Lab Med Online.
2022 Jul;12(3):195-200. 10.47429/lmo.2022.12.3.195.
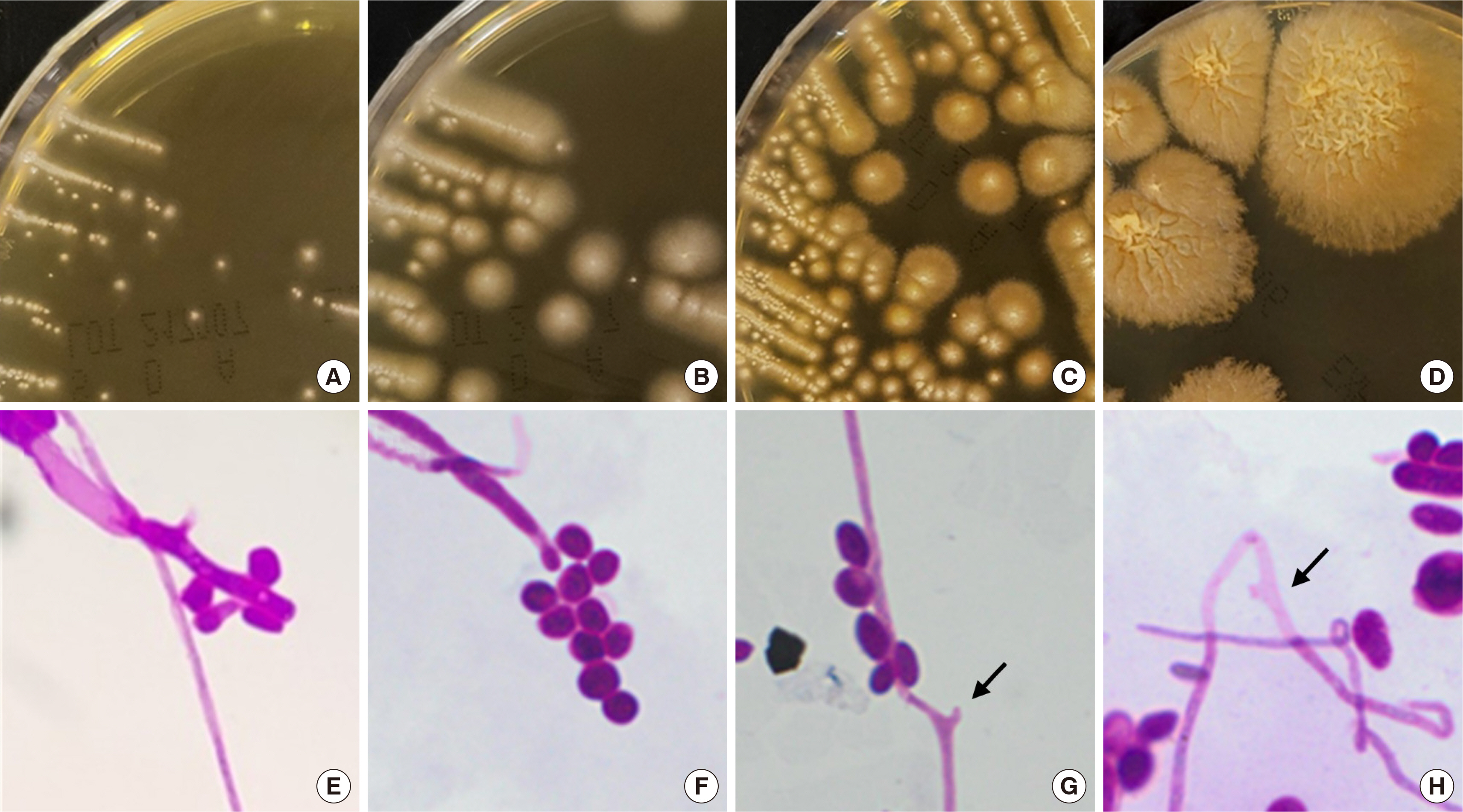
The First Case of Coniochaeta hoffmannii Fungemia and Literature Review
- Affiliations
-
- 1Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2538605
- DOI: http://doi.org/10.47429/lmo.2022.12.3.195
Abstract
- Coniochaeta hoffmannii (formerly, Lecythophora hoffmannii) is a soil-inhabiting plant pathogen in the class of Sordariomycetes. Coniochaeta species are rare and opportunistic and cause subcutaneous infections, keratitis, sinusitis, and peritonitis. Only three cases of human infection by C. hoffmannii have been reported worldwide. A 61-year-old woman with advanced endometrioid adenocarcinoma developed a fever of 39.2°C. Her chest computed tomography (CT) revealed multiple irregular nodules in both lungs, suggesting septic embolism, fungal infection, or less likely, metastasis. Blood cultures performed using a set of blood samples drawn from the central venous catheter showed the presence of Clostridium baratii and C. hoffmannii. Ceftriaxone was administered for 2 days and piperacillin-tazobactam was administered for 6 days after removing the central line. Her fever subsided the next day after febrile onset. Cultures obtained from the central line tip showed no growth. The follow-up CT performed two months later revealed variable changes in the size of the previous nodules and multiple new nodules accompanying the inflammatory lesions. The central venous catheter or pulmonary fungal infections are the suspected source of this rare case of fungemia; this represents the first reported case of C. hoffmannii fungemia.
Figure
Reference
-
1. Khan Z, Gené J, Ahmad S, Cano J, Al-Sweih N, Joseph L, et al. 2013; Coniochaeta polymorpha, a new species from endotracheal aspirate of a preterm neonate, and transfer of Lecythophora species to Coniochaeta. Antonie Van Leeuwenhoek. 104:243–52. DOI: 10.1007/s10482-013-9943-z. PMID: 23748934.
Article2. Larone DH. 2002. Medically important fungi: a guide to identification. 4th ed. Washington, D.C.: ASM Press.3. Perdomo H, Sutton DA, García D, Fothergill AW, Gené J, Cano J, et al. 2011; Molecular and phenotypic characterization of Phialemonium and Lecythophora isolates from clinical samples. J Clin Microbiol. 49:1209–16. DOI: 10.1128/JCM.01979-10. PMID: 21270235. PMCID: PMC3122869.
Article4. Drees M, Wickes BL, Gupta M, Hadley S. 2007; Lecythophora mutabilis prosthetic valve endocarditis in a diabetic patient. Med Mycol. 45:463–7. DOI: 10.1080/13693780701386007. PMID: 17654274.
Article5. Scott IU, Cruz-Villegas V, Flynn HW Jr, Miller D. 2004; Delayed-onset, bleb-associated endophthalmitis caused by Lecythophora mutabilis. Am J Ophthalmol. 137:583–5. DOI: 10.1016/j.ajo.2003.08.037. PMID: 15013895.
Article6. Taniguchi Y, Taketani T, Moriyama H, Moriki S, Nishimura K, Sato E, et al. 2009; Septic shock induced by Lecythophora mutabilis in a patient with mitochondrial encephalomyopathy. J Med Microbiol. 58:1255–8. DOI: 10.1099/jmm.0.010678-0. PMID: 19528157.
Article7. Chang CY, Schell WA, Perfect JR, Hulka GF. 2005; Novel use of a swimming pool biocide in the treatment of a rare fungal mastoiditis. Laryngoscope. 115:1065–9. DOI: 10.1097/01.MLG.0000163338.45700.FE. PMID: 15933522.
Article8. Marriott DJ, Wong KH, Aznar E, Harkness JL, Cooper DA, Muir D. 1997; Scytalidium dimidiatum and Lecythophora hoffmannii: unusual causes of fungal infections in a patient with AIDS. J Clin Microbiol. 35:2949–52. DOI: 10.1128/jcm.35.11.2949-2952.1997. PMID: 9350765. PMCID: PMC230093.
Article9. Rinaldi MG, McCoy EL, Winn DF. 1982; Gluteal abscess caused by Phialophora hoffmannii and review of the role of this organism in human mycoses. J Clin Microbiol. 16:181–5. DOI: 10.1128/jcm.16.1.181-185.1982. PMID: 7107854. PMCID: PMC272316.
Article10. Ahmad S, Johnson RJ, Hillier S, Shelton WR, Rinaldi MG. 1985; Fungal peritonitis caused by Lecythophora mutabilis. J Clin Microbiol. 22:182–6. DOI: 10.1128/jcm.22.2.182-186.1985. PMID: 4031032. PMCID: PMC268355.
Article11. Fintelmann RE, Gilmer W, Bloomer MM, Jeng BH. 2011; Recurrent Lecytho-phora mutabilis keratitis and endophthalmitis after deep anterior lamellar keratoplasty. Arch Ophthalmol. 129:108–10. DOI: 10.1001/archophthalmol.2010.335. PMID: 21220641.
Article12. Pierach CA, Gülmen G, Dhar GJ, Kiser JC. 1973; Letter: Phialophora mutabilis endocarditis. Ann Intern Med. 79:900–1. DOI: 10.7326/0003-4819-79-6-900_2. PMID: 4796911.13. Slifkin M, Bowers HM Jr. 1975; Phialophora mutabilis endocarditis. Am J Clin Pathol. 63:120–30. DOI: 10.1093/ajcp/63.3.120. PMID: 803342.14. Ho RH, Bernard PJ, McClellan KA. 1991; Phialophora mutabilis keratomycosis. Am J Ophthalmol. 112:728–9. DOI: 10.1016/S0002-9394(14)77283-6.
Article15. Marcus DM, Hull DS, Rubin RM, Newman CL. 1999; Lecythophora mutabilis endophthalmitis after long-term corneal cyanoacrylate. Retina. 19:351–3. DOI: 10.1097/00006982-199919040-00018. PMID: 10458306.
Article16. Castro LL, Schütze M, Bücker DH, Vasconcellos Lde S. 2016; Prevalence of fungemia in a tertiary hospital: Analysis of the last decade. Rev Assoc Med Bras (1992). 62:315–9. DOI: 10.1590/1806-9282.62.04.315. PMID: 27437675.
Article17. Singhal N, Kumar M, Kanaujia PK, Virdi JS. 2015; MALDI-TOF mass spectrometry: an emerging technology for microbial identification and diagnosis. Front Microbiol. 6:791. DOI: 10.3389/fmicb.2015.00791. PMID: 26300860. PMCID: PMC4525378.
Article18. Usyk M, Zolnik CP, Patel H, Levi MH, Burk RD. 2017; Novel ITS1 Fungal Primers for characterization of the mycobiome. mSphere. 2:e00488–17. DOI: 10.1128/mSphere.00488-17. PMID: 29242834. PMCID: PMC5729218.
Article19. Rechner PM, Agger WA, Mruz K, Cogbill TH. 2001; Clinical features of clostridial bacteremia: a review from a rural area. Clin Infect Dis. 33:349–53. DOI: 10.1086/321883. PMID: 11438901.
Article20. Iaria C, Stassi G, Salpietro DC, La Mazza A, Silipigni L, Arena A, et al. 2007; Clostridium baratii bacteremia associated with Kawasaki syndrome. First case report. New Microbiol. 30:481–4.21. Peleg AY, Hogan DA, Mylonakis E. 2010; Medically important bacterial-fungal interactions. Nat Rev Microbiol. 8:340–9. DOI: 10.1038/nrmicro2313. PMID: 20348933.
Article22. Heydari S, Siavoshi F, Sarrafnejad A, Malekzadeh R. 2021; Coniochaeta fungus benefits from its intracellular bacteria to form biofilm and defend against other fungi. Arch Microbiol. 203:1357–66. DOI: 10.1007/s00203-020-02122-4. PMID: 33386870.
Article23. Donelli G, Vuotto C, Cardines R, Mastrantonio P. 2012; Biofilm-growing intestinal anaerobic bacteria. FEMS Immunol Med Microbiol. 65:318–25. DOI: 10.1111/j.1574-695X.2012.00962.x. PMID: 22444687.
Article24. Krcmery V, Barnes AJ. 2002; Non-albicans Candida spp. causing fungaemia: pathogenicity and antifungal resistance. J Hosp Infect. 50:243–60. DOI: 10.1053/jhin.2001.1151. PMID: 12014897.25. McPherson RA, Pincus MR, editors. 2017. Henry's clinical diagnosis and management by laboratory methods. 23rd ed. St. Louis, MO: Elsevier.26. Hall-Stoodley L, Stoodley P, Kathju S, Høiby N, Moser C, Costerton JW, et al. 2012; Towards diagnostic guidelines for biofilm-associated infections. FEMS Immunol Med Microbiol. 65:127–45. DOI: 10.1111/j.1574-695X.2012.00968.x. PMID: 22469292.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hansenule anomala fungemia: a case report and a review of theliterature
- Kodamaea ohmeri Fungemia Associated with Colonoscopic Stent Insertion: A Case Report
- Two Cases of Pichia Ohmeri Fungemia
- A case of Yarrowia lipolytica fungemia after raw beef ingestion
- A Case of Fungemia due to Rhodotorula Glutinis with Liver Cirrhosis