Cardiovasc Prev Pharmacother.
2022 Jan;4(1):18-25. 10.36011/cpp.2022.4.e1.
Indirect comparison of nonvitamin K oral anticoagulants and left atrial appendage occlusion
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Public Health Science, Graduate School of Public Health, Seoul National University, Seoul, Korea
- KMID: 2536929
- DOI: http://doi.org/10.36011/cpp.2022.4.e1
Abstract
- Background
Anticoagulation is important in atrial fibrillation (AF) patients to reduce the occurrence of thrombotic events. We evaluated the efficacy and safety of percutaneous left atrial appendage occlusion (LAAO) as an alternative to systemic anticoagulation through an indirect comparative analysis.
Methods
An indirect comparative analysis of nonvitamin K oral anticoagulants (NOACs) and LAAO was conducted. Comparisons were made using data from four landmark randomized clinical trials (RE-LY, ROCKET-AF, ARISTOTLE, and PROTECT AF). Using warfarin as the common comparator, an indirect comparison was performed using data from each trial, and the relative risk was calculated between NOACs and LAAO.
Results
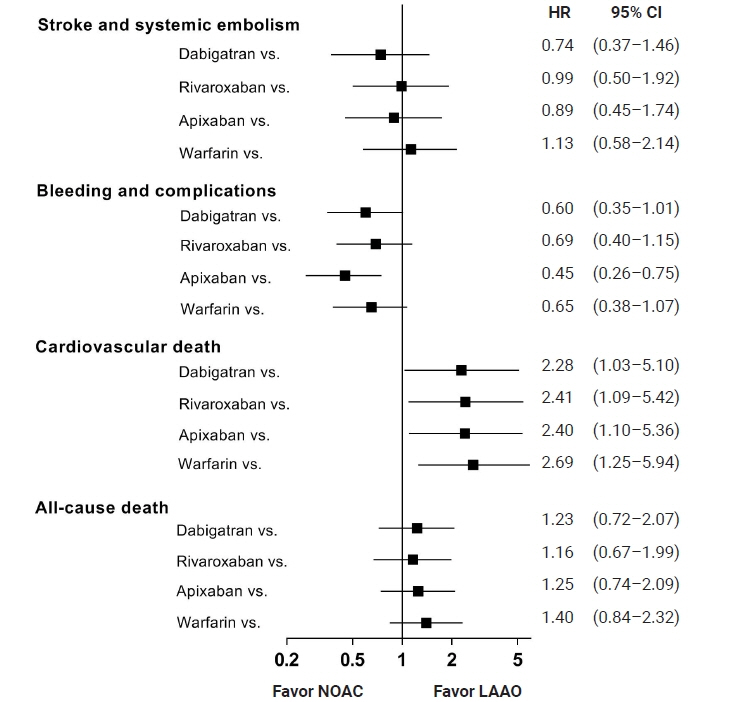
NOACs and LAAO showed similar results for the reduction of stroke and systemic embolism, with a non-statistically significant trend favoring NOACs (hazard ratio [HR], 0.74; 95% confidence interval [CI], 0.37–1.46 for dabigatran; HR, 0.99; 95% CI, 0.50–1.92 for rivaroxaban; HR, 0.89; 95% CI, 0.45–1.74 for apixaban). Significantly fewer major bleeding and procedure-related complications were found in patients treated with apixaban compared with LAAO (HR, 0.45; 95% CI, 0.26–0.75). Cardiovascular death occurred more frequently in patients administered NOACs than in patients with LAAO (HR, 2.28; 95% CI, 1.03–5.10 for dabigatran; HR, 2.41; 95% CI, 1.09–5.42 for rivaroxaban; HR, 2.40; 95% CI, 1.10–5.36 for apixaban).
Conclusions
The rate of all-cause death was similar between NOACs and LAAO. Compared with LAAO, NOACs led to a nonsignificant numerical decrease in stroke and embolism in AF patients. Significantly fewer safety events occurred in patients treated with apixaban. LAAO significantly reduced cardiovascular death.
Keyword
Figure
Reference
-
1. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991; 22:983–8.
Article2. Kimura K, Minematsu K, Yamaguchi T; Japan Multicenter Stroke Investigators’ Collaboration (J-MUSIC). Atrial fibrillation as a predictive factor for severe stroke and early death in 15,831 patients with acute ischaemic stroke. J Neurol Neurosurg Psychiatry. 2005; 76:679–83.3. Friberg L, Rosenqvist M, Lip GY. Net clinical benefit of warfarin in patients with atrial fibrillation: a report from the Swedish atrial fibrillation cohort study. Circulation. 2012; 125:2298–307.
Article4. Ogilvie IM, Newton N, Welner SA, Cowell W, Lip GY. Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med. 2010; 123:638–45.
Article5. Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–51.
Article6. Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–91.
Article7. Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–92.8. Holmes DR, Reddy VY, Turi ZG, Doshi SK, Sievert H, Buchbinder M, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet. 2009; 374:534–42.
Article9. Rodes-Cabau J, Champagne J, Bernier M. Transcatheter closure of the left atrial appendage: initial experience with the Amplatzer cardiac plug device. Catheter Cardiovasc Interv. 2010; 76:186–92.
Article10. Stoddard MF, Dawkins PR, Prince CR, Ammash NM. Left atrial appendage thrombus is not uncommon in patients with acute atrial fibrillation and a recent embolic event: a transesophageal echocardiographic study. J Am Coll Cardiol. 1995; 25:452–9.11. Reddy VY, Doshi SK, Sievert H, Buchbinder M, Neuzil P, Huber K, et al. Percutaneous left atrial appendage closure for stroke prophylaxis in patients with atrial fibrillation: 2.3-Year Follow-up of the PROTECT AF (Watchman Left Atrial Appendage System for Embolic Protection in Patients with Atrial Fibrillation) Trial. Circulation. 2013; 127:720–9.
Article12. Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 Focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation: developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33:2719–47.13. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1–76.14. Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al. Indirect comparisons of competing interventions. Health Technol Assess. 2005; 9:1–134.
Article15. Miladinovic B, Chaimani A, Hozo I, Djulbegovic B. Indirect treatment comparison. Stata J. 2014; 14:76–86.
Article16. Rasmussen LH, Larsen TB, Graungaard T, Skjoth F, Lip GY. Primary and secondary prevention with new oral anticoagulant drugs for stroke prevention in atrial fibrillation: indirect comparison analysis. BMJ. 2012; 345:e7097.
Article17. Holmes DR Jr, Kar S, Price MJ, Whisenant B, Sievert H, Doshi SK, et al. Prospective randomized evaluation of the Watchman Left Atrial Appendage Closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol. 2014; 64:1–12.
Article18. Biondi-Zoccai G, Lotrionte M, Agostoni P, Abbate A, Romagnoli E, Sangiorgi G, et al. Adjusted indirect comparison meta-analysis of prasugrel versus ticagrelor for patients with acute coronary syndromes. Int J Cardiol. 2011; 150:325–31.
Article19. Cassese S, Ndrepepa G, King LA, Tada T, Fusaro M, Kastrati A. Two zotarolimus-eluting stent generations: a meta-analysis of 12 randomised trials versus other limus-eluting stents and an adjusted indirect comparison. Heart. 2012; 98:1632–40.
Article20. Kwok CS, Pradhan S, Yeong JK, Loke YK. Relative effects of two different enoxaparin regimens as comparators against newer oral anticoagulants: meta-analysis and adjusted indirect comparison. Chest. 2013; 144:593–600.
Article21. Colmenarez H, Fernandez C, Escaned J. Impact of technological developments in drug-eluting stents on patient-focused outcomes: a pooled direct and indirect comparison of randomised trials comparing first- and second-generation drug-eluting stents. EuroIntervention. 2014; 10:942–52.
Article22. Mantha S, Ansell J. Indirect comparison of dabigatran, rivaroxaban, apixaban and edoxaban for the treatment of acute venous thromboembolism. J Thromb Thrombolysis. 2015; 39:155–65.
Article23. Briceno DF, Villablanca P, Cyrille N, Massera D, Bader E, Manheimer E, et al. Left atrial appendage occlusion device and novel oral anticoagulants versus warfarin for stroke prevention in nonvalvular atrial fibrillation: systematic review and meta-analysis of randomized controlled trials. Circ Arrhythm Electrophysiol. 2015; 8:1057–64.24. Ziegler PD, Glotzer TV, Daoud EG, Wyse DG, Singer DE, Ezekowitz MD, et al. Incidence of newly detected atrial arrhythmias via implantable devices in patients with a history of thromboembolic events. Stroke. 2010; 41:256–60.
Article25. Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, et al. Stroke severity in atrial fibrillation: the Framingham Study. Stroke. 1996; 27:1760–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Sealing of WATCHMAN Device Shunt
- Current methods of left atrial appendage closure: the non‑pharmacological approach for stroke prevention in atrial fibrillation patients
- Simultaneous Closure of a Left Atrial Appendage through an Atrial Septal Defect and the Atrial Septal Defect
- Is Left Atrial Appendage Occlusion Always Better than Direct Oral Anticoagulants?
- Interventional Treatment for Stroke Prevention