J Korean Med Sci.
2023 Jan;38(3):e18. 10.3346/jkms.2023.38.e18.
The Impact of Omicron Wave on Pediatric Febrile Seizure
- Affiliations
-
- 1Department of Emergency Medicine, Ajou University School of Medicine, Suwon, Korea
- KMID: 2538372
- DOI: http://doi.org/10.3346/jkms.2023.38.e18
Abstract
- Background
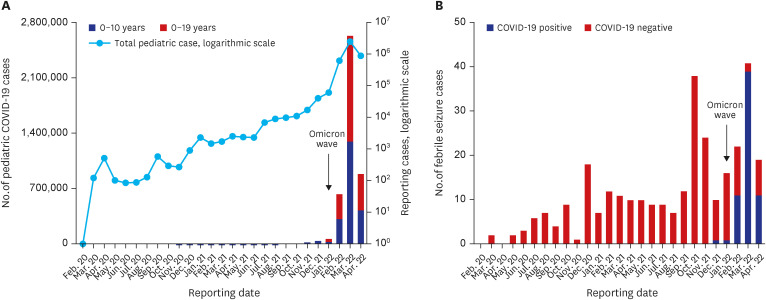
The coronavirus disease 2019 (COVID-19) omicron (B.1.1.529) variant reduced the risk of severe disease compared with the original strain and other variants, but it appeared to be highly infectious, which resulted in an exponential increase in confirmed cases in South Korea. As the number of confirmed cases increased, so did the number of pediatric patients’ hospitalization. This study aims to evaluate the frequency and clinical features of febrile seizure associated with the COVID-19 omicron variant in children.
Methods
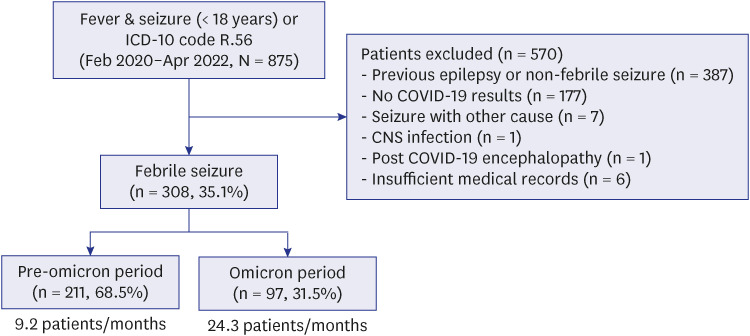
We retrospectively reviewed the medical records of children aged under 18 years with febrile seizure who were tested for COVID-19 from February 2020 to April 2022 at Ajou University Hospital, South Korea. Based on the dominant variants, we divided the period into the pre-omicron (from February 2020 to December 2021) and omicron periods (from January 2022 to April 2022) and compared the clinical characteristics between the two. Also, we compared the clinical characteristics of febrile seizure between COVID-19 positive and negative group during the omicron period.
Results
Among the 308 children, 211 patients (9.2 patients/months) and 97 patients (24.3 patients/months) were grouped into pre-omicron and omicron periods, respectively. Compared with the pre-omicron period, patients in the omicron period showed significantly higher mean age (pre-omicron vs. omicron, 22.0 vs. 28.0 months; P = 0.004) and COVID-19 positive results (pre-omicron vs. omicron, 0.5% vs. 62.9%; P < 0.001). As the COVID-19 confirmed cases in the omicron period increased, the number of COVID-19 associated febrile seizure also increased. In the omicron period, 61 children were confirmed to be positive for COVID-19, and COVID-19 positive group showed statistically significant higher mean age (positive vs. negative, 33.0 vs. 23.0 months; P= 0.003) and peak body temperature than the negative group (positive vs. negative, 39.1°C vs. 38.6°C; P = 0.030). Despite the lack of significance, COVID-19 positive group showed longer seizure time, multiple seizure episodes, and higher prevalence of complex febrile seizure.
Conclusion
The frequency of COVID-19 associated febrile seizure increased in the omicron periods. In addition, in this period, children with febrile seizure diagnosed with COVID-19 had a higher mean age and higher peak body temperature.
Figure
Reference
-
1. Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020; 109(6):1088–1095. PMID: 32202343.2. Cloete J, Kruger A, Masha M, du Plessis NM, Mawela D, Tshukudu M, et al. Rapid rise in paediatric COVID-19 hospitalisations during the early stages of the omicron wave, Tshwane District, South Africa. medRxiv. 2021. 12. 21. DOI: 10.1101/2021.12.21.21268108.3. Choi YY, Kim YS, Lee SY, Sim J, Choe YJ, Han MS. Croup as a manifestation of SARS-CoV-2 omicron variant infection in young children. J Korean Med Sci. 2022; 37(20):e140. PMID: 35607737.4. Sawires R, Buttery J, Fahey M. A review of febrile seizures: recent advances in understanding of febrile seizure pathophysiology and commonly implicated viral triggers. Front Pediatr. 2022; 9:801321. PMID: 35096712.5. Ludvigsson JF. Convulsions in children with COVID-19 during the omicron wave. Acta Paediatr. 2022; 111(5):1023–1026. PMID: 35098577.6. Cadet K, Boegner J, Ceneviva GD, Thomas NJ, Krawiec C. Evaluation of febrile seizure diagnoses associated with COVID-19. J Child Neurol. 2022; 37(5):410–415. PMID: 35286175.7. Chiu TG, Leung WC, Zhang Q, Lau EH, Ho RW, Chan HS, et al. Changes in pediatric seizure-related emergency department attendances during COVID-19 - a territory-wide observational study. J Formos Med Assoc. 2021; 120(8):1647–1651. PMID: 33248859.8. Tintinalli J, Ma OJ, Yealy D, Meckler G, Stapczynski J, Cline D, et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. New York, NY, USA: McGraw-Hill Education;2019.9. Kim JY, Ko JH, Kim Y, Kim YJ, Kim JM, Chung YS, et al. Viral load kinetics of SARS-CoV-2 infection in first two patients in Korea. J Korean Med Sci. 2020; 35(7):e86. PMID: 32080991.10. Park JY, Han MS, Park KU, Kim JY, Choi EH. First pediatric case of coronavirus disease 2019 in Korea. J Korean Med Sci. 2020; 35(11):e124. PMID: 32193905.11. Shin DH, Jang H, Lee S, Choi BS, Kim D, Oh HS. Trends in confirmed COVID-19 cases in the Korean military before and after the emergence of the omicron variant. J Korean Med Sci. 2022; 37(34):e260. PMID: 36038957.12. Yun HE, Ryu BY, Choe YJ. Impact of social distancing on incidence of vaccine-preventable diseases, South Korea. J Med Virol. 2021; 93(3):1814–1816. PMID: 33079384.13. Park KH, Choe YJ, Shim Y, Eun BL, Byeon JH. Decrease in incidence of febrile seizure following social distancing measures: a national cohort study in South Korea. Pediatr Infect Vaccine. 2021; 28(3):144.14. Misra S, Kolappa K, Prasad M, Radhakrishnan D, Thakur KT, Solomon T, et al. Frequency of neurologic manifestations in COVID-19: a systematic review and meta-analysis. Neurology. 2021; 97(23):e2269–e2281. PMID: 34635561.15. Cloete J, Kruger A, Masha M, du Plessis NM, Mawela D, Tshukudu M, et al. Paediatric hospitalisations due to COVID-19 during the first SARS-CoV-2 omicron (B.1.1.529) variant wave in South Africa: a multicentre observational study. Lancet Child Adolesc Health. 2022; 6(5):294–302. PMID: 35189083.16. van Zeijl JH, Mullaart RA, Borm GF, Galama JM. Recurrence of febrile seizures in the respiratory season is associated with influenza A. J Pediatr. 2004; 145(6):800–805. PMID: 15580205.17. Christy A. COVID-19: a review for the pediatric neurologist. J Child Neurol. 2020; 35(13):934–939. PMID: 32660309.18. Mikkonen K, Uhari M, Pokka T, Rantala H. Diurnal and seasonal occurrence of febrile seizures. Pediatr Neurol. 2015; 52(4):424–427. PMID: 25682483.19. Han DH, Kim SY, Lee NM, Yi DY, Yun SW, Lim IS, et al. Seasonal distribution of febrile seizure and the relationship with respiratory and enteric viruses in Korean children based on nationwide registry data. Seizure. 2019; 73:9–13. PMID: 31675516.20. Esmaili Gourabi H, Bidabadi E, Cheraghalipour F, Aarabi Y, Salamat F. Febrile seizure: demographic features and causative factors. Iran J Child Neurol. 2012; 6(4):33–37.21. Brewster RC, Parsons C, Laird-Gion J, Hilker S, Irwin M, Sommerschield A, et al. COVID-19-associated croup in children. Pediatrics. 2022; 149(6):e2022056492. PMID: 35257175.22. Francis JR, Richmond P, Robins C, Lindsay K, Levy A, Effler PV, et al. An observational study of febrile seizures: the importance of viral infection and immunization. BMC Pediatr. 2016; 16(1):202. PMID: 27914475.23. Verity CM, Golding J. Risk of epilepsy after febrile convulsions: a national cohort study. BMJ. 1991; 303(6814):1373–1376. PMID: 1760604.24. Lin JE, Asfour A, Sewell TB, Hooe B, Pryce P, Earley C, et al. Neurological issues in children with COVID-19. Neurosci Lett. 2021; 743:135567. PMID: 33352286.25. Asadi-Pooya AA. Seizures associated with coronavirus infections. Seizure. 2020; 79:49–52. PMID: 32416567.26. Narula N, Joseph R, Katyal N, Daouk A, Acharya S, Avula A, et al. Seizure and COVID-19: association and review of potential mechanism. Neurol Psychiatry Brain Res. 2020; 38:49–53. PMID: 33071468.27. Dantzer R. Neuroimmune interactions: from the brain to the immune system and vice versa. Physiol Rev. 2018; 98(1):477–504. PMID: 29351513.28. Rana A, Musto AE. The role of inflammation in the development of epilepsy. J Neuroinflammation. 2018; 15(1):144. PMID: 29764485.29. Erdő F, Denes L, de Lange E. Age-associated physiological and pathological changes at the blood-brain barrier: a review. J Cereb Blood Flow Metab. 2017; 37(1):4–24. PMID: 27837191.30. LaRovere KL, Riggs BJ, Poussaint TY, Young CC, Newhams MM, Maamari M, et al. Neurologic involvement in children and adolescents hospitalized in the United States for COVID-19 or multisystem inflammatory syndrome. JAMA Neurol. 2021; 78(5):536–547. PMID: 33666649.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Seizure Incidence among Children Hospitalized with COVID-19 during the Omicron Wave
- A Clinicoelectroencephalographic Study of Febrile Convulsion and Epilepsy in Childhood
- Analysis of Inflammatory Markers and Electroencephalogram Findings in Pediatric Patients with COVID-19: A Single-Center Study in Korea
- The Optimum Dose of Oral Diazepam to Reduce Seizure Attack in Febrile Seizure Patients During Febrile Illness
- Selection of High Risk Group According to Risk Factors of Recurrent Febrile Seizures