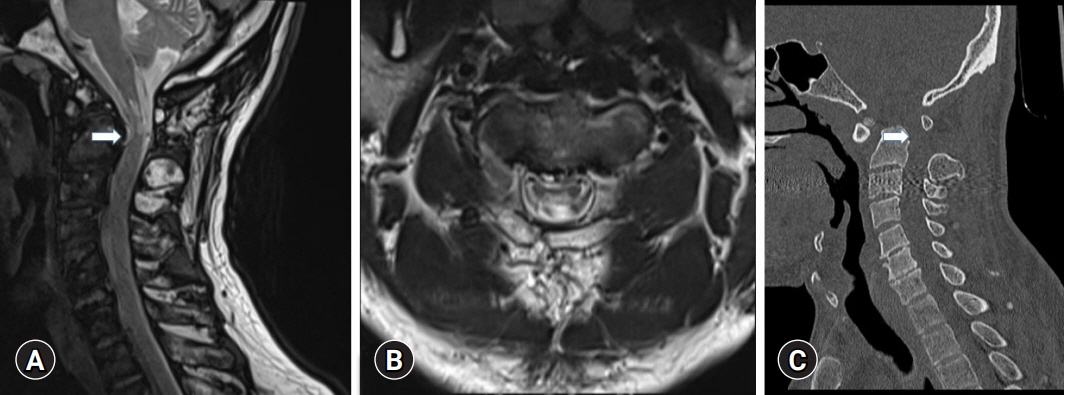
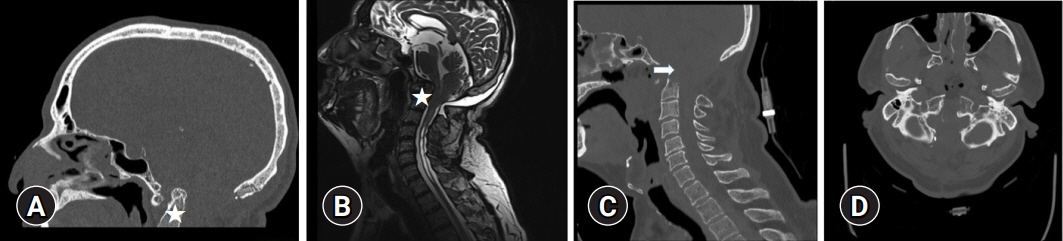
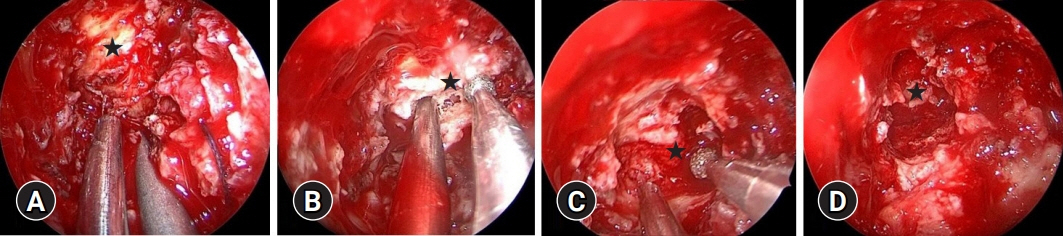
- The endoscopic endonasal approach (EEA) to the craniovertebral junction (CVJ) has recently been considered a safer alternative and less invasive approach than the traditional transoral approach because the complications associated with the latter are avoided or minimized. Here, we present two challenging cases of CVJ pathologies. The first case involved os odontoideum associated with anterior displacement of the occipitocervical junction where the EEA was used, followed by C0-C1-C2 fusion using a posterior approach to decompress the CVJ, and was complicated by rhinorrhea and Candida albicans meningitis. The second case involved basilar invagination with syringomyelia previously treated using a posterior approach, where aggravation of neuropathic symptoms required combined treatment with EEA and occipitocervical fusion of C0-C2-C3-C4, with the postoperative course challenged by operative site infection requiring drainage with debridement and antibiotic therapy. The EEA is an alternative approach for accessing the CVJ in well-selected patients. Knowledge of EEA complications is crucial for the optimal care of patients.
Figure
Reference
-
References
1. Hong JT, Kim IS, Lee HJ, Park JH, Hur JW, Lee JB, et al. Evaluation and surgical planning for craniovertebral junction deformity. Neurospine. 2020; 17:554–67.2. Frempong-Boadu AK, Faunce WA, Fessler RG. Endoscopically assisted transoral-transpharyngeal approach to the craniovertebral junction. Neurosurgery. 2002; 51(5 Suppl):S60–6.3. Mummaneni PV, Haid RW. Transoral odontoidectomy. Neurosurgery. 2005; 56:1045–50.4. Shaha AR, Johnson R, Miller J, Milhorat T. Transoral-transpharyngeal approach to the upper cervical vertebrae. Am J Surg. 1993; 166:336–40.5. Silveira-Bertazzo G, Manjila S, London NR Jr, Prevedello DM. Focused endoscopic endonasal craniocervical junction approach for resection of retro-odontoid lesions: surgical techniques and nuances. Acta Neurochir (Wien). 2020; 162:1275–80.6. Grose E, Moldovan ID, Kilty S, Agbi C, Lamothe A, Alkherayf F. Clinical outcomes of endoscopic endonasal odontoidectomy: a single-center experience. World Neurosurg. 2020; 137:e406–15.7. Signorelli F, Olivi A, De Giorgio F, Pascali VL, Visocchi M. A 360° approach to the craniovertebral junction in a cadaveric laboratory setting: historical insights, current, and future perspectives in a comparative study. World Neurosurg. 2020; 140:564–73.8. Visocchi M, Signorelli F, Liao C, Rigante M, Ciappetta P, Barbagallo G, et al. Transoral versus transnasal approach for craniovertebral junction pathologies: which route is better? Acta Neurochir Suppl. 2019; 125:181–6.9. Crockard HA. Transoral surgery: some lessons learned. Br J Neurosurg. 1995; 9:283–93.10. Alfieri A, Jho HD, Tschabitscher M. Endoscopic endonasal approach to the ventral cranio-cervical junction: anatomical study. Acta Neurochir (Wien). 2002; 144:219–25.11. Kassam AB, Snyderman C, Gardner P, Carrau R, Spiro R. The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process: technical case report. Neurosurgery. 2005; 57(1 Suppl):E213.12. Nayak JV, Gardner PA, Vescan AD, Carrau RL, Kassam AB, Snyderman CH. Experience with the expanded endonasal approach for resection of the odontoid process in rheumatoid disease. Am J Rhinol. 2007; 21:601–6.13. Shkarubo AN, Chernov I, Andreev DN, Nikolenko VN, Chmutin KG, Sinelnikov MY. Expanded endoscopic transnasal odontoidectomy and posterior stabilization: a combined approach. J Neurosurg Sci. 2022; 66:551–9.14. Yu Y, Wang X, Zhang X, Hu F, Gu Y, Xie T, et al. Endoscopic transnasal odontoidectomy to treat basilar invagination with congenital osseous malformations. Eur Spine J. 2013; 22:1127–36.15. Visocchi M, Iacopino DG, Signorelli F, Olivi A, Maugeri R. Walk the line: the surgical highways to the craniovertebral junction in endoscopic approaches: a historical perspective. World Neurosurg. 2018; 110:544–57.16. Shriver MF, Kshettry VR, Sindwani R, Woodard T, Benzel EC, Recinos PF. Transoral and transnasal odontoidectomy complications: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2016; 148:121–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Craniocervical Junctional Neurenteric Cyst
- Long-Term Outcomes of Transnasal Endoscopic Marsupialization through Middle, Inferior Meatal Antrostomy or Extended Middle Meatal Antrostomy in Maxillary Sinus Mucoceles
- Clinical and anatomical importance of foramen magnum and craniocervical junction structures in the perspective of surgical approaches
- Transnasal Endoscopic Resection of Juvenile Nasopharyngeal Angiofibroma: A Case Report
- Clinical Analysis of Endoscopic Transnasal Transsphenoidal Hypophysectomy of Pituitary Tumor