Cardiovasc Prev Pharmacother.
2019 Jul;1(1):30-42. 10.36011/cpp.2019.1.e4.
Aspirin Has a Neutral Effect in Preventing Future Cardiovascular Events in Vasospastic Angina
- Affiliations
-
- 1Department of Cardiovascular Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Cardiovascular Medicine, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Cardiovascular Medicine, Gil Medical Center, Gachon University, Incheon, Korea
- 4Department of Cardiovascular Medicine, Chonnam National University Hospital, Chonnam National University, Gwangju, Korea
- 5Department of Cardiovascular Medicine, Busan Paik Hospital, Inje University, Busan, Korea
- 6Department of Cardiovascular Medicine, Bundang Hospital, Seoul National University, Seongnam, Korea
- 7Department of Cardiovascular Medicine, Gangnam Severance Hospital, Yonsei University, Seoul, Korea
- 8Department of Cardiovascular Medicine, Samsung Medical Center, Sungkyunkwan University, Seoul, Korea
- 9Department of Cardiovascular Medicine, Guro Hospital, Korea University, Seoul, Korea
- 10Department of Cardiovascular Medicine, Pyeongchon Sacred Heart Hospital, Hallym University, Anyang, Korea
- 11Department of Cardiovascular Medicine, College of Pharmacy, The Catholic University of Korea, Bucheon, Korea
- 12Department of Occupational and Environmental Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 13Department of Cardiovascular Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2536961
- DOI: http://doi.org/10.36011/cpp.2019.1.e4
Abstract
- Background
The aim of this multi-center prospective registry study was to evaluate the clinical efficacy of low-dose aspirin in vasospastic angina (VA) patients for the prevention of future cardiovascular events.
Methods
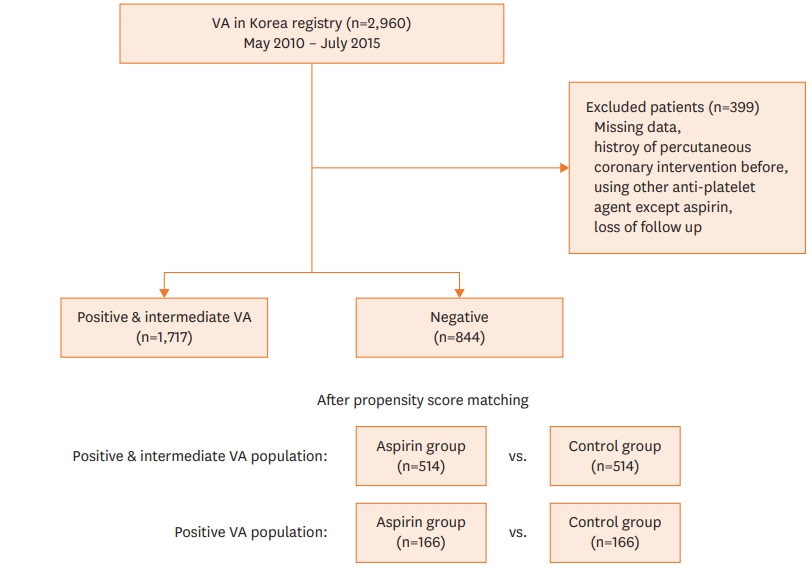
A total of 1,717 patients with positive and intermediate results of an intracoronary ergonovine provocation test in the VA in Korea registry (n=2,960) were classified into 100 mg/day aspirin intake (aspirin, n=743) and no-aspirin intake (control, n=974) groups. The primary end-point was a composite of major adverse cardiac events (MACEs) including cardiac death, new-onset arrhythmia, and acute coronary syndrome.
Results
The median follow-up duration was 2.0 years (25–75th, interquartile range 0.9–3.0 years). Cumulative composite MACE in the propensity score matched-pair cohort (n=1,028) was 3.6%. There was no significant difference in composite MACE between the aspirin and control groups (3.1% vs. 4.1%; hazard ratio [HR], 1.18; 95% confidence interval [CI], 0.61–2.26; p=0.623). A sensitivity analysis of only the VA-positive population showed these results to be consistent. Even for patients with minimal organic stenosis (n=369), aspirin usage was not related to the incidence of a composite MACE (HR, 1.61; 95% CI, 0.55–4.72; p=0.380).
Conclusions
Low-dose aspirin does not protect against future cardiovascular events in VA patients, even patients who combine with minimal coronary artery stenosis.
Figure
Cited by 2 articles
-
Welcome to the New Journal
Cardiovascular Prevention and Pharmacotherapy
Mi-Jeong Kim, Jang-Whan Bae, Dae Ryong Kang
Cardiovasc Prev Pharmacother. 2019;1(1):1-2. doi: 10.36011/cpp.2019.1.e5.Characteristics of Patients with Vasospastic Angina in Korea: Data from a Large Cohort (VA-KOREA)
Sung Eun Kim, Sang-Ho Jo, Won-Woo Seo, Min-Ho Lee, Hyun-Jin Kim, Seong-Sik Cho, Kwan Yong Lee, Dong-Soo Kim, Tae-Hyun Yang, Sung-Ho Her, Seung Hwan Han, Byoung-Kwon Lee, Youngkeun Ahn, Seung-Woon Rha, Hyeon-Cheol Gwon, Dong-Ju Choi, Sang Hong Baek
Cardiovasc Prev Pharmacother. 2021;3(3):47-53. doi: 10.36011/cpp.2021.3.e8.
Reference
-
1. Ittaman SV, VanWormer JJ, Rezkalla SH. The role of aspirin in the prevention of cardiovascular disease. Clin Med Res. 2014; 12:147–54.
Article2. Raju NC, Eikelboom JW. The aspirin controversy in primary prevention. Curr Opin Cardiol. 2012; 27:499–507.
Article3. Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Kandala NB, Grove A, Gurung B, Morrow S, Clarke A. Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews. Health Technol Assess. 2013; 17:1–253.
Article4. Wolff T, Miller T, Ko S. Aspirin for the Primary Prevention of Cardiovascular Events: An Update of the Evidence for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality;2009.5. McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, Reid CM, Lockery JE, Kirpach B, Storey E, Shah RC, Williamson JD, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Orchard SG, Trevaks RE, Beilin LJ, Johnston CI, Ryan J, Radziszewska B, Jelinek M, Malik M, Eaton CB, Brauer D, Cloud G, Wood EM, Mahady SE, Satterfield S, Grimm R, Murray AM; ASPREE Investigator Group. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018; 379:1509–18.
Article6. Gaziano JM, Brotons C, Coppolecchia R, Cricelli C, Darius H, Gorelick PB, Howard G, Pearson TA, Rothwell PM, Ruilope LM, Tendera M, Tognoni G; ARRIVE Executive Committee. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet. 2018; 392:1036–46.
Article7. Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, Barton J, Murphy K, Aung T, Haynes R, Cox J, Murawska A, Young A, Lay M, Chen F, Sammons E, Waters E, Adler A, Bodansky J, Farmer A, McPherson R, Neil A, Simpson D, Peto R, Baigent C, Collins R, Parish S, Armitage J; ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018; 379:1529–39.8. Miwa K, Kambara H, Kawai C. Effect of aspirin in large doses on attacks of variant angina. Am Heart J. 1983; 105:351–5.
Article9. Clària J, Serhan CN. Aspirin triggers previously undescribed bioactive eicosanoids by human endothelial cell-leukocyte interactions. Proc Natl Acad Sci U S A. 1995; 92:9475–9.
Article10. Morris T, Stables M, Hobbs A, de Souza P, Colville-Nash P, Warner T, Newson J, Bellingan G, Gilroy DW. Effects of low-dose aspirin on acute inflammatory responses in humans. J Immunol. 2009; 183:2089–96.
Article11. Sueda S, Kohno H, Inoue K, Fukuda H, Suzuki J, Watanabe K, Ochi N, Kawada H, Uraoka T. Intracoronary administration of a thromboxane A2 synthase inhibitor relieves acetylcholine-induced coronary spasm. Circ J. 2002; 66:826–30.
Article12. Shin ES, Ann SH, Singh GB, Lim KH, Yoon HJ, Hur SH, Her AY, Koo BK, Akasaka T. OCT-defined morphological characteristics of coronary artery spasm sites in vasospastic angina. JACC Cardiovasc Imaging. 2015; 8:1059–67.13. Kim MC, Ahn Y, Park KH, Sim DS, Yoon NS, Yoon HJ, Kim KH, Hong YJ, Park HW, Kim JH, Jeong MH, Cho JG, Park JC, Kang JC. Clinical outcomes of low-dose aspirin administration in patients with variant angina pectoris. Int J Cardiol. 2013; 167:2333–4.
Article14. Lim AY, Park TK, Cho SW, Oh MS, Lee H, Seong CS, Gwag HB, Yang JH, Song YB, Hahn JY, Choi JH, Lee SH, Gwon HC, Ahn J, Carriere KC, Choi SH. Clinical implications of low-dose aspirin on vasospastic angina patients without significant coronary artery stenosis; a propensity score-matched analysis. Int J Cardiol. 2016; 221:161–6.
Article15. Park JY, Rha SW, Poddar KL, Ramasamy S, Chen KY, Li YJ, Choi BG, Ryu SK, Choi JW, Park SH, Park S, Elnagar A, Im SI, Kim SW, Na JO, Choi CU, Lim HE, Kim JW, Kim EJ, Han SW, Park CG, Seo HS, Oh DJ. Impact of low-dose aspirin on coronary artery spasm as assessed by intracoronary acetylcholine provocation test in Korean patients. J Cardiol. 2012; 60:187–91.
Article16. Shin DI, Baek SH, Her SH, Han SH, Ahn Y, Park KH, Kim DS, Yang TH, Choi DJ, Suh JW, Kwon HM, Lee BK, Gwon HC, Rha SW, Jo SH. The 24-month prognosis of patients with positive or intermediate results in the intracoronary ergonovine provocation test. JACC Cardiovasc Interv. 2015; 8:914–23.
Article17. Sueda S, Kohno H, Ochi T, Uraoka T. Overview of the acetylcholine spasm provocation test. Clin Cardiol. 2015; 38:430–8.
Article18. Galvão Braga C, Ramos V, Vieira C, Martins J, Ribeiro S, Gaspar A, Salgado A, Azevedo P, Alvares Pereira M, Magalhães S, Correia A. New-onset atrial fibrillation during acute coronary syndromes: predictors and prognosis. Rev Port Cardiol. 2014; 33:281–7.
Article19. Gum PA, Thamilarasan M, Watanabe J, Blackstone EH, Lauer MS. Aspirin use and all-cause mortality among patients being evaluated for known or suspected coronary artery disease: a propensity analysis. JAMA. 2001; 286:1187–94.
Article20. Takagi Y, Takahashi J, Yasuda S, Miyata S, Tsunoda R, Ogata Y, Seki A, Sumiyoshi T, Matsui M, Goto T, Tanabe Y, Sueda S, Sato T, Ogawa S, Kubo N, Momomura S, Ogawa H, Shimokawa H; Japanese Coronary Spasm Association. Prognostic stratification of patients with vasospastic angina: a comprehensive clinical risk score developed by the Japanese Coronary Spasm Association. J Am Coll Cardiol. 2013; 62:1144–53.21. Ishii M, Kaikita K, Sato K, Yamanaga K, Miyazaki T, Akasaka T, Tabata N, Arima Y, Sueta D, Sakamoto K, Yamamoto E, Tsujita K, Yamamuro M, Kojima S, Soejima H, Hokimoto S, Matsui K, Ogawa H. Impact of aspirin on the prognosis in patients with coronary spasm without significant atherosclerotic stenosis. Int J Cardiol. 2016; 220:328–32.
Article22. Dauerman HL. Reconsidering the necessity of aspirin in stable coronary artery disease. J Am Coll Cardiol. 2014; 64:1437–40.
Article23. Cuzick J, Thorat MA, Bosetti C, Brown PH, Burn J, Cook NR, Ford LG, Jacobs EJ, Jankowski JA, La Vecchia C, Law M, Meyskens F, Rothwell PM, Senn HJ, Umar A. Estimates of benefits and harms of prophylactic use of aspirin in the general population. Ann Oncol. 2015; 26:47–57.
Article24. Halvorsen S, Andreotti F, ten Berg JM, Cattaneo M, Coccheri S, Marchioli R, Morais J, Verheugt FW, De Caterina R. Aspirin therapy in primary cardiovascular disease prevention: a position paper of the European Society of Cardiology working group on thrombosis. J Am Coll Cardiol. 2014; 64:319–27.25. Vandvik PO, Lincoff AM, Gore JM, Gutterman DD, Sonnenberg FA, Alonso-Coello P, Akl EA, Lansberg MG, Guyatt GH, Spencer FA. Primary and secondary prevention of cardiovascular disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141:e637S–e668S.26. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB Sr, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC Jr, Sorlie P, Stone NJ, Wilson PW. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/ American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014; 63:2935–59.27. Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer. Summaries for patients. Screening for suicide risk in adolescents, adults, and older adults in primary care: recommendations from the U.S. Preventive Services Task Force. Ann Intern Med. 2014; 160:I–22.28. Suzuki H, Kawai S, Aizawa T, Kato K, Sunayama S, Okada R, Yamaguchi H. Histological evaluation of coronary plaque in patients with variant angina: relationship between vasospasm and neointimal hyperplasia in primary coronary lesions. J Am Coll Cardiol. 1999; 33:198–205.
Article29. Ishii M, Kaikita K, Sato K, Tanaka T, Sugamura K, Sakamoto K, Izumiya Y, Yamamoto E, Tsujita K, Yamamuro M, Kojima S, Soejima H, Hokimoto S, Matsui K, Ogawa H. Acetylcholine-provoked coronary spasm at site of significant organic stenosis predicts poor prognosis in patients with coronary vasospastic angina. J Am Coll Cardiol. 2015; 66:1105–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Aspirin Has a Neutral Effect in Preventing Future Cardiovascular Events in Vasospastic Angina
- Exercise-Induced Vasospastic Angina With Prominent Regional Wall Motion Abnormality
- The Vasomotor Tone In Vasospastic Angina
- Diagnostic Significance of ECG Ergonovine Provocation Test in Patients with Vasospastic Angina
- The Association Between Asymmetric Dimethylarginine (ADMA) and Vasospastic Angina, Hypertension, and Cardiovascular Risk Factors