Pediatr Emerg Med J.
2023 Jan;10(1):3-10. 10.22470/pemj.2022.00598.
The pattern of mortality among children hospitalized in the children emergency ward of a single tertiary hospital in Nigeria
- Affiliations
-
- 1Department of Paediatrics and Child Health, College of Medical Sciences, Rivers State University/Rivers State University Teaching Hospital, Port Harcourt, Nigeria
- 2Department of Paediatrics, College of Health Sciences, University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria
- KMID: 2538076
- DOI: http://doi.org/10.22470/pemj.2022.00598
Abstract
- Purpose
This study was performed to review the mortality pattern at the emergency ward (EW) of the Rivers State University Teaching Hospital, Port Harcourt, Nigeria.
Methods
A retrospective review of mortality among children hospitalized in the EW was conducted from January 2015 through May 2017. Information on their age, sex, weight, diagnosis, and mortality was recorded. The data were expressed in frequencies, and logistic regressions were performed with mortality as the dependent variable.
Results
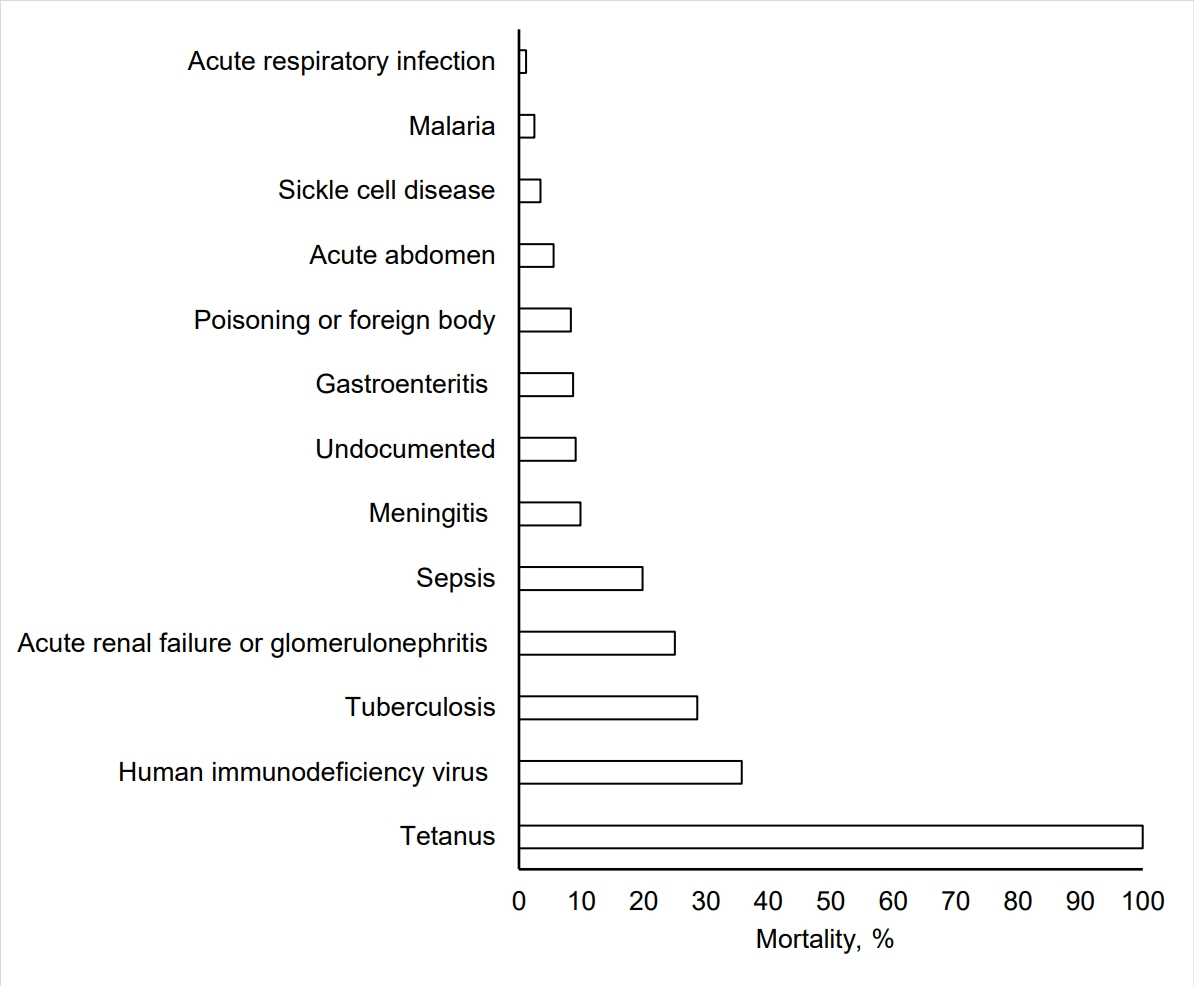
The median age of the 1,020 children hospitalized in the EW was 1.0 year (interquartile range, 0.6-4.0) with death recorded in 60 children, a 5.9% mortality rate. Mortality was higher in the children younger than 2 years, boys, and those with infectious diseases. Of the 60 dead children, infectious diseases were the leading cause of mortality (53 [88.3%]) with sepsis (22 [36.7%]), gastroenteritis (10 [16.7%]), and meningitis (6 [10.0%]), accounting for the highest contributors to mortality. The highest case fatality rates were noted in tetanus (1/1 [100%]), human immunodeficiency virus (5/14 [35.7%]), and tuberculosis (2/7 [28.6%]). The logistic regression showed that age of 13-16 years (adjusted odds ratio, 4.59; 95% confidence interval, 1.80-11.20; compared with age < 2 years) and presence of infectious diseases (4.65; 1.80-12.10) significantly increased the risk of mortality.
Conclusion
The mortality rate in our EW during the study period was 5.9%. Infectious diseases remained significant contributors to mortality in our practice. Greater efforts at prevention and control of the diseases are required to correct this negative trend.
Keyword
Figure
Reference
-
References
1. World Health Organization (WHO). The global health observatory. Child mortality and causes of death [Internet]. Geneva: WHO;c2022 [cited 2022 Jun 13]. Available from: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/child-mortality-and-causes-of-death.2. Whitehead PR. The lived experience of physicians dealing with patient death. BMJ Support Palliat Care. 2014; 4:271–6.3. Zhu CP, Wu XH, Liang YT, Ma WC, Ren L. The mortality of patients in a pediatric emergency department at a tertiary medical center in China: an observational study. World J Emerg Med. 2015; 6:212–6.4. Lopez E, Udaondo J, Olabarri M, Martinez-Indart L, Benito J, Mintegi S, et al. Mortality in Spanish pediatric emergency departments: a 5-year multicenter survey. Eur J Emerg Med. 2017; 24:392–7.5. Tette EMA, Nyarko MY, Nartey ET, Neizer ML, Egbefome A, Akosa F, et al. Under-five mortality pattern and associated risk factors: a case-control study at the Princess Marie Louise Children’s Hospital in Accra, Ghana. BMC Pediatr. 2016; 16:148.6. Jofiro G, Jemal K, Beza L, Bacha Heye T. Prevalence and associated factors of pediatric emergency mortality at Tikur Anbessa specialized tertiary hospital: a 5 year retrospective case review study. BMC Pediatr. 2018; 18:316.7. Edelu BO, Eze JN, Oguonu T, Ndu IK. Morbidity and mortality pattern in the children emergency unit of the University of Nigeria Teaching Hospital Enugu. Orient J Med. 2014; 26:73–8.8. Enyuma CO, Ikpeme OE, Brown-Abang E, Uket H. Morbidity and mortality pattern in a children emergency room in Calabar, Nigeria. J Med Africa. 2016; 1:6–10.9. Onyearugha CN, Okoronkwo NC, Onyemachi PE. Mortality pattern in children aged 1-60 months at a tertiary healthcare institution, in Southeast Nigeria. Ann Med Health Sci Res. 2020; 10:907–11.10. Ibeziako SN, Ibekwe RC. Pattern and outcome of admissions in the children’s emergency room of the University of Nigeria Teaching Hospital, Enugu. Niger J Paed. 2002; 29:103–7.11. Njoku PU, Iloh GU, Dienye PO, Korie FC, Ahaiwe VC. Pattern of paediatric conditions seen in the children emergency room of an urban hospital in South-Eastern Nigeria. GSC Biol Pharm Sci. 2020; 13:174–80.12. Singhi S, Jain V, Gupta G. Pediatric emergencies at a tertiary care hospital in India. J Trop Pediatr. 2003; 49:207–11.13. Brugnolaro V, Fovino LN, Calgaro S, Putoto G, Muhelo AR, Gregori D, et al. Pediatric emergency care in a low-income country: characteristics and outcomes of presentations to a tertiary-care emergency department in Mozambique. PLoS One. 2020; 15:e0241209.14. Duru C, Peterside O, Akinbami F. Pattern and outcome of admissions as seen in the paediatric emergency ward of the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. Niger J Paed. 2013; 40:232–7.15. Okoronkwo NC, ChappJumbo AU. Pattern of morbidity and mortality of childhood illnesses at the children emergency room of Abia State University Teaching Hospital, Aba, Nigeria. East Central Afr Med J. 2015; 2:70–3.16. Sa’ad YM, Hayatu A, Al-Mustapha II, Orahachi YM, Hauwa MU. Morbidity and mortality of childhood illnesses at the emergency pediatric unit of a tertiary hospital, north-eastern Nigeria. Sahel Med J. 2015; 18:1–3.17. Molyneux EM. Paediatric emergency care in resource-constrained health services is usually neglected: time for change. Ann Trop Paediatr. 2010; 30:165–76.18. Ndukwu CI, Onah SK. Pattern and outcome of postneonatal pediatric emergencies in Nnamdi Azikiwe University Teaching Hospital, Nnewi, South East Nigeria. Niger J Clin Pract. 2015; 18:348–53.19. Ibeneme CA, Ezuruike EO, Korie FC, Chukwudi NK, Ukpabi IK. Morbidity pattern and outcome among under-fives at the children’s emergency room of Federal Medical Center Umuahia. Niger J Paediatr. 2019; 46:189–94.20. Kingwengwe AA, Ndgadi AK, Lukusa PM, Ilunga PM, Ibeki EK, Kyanga PA, et al. Epidemiology of pediatric medical emergencies at the Kindu reference General Hospital (HGRK): state of affairs and perspectives. Open Access Libr J. 2019; 6:e5715.21. World Health Organization (WHO). Children: improving survival and well-being 2020 [Internet]. Geneva: WHO;2020. [cited 2022 April 3]. Available from: https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality.22. World Health Organization (WHO). Mortality among children aged 5-14 years. Geneva: WHO;2019. [cited 2022 July 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/mortality-among-children-aged-5-14-years.23. Mathers C. Deaths of older children: what do the data tell us? Lancet Glob Health. 2015; 3:e579–80.24. Ngwalangwa F, Phiri CHA, Dube Q, Langton J, Hildenwall H, Baker T. Risk factors for mortality in severely ill children admitted to a tertiary referral hospital in Malawi. Am J Trop Med Hyg. 2019; 101:670–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of children hospitalized through the pediatric emergency department and effects of pediatric emergency ward hospitalization
- Correlation between the occurrence of acute gastroenteritis in children and regional temperature at a tertiary hospital emergency department in Korea
- Studies on the General Fearfulness of Hospitalized School - Age Children and Their Mother's Emotional Anxiety
- Effects of Anxiety, Parenting Efficacy, and Partnership With Nurses on the Caring Behaviors of Mothers of Hospitalized Children
- Blood culture contamination in hospitalized pediatric patients: a single institution experience