Cancer Res Treat.
2023 Jan;55(1):41-49. 10.4143/crt.2021.1514.
Suggestions for Escaping the Dark Ages for Pediatric Diffuse Intrinsic Pontine Glioma Treated with Radiotherapy: Analysis of Prognostic Factors from the National Multicenter Study
- Affiliations
-
- 1Department of Radiation Oncology, Gachon University Gil Hospital, Incheon, Korea
- 2Department of Radiation Oncology, Seoul National University Hospital, Seoul National University, College of Medicine, Seoul, Korea
- 3Department of Radiation Oncology, Kyung Hee University Medical Center, Kyung Hee University School of Medicine, Seoul, Korea
- 4Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Department of Radiation Oncology, School of Medicine, Kyungpook National University, Daegu, Korea
- 6Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 7Department of Radiation Oncology, Seoul National University Bundang Hospital, Seongnam, Korea
- 8Department of Radiation Oncology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 9Department of Radiation Oncology, Chonnam National University Medical School, Gwangju, Korea
- 10Proton Therapy Center, National Cancer Center, Goyang, Korea
- 11Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2537990
- DOI: http://doi.org/10.4143/crt.2021.1514
Abstract
- Purpose
This multicenter retrospective study aimed to investigate clinical, radiologic, and treatment-related factors affecting survival in patients with newly diagnosed diffuse intrinsic pontine glioma (DIPG) treated with radiotherapy.
Materials and Methods
Patients aged <30 years who underwent radiotherapy as an initial treatment for DIPG between 2000 and 2018 were included; patients who did not undergo magnetic resonance imaging at diagnosis and those with pathologically diagnosed grade I glioma were excluded. We examined medical records of 162 patients collected from 10 participating centers in Korea. The patients’ clinical, radiological, molecular, and histopathologic characteristics, and treatment responses were evaluated to identify the prognosticators for DIPG and estimate survival outcomes.
Results
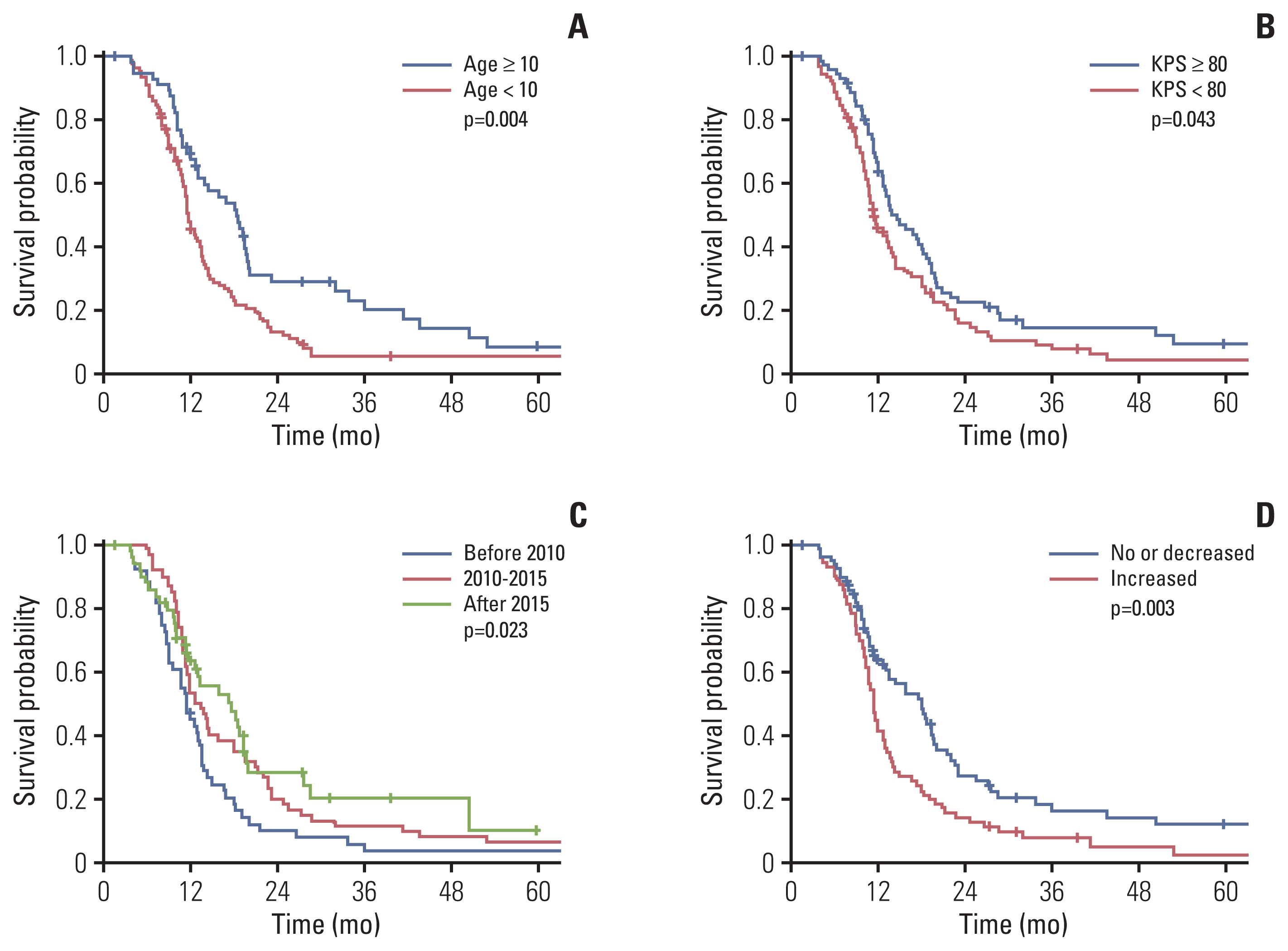
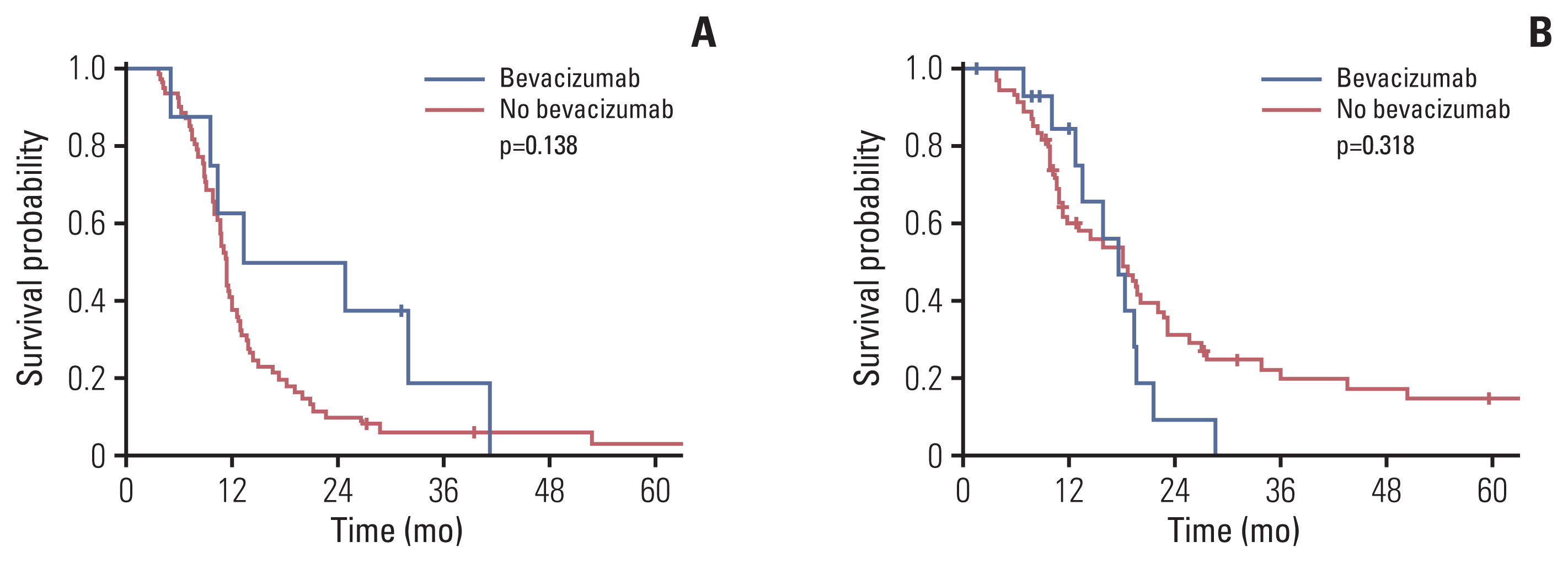
The median follow-up period was 10.8 months (interquartile range, 7.5 to 18.1). The 1- and 2-year overall survival (OS) rates were 53.5% and 19.0%, respectively, with a median OS of 13.1 months. Long-term survival rate (≥ 2 years) was 16.7%, and median OS was 43.6 months. Age (< 10 years), poor performance status, treatment before 2010, and post-radiotherapy necrosis were independently associated with poor OS in multivariate analysis. In patients with increased post-radiotherapy necrosis, the median OS estimates were 13.3 months and 11.4 months with and without bevacizumab, respectively (p=0.138).
Conclusion
Therapeutic strategy for DIPG has remained unchanged over time, and the associated prognosis remains poor. Our findings suggest that appropriate efforts are needed to reduce the occurrence of post-radiotherapy necrosis. Further well-designed clinical trials are recommended to improve the poor prognosis observed in DIPG patients.
Figure
Reference
-
References
1. Hoffman LM, Veldhuijzen van Zanten SE, Colditz N, Baugh J, Chaney B, Hoffmann M, et al. Clinical, radiologic, pathologic, and molecular characteristics of long-term survivors of diffuse intrinsic pontine glioma (DIPG): a collaborative report from the International and European Society for Pediatric Oncology DIPG Registries. J Clin Oncol. 2018; 36:1963–72.2. Jackson S, Patay Z, Howarth R, Pai Panandiker AS, Onar-Thomas A, Gajjar A, et al. Clinico-radiologic characteristics of long-term survivors of diffuse intrinsic pontine glioma. J Neurooncol. 2013; 114:339–44.3. Jansen MH, Veldhuijzen van Zanten SE, Sanchez Aliaga E, Heymans MW, Warmuth-Metz M, Hargrave D, et al. Survival prediction model of children with diffuse intrinsic pontine glioma based on clinical and radiological criteria. Neuro Oncol. 2015; 17:160–6.4. Hargrave D, Bartels U, Bouffet E. Diffuse brainstem glioma in children: critical review of clinical trials. Lancet Oncol. 2006; 7:241–8.5. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–20.6. Wu G, Broniscer A, McEachron TA, Lu C, Paugh BS, Becksfort J, et al. Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat Genet. 2012; 44:251–3.7. Langmoen IA, Lundar T, Storm-Mathisen I, Lie SO, Hovind KH. Management of pediatric pontine gliomas. Childs Nerv Syst. 1991; 7:13–5.8. Wagner S, Warmuth-Metz M, Emser A, Gnekow AK, Strater R, Rutkowski S, et al. Treatment options in childhood pontine gliomas. J Neurooncol. 2006; 79:281–7.9. Cohen KJ, Heideman RL, Zhou T, Holmes EJ, Lavey RS, Bouffet E, et al. Temozolomide in the treatment of children with newly diagnosed diffuse intrinsic pontine gliomas: a report from the Children’s Oncology Group. Neuro Oncol. 2011; 13:410–6.10. Cooney TM, Cohen KJ, Guimaraes CV, Dhall G, Leach J, Massimino M, et al. Response assessment in diffuse intrinsic pontine glioma: recommendations from the Response Assessment in Pediatric Neuro-Oncology (RAPNO) working group. Lancet Oncol. 2020; 21:e330–6.11. El-Khouly FE, Veldhuijzen van Zanten SE, Santa-Maria Lopez V, Hendrikse NH, Kaspers GJ, Loizos G, et al. Diagnostics and treatment of diffuse intrinsic pontine glioma: where do we stand? J Neurooncol. 2019; 145:177–84.12. Hassan H, Pinches A, Picton SV, Phillips RS. Survival rates and prognostic predictors of high grade brain stem gliomas in childhood: a systematic review and meta-analysis. J Neurooncol. 2017; 135:13–20.13. Brandel MG, Alattar AA, Hirshman BR, Dong X, Carroll KT, Ali MA, et al. Survival trends of oligodendroglial tumor patients and associated clinical practice patterns: a SEER-based analysis. J Neurooncol. 2017; 133:173–81.14. Tejada S, Aquilina K, Goodden J, Pettorini B, Mallucci C, van Veelen ML, et al. Biopsy in diffuse pontine gliomas: expert neurosurgeon opinion-a survey from the SIOPE brain tumor group. Childs Nerv Syst. 2020; 36:705–11.15. Schwartzentruber J, Korshunov A, Liu XY, Jones DT, Pfaff E, Jacob K, et al. Driver mutations in histone H3.3 and chromatin remodelling genes in paediatric glioblastoma. Nature. 2012; 482:226–31.16. Morales La Madrid A, Hashizume R, Kieran MW. Future clinical trials in DIPG: bringing epigenetics to the clinic. Front Oncol. 2015; 5:148.17. Tam LT, Yeom KW, Wright JN, Jaju A, Radmanesh A, Han M, et al. MRI-based radiomics for prognosis of pediatric diffuse intrinsic pontine glioma: an international study. Neurooncol Adv. 2021; 3:vdab042.18. Leach JL, Roebker J, Schafer A, Baugh J, Chaney B, Fuller C, et al. MR imaging features of diffuse intrinsic pontine glioma and relationship to overall survival: report from the International DIPG Registry. Neuro Oncol. 2020; 22:1647–57.19. Szychot E, Youssef A, Ganeshan B, Endozo R, Hyare H, Gains J, et al. Predicting outcome in childhood diffuse midline gliomas using magnetic resonance imaging based texture analysis. J Neuroradiol. 2021; 48:243–7.20. Hummel TR, Salloum R, Drissi R, Kumar S, Sobo M, Goldman S, et al. A pilot study of bevacizumab-based therapy in patients with newly diagnosed high-grade gliomas and diffuse intrinsic pontine gliomas. J Neurooncol. 2016; 127:53–61.21. Gururangan S, Fangusaro J, Poussaint TY, McLendon RE, Onar-Thomas A, Wu S, et al. Efficacy of bevacizumab plus irinotecan in children with recurrent low-grade gliomas: a Pediatric Brain Tumor Consortium study. Neuro Oncol. 2014; 16:310–7.22. Crotty EE, Leary SE, Geyer JR, Olson JM, Millard NE, Sato AA, et al. Children with DIPG and high-grade glioma treated with temozolomide, irinotecan, and bevacizumab: the Seattle Children’s Hospital experience. J Neurooncol. 2020; 148:607–17.23. Tinkle CL, Simone B, Chiang J, Li X, Campbell K, Han Y, et al. Defining optimal target volumes of conformal radiation therapy for diffuse intrinsic pontine glioma. Int J Radiat Oncol Biol Phys. 2020; 106:838–47.24. Broniscer A, Iacono L, Chintagumpala M, Fouladi M, Wallace D, Bowers DC, et al. Role of temozolomide after radiotherapy for newly diagnosed diffuse brainstem glioma in children: results of a multiinstitutional study (SJHG-98). Cancer. 2005; 103:133–9.25. Jalali R, Raut N, Arora B, Gupta T, Dutta D, Munshi A, et al. Prospective evaluation of radiotherapy with concurrent and adjuvant temozolomide in children with newly diagnosed diffuse intrinsic pontine glioma. Int J Radiat Oncol Biol Phys. 2010; 77:113–8.26. Chassot A, Canale S, Varlet P, Puget S, Roujeau T, Negretti L, et al. Radiotherapy with concurrent and adjuvant temozolomide in children with newly diagnosed diffuse intrinsic pontine glioma. J Neurooncol. 2012; 106:399–407.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiotherapy for Diffuse Intrinsic Pontine Glioma: Insufficient but Indispensable
- Brain Stem Gliomas in Adult: Correlation between MRI, Clinical Findings and Outcome: Preliminary Report
- Fractionated Stereotactic Radiotherapy in Pediatric Diffuse Intrinsic Brain Stem Gliomas
- Spontaneous Regression of Glioma–Mimicking Brainstem Lesion in a Child: A Case Report
- Epigenetic and Metabolic Changes in Diffuse Intrinsic Pontine Glioma