Korean J Sports Med.
2022 Dec;40(4):263-269. 10.5763/kjsm.2022.40.4.263.
Open Reduction and Primary Ligament Suture for Irreducible Knee Dislocation: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Daejeon Sun Hospital, Daejeon, Korea
- KMID: 2536678
- DOI: http://doi.org/10.5763/kjsm.2022.40.4.263
Abstract
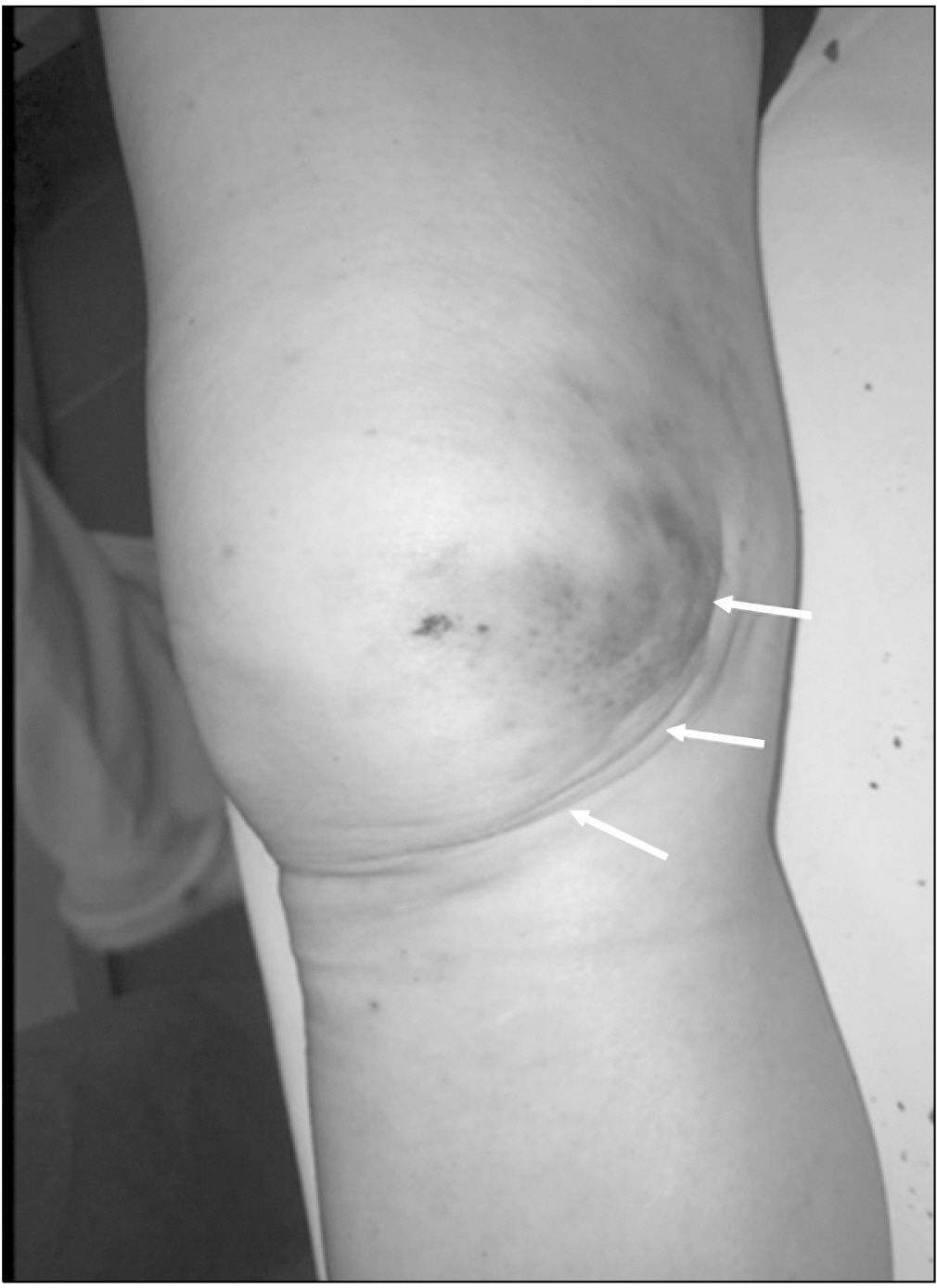
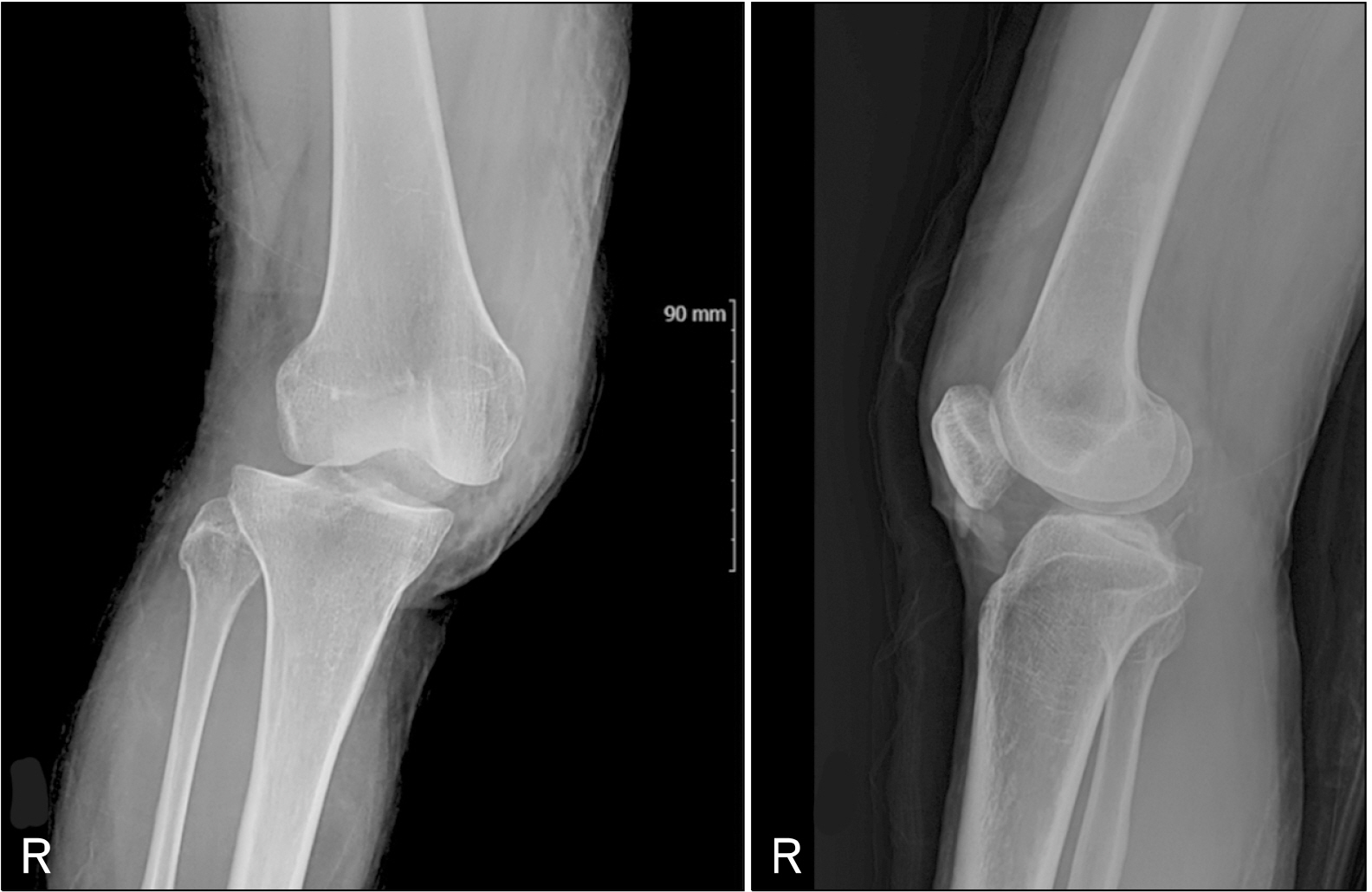
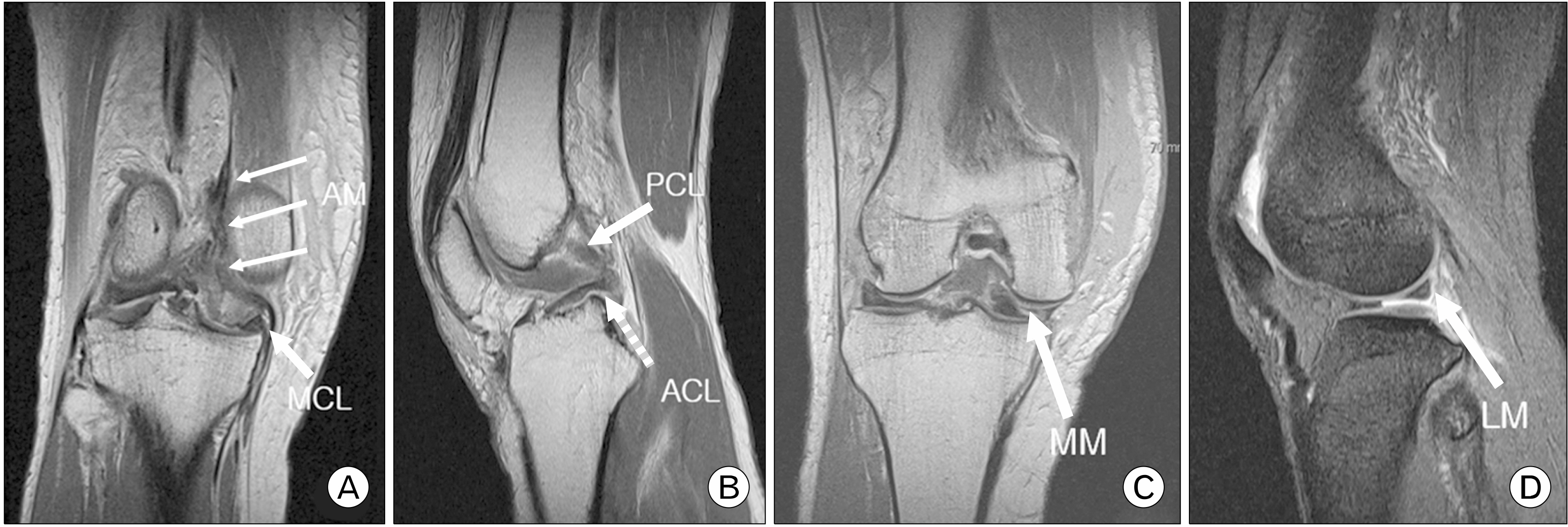
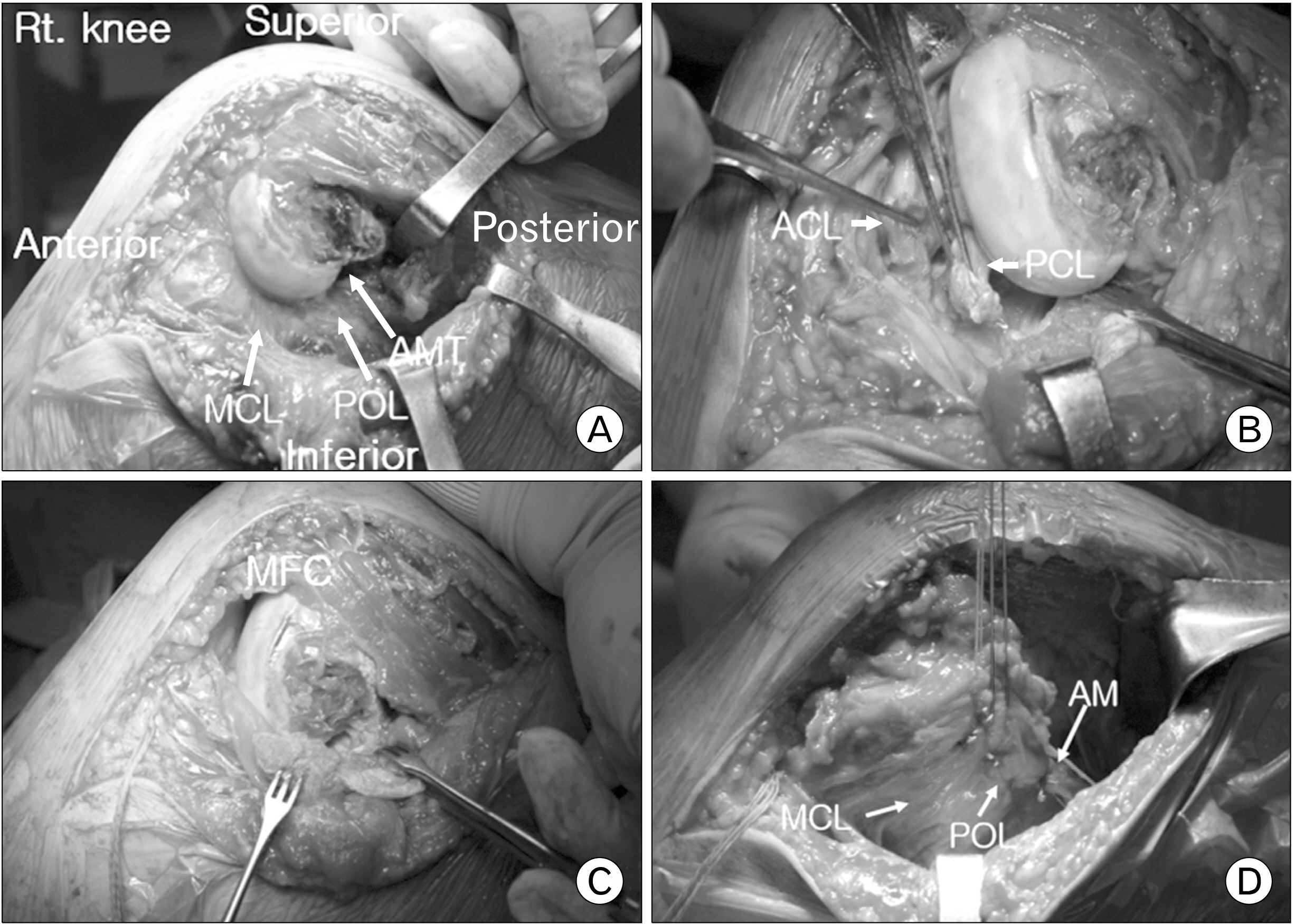
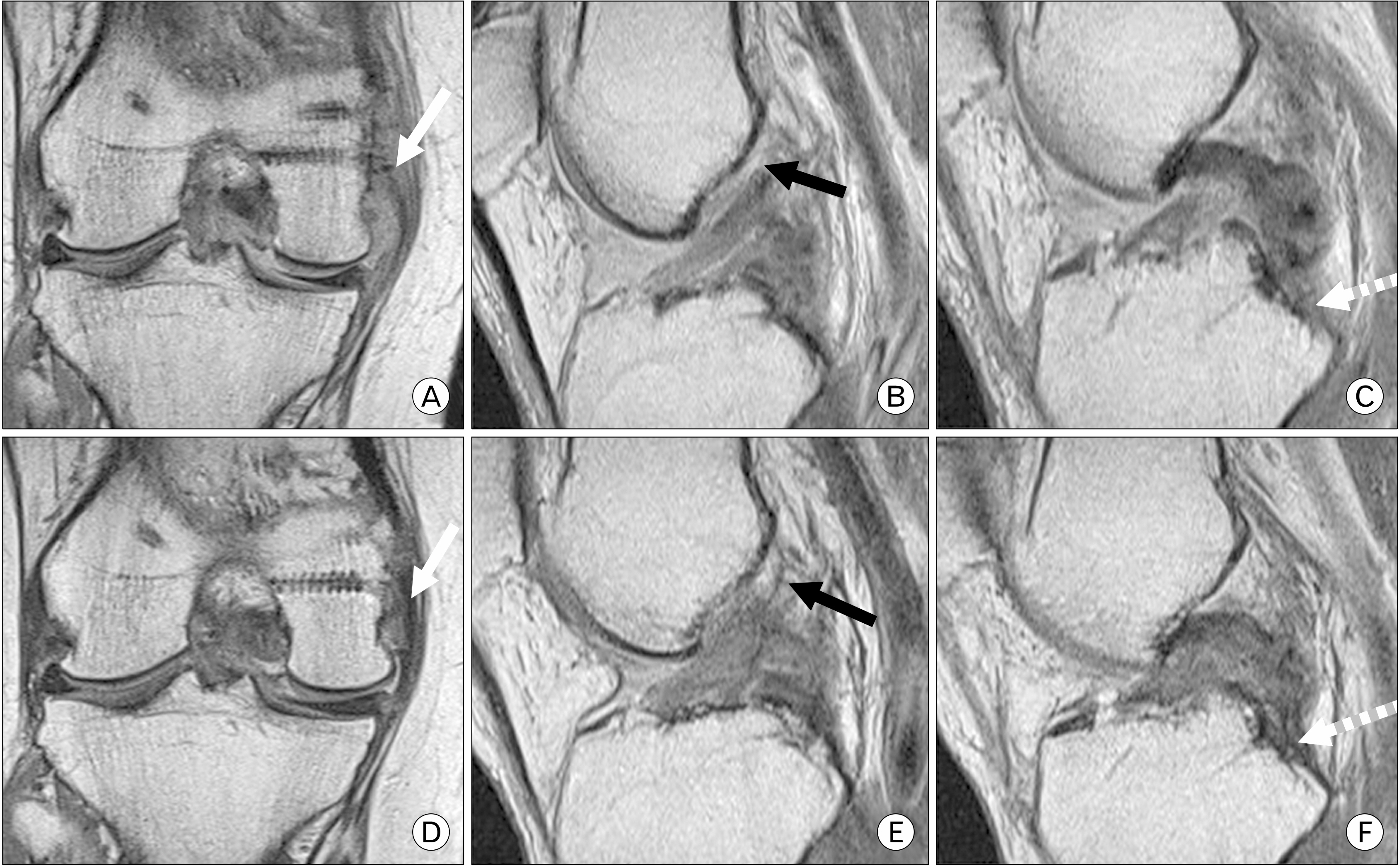
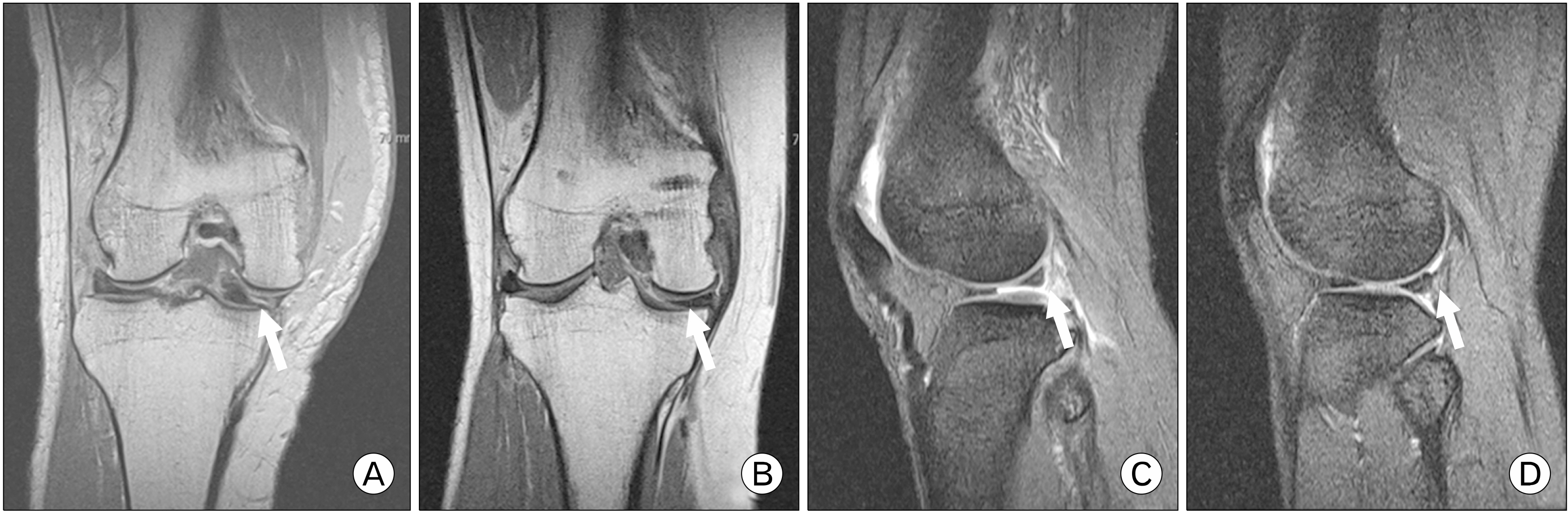
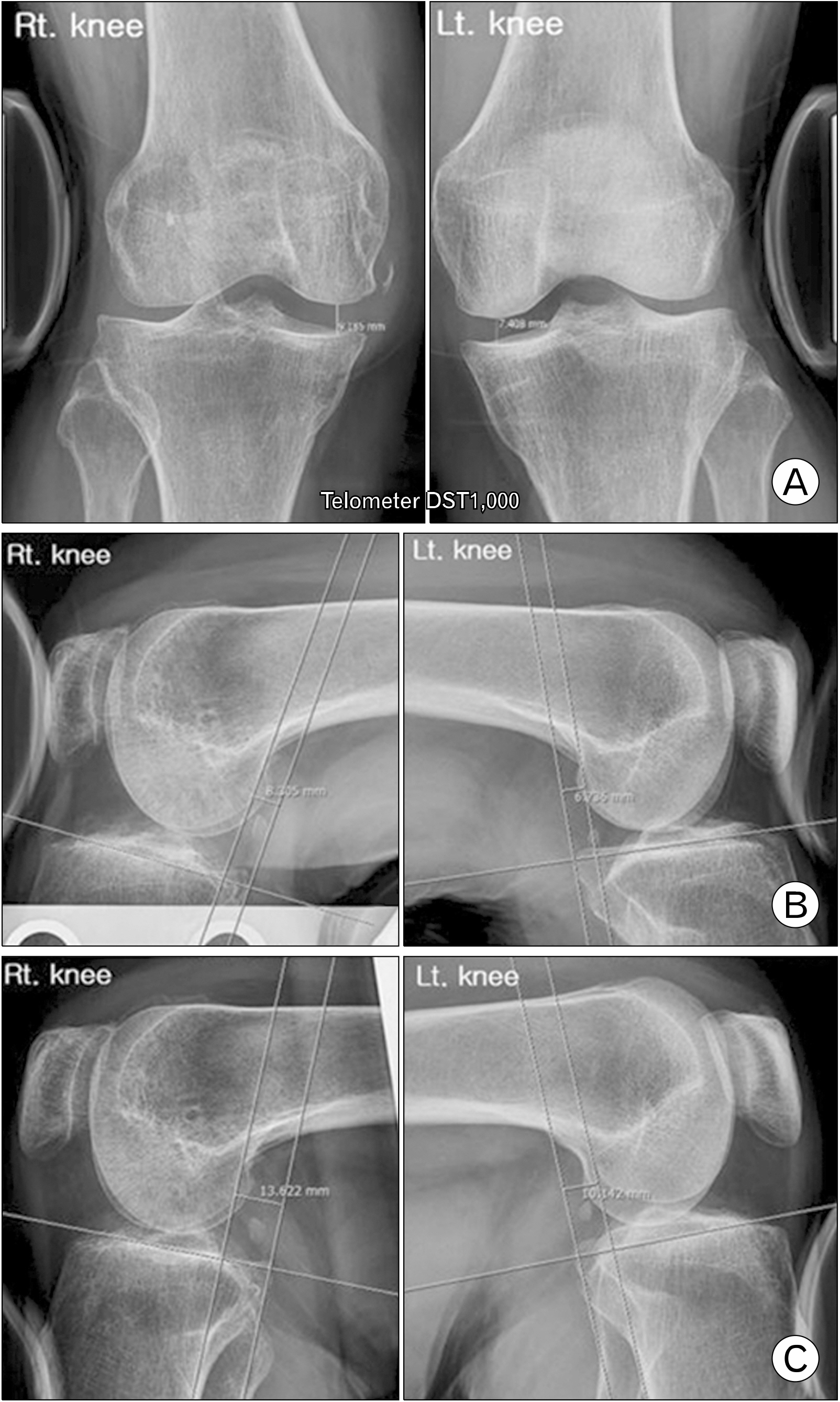
- Irreducible knee dislocation among acute knee dislocations is very rare. If reduction and treatment are not performed early, serious complications such as skin necrosis, vascular and nerve injury, compartment syndrome, and instability can occur. So far, treatment options, such as two-staged operation with early open reduction and delayed ligaments reconstruction or repair, one-staged arthroscopic reduction without ligaments reconstruction or repair, one-staged operation with open reduction and ligaments reconstruction have been reported for the irreducible knee dislocation. In this case, the authors have found satisfactory results following one-staged operation with open reduction and primary ligament suture after diagnosing the exact injury site using magnetic resonance imaging preoperatively.
Keyword
Figure
Reference
-
1. Capito N, Gregory MH, Volgas D, Sherman SL. 2013; Evaluation and management of an irreducible posterolateral knee dislocation. J Knee Surg. 26 Suppl 1:S136–41. DOI: 10.1055/s-0033-1341577. PMID: 23512541.
Article2. Lee HS, Lee SH, Lee SW. 2020; Closed reduction of irreducible posterolateral rotatory knee dislocation. J Korean Orthop Assoc. 55:95–100. DOI: 10.4055/jkoa.2020.55.1.95.
Article3. Koh HS, Kim HS, Lee HS. 2009; Irreducible Posterolateral Dislocation of the Knee Joint with Lateral Dislocation of the Patella: a report of two cases. Knee Surg Relat Res. 21:51–6.4. Kim HS, Park SR, Kang JS, Lee WH, Kim KW. 2001; A rare case of irreducible knee dislocation: vastus medialis obliqus-buttonholing of medial femoral condyle: a case report. J Korean Arthrosc Soc. 5:41–4.5. Malik SS, MacDonald PB. 2020; The irreducible knee dislocation. J Knee Surg. 33:328–34. DOI: 10.1055/s-0039-1698749. PMID: 31756734.
Article6. Jeong JY. 2009; Arthroscopic reduction of irreducible knee dislocation: a case report. J Korean Arthrosc Soc. 13:161–4.7. Lim JC, Kim SH, Seo SH, Kim YM. 2019; A Study of applied pressure according to knee variable during Lachman test for anterior cruciate ligament using Telos device. J Korean Radiology Soc. 13:391–8.8. Huang FS, Simonian PT, Chansky HA. 2000; Irreducible posterolateral dislocation of the knee. Arthroscopy. 16:323–7. DOI: 10.1016/S0749-8063(00)90057-4. PMID: 10750013.
Article9. Solarino G, Notarnicola A, Maccagnano G, Piazzolla A, Moretti B. 2015; Irreducible posterolateral dislocation of the knee: a case report. Joints. 3:91–6. DOI: 10.11138/jts/2015.3.2.091. PMID: 26605258. PMCID: PMC4634811.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthroscopic Reduction of Irreducible Posterolateral Knee Dislocation with Interposition of the Vastus Medialis: A Case Report
- Closed Reduction of Irreducible Posterolateral Rotatory Knee Dislocation
- Irreducible Posterolateral Dislocation of the Knee Joint with Lateral Dislocation of the Patella: A Report of Two Cases
- Irreducible Dislocation of the Interphalangeal Joint of the Thumb: A Case Report
- Irreducible Knee Dislocation with Vastus Medialis Muscle Interposition