Diabetes Metab J.
2022 Nov;46(6):912-922. 10.4093/dmj.2021.0340.
Influence of Maternal Diabetes on the Risk of Neurodevelopmental Disorders in Offspring in the Prenatal and Postnatal Periods
- Affiliations
-
- 1Endocrinology and Nutrition Department, University Hospital Mutua de Terrassa, Terrassa, Spain
- 2Obstetrics and Gynecology Department, University Hospital Mutua de Terrassa, Terrassa, Spain
- 3Endocrinology and Nutrition Department, Hospital Clinic de Barcelona, Barcelona, Spain
- KMID: 2536149
- DOI: http://doi.org/10.4093/dmj.2021.0340
Abstract
- Background
This study aimed to evaluate the influence of maternal diabetes in the risk of neurodevelopmental disorders in offspring in the prenatal and postnatal periods.
Methods
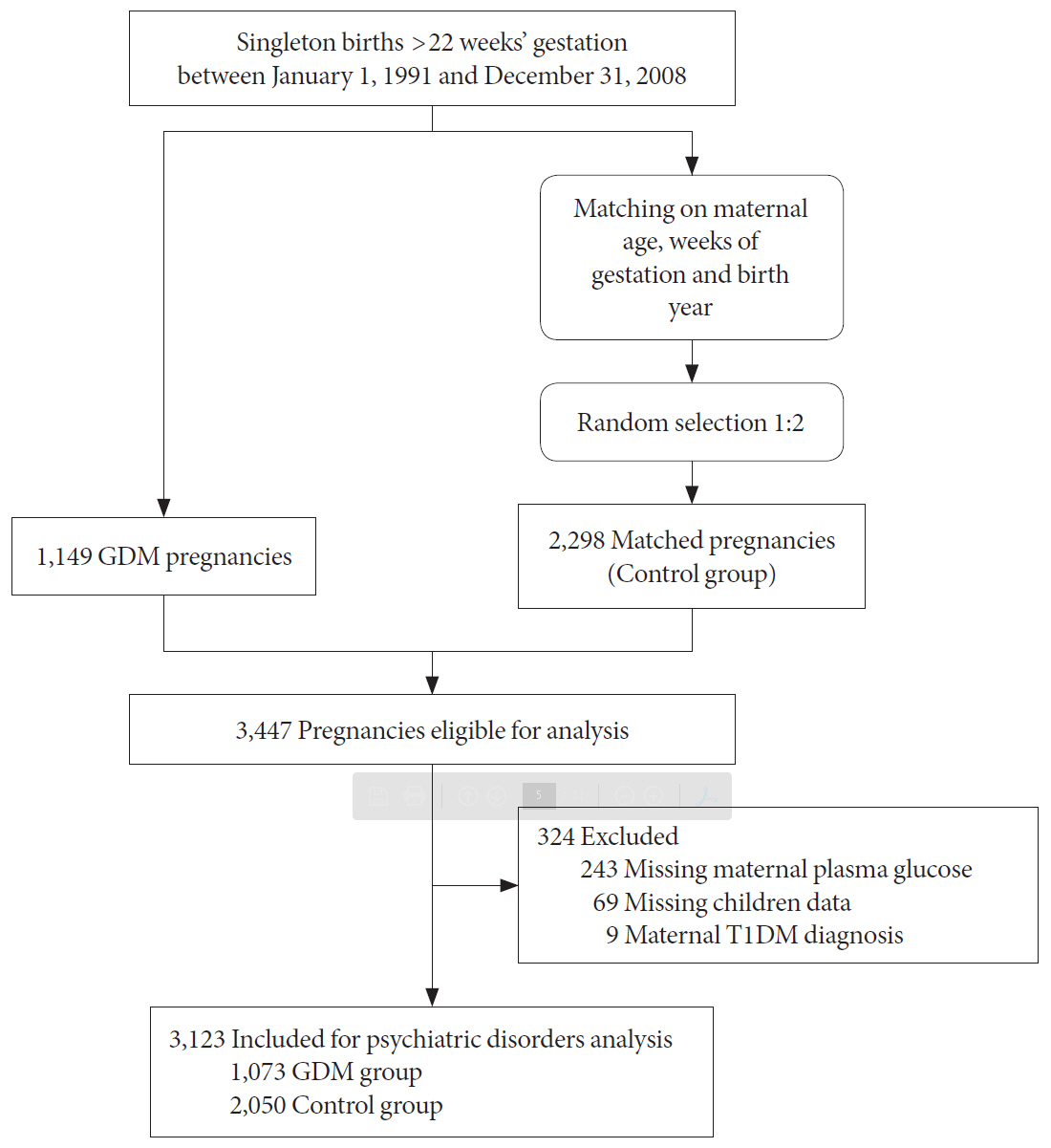
This cohort study included singleton gestational diabetes mellitus (GDM) pregnancies >22 weeks’ gestation with live newborns between 1991 and 2008. The control group was randomly selected and matched (1:2) for maternal age, weeks of gestation and birth year. Cox regression models estimated the effect of GDM on the risk of attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), and maternal type 2 diabetes mellitus (T2DM). Moreover, interaction between maternal T2DM and GDM-ADHD relationship was evaluated.
Results
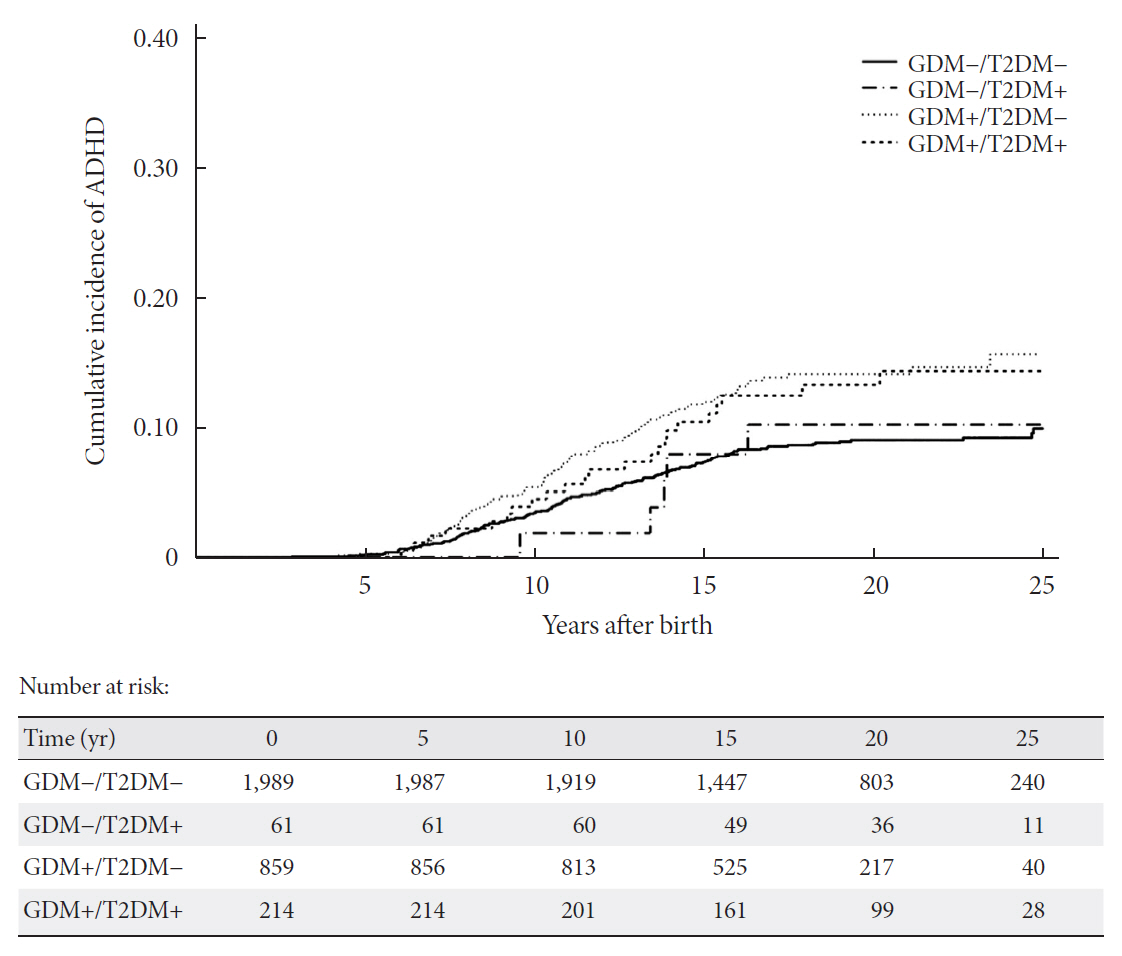
Children (n=3,123) were included (1,073 GDM; 2,050 control group). The median follow-up was 18.2 years (interquartile range, 14.2 to 22.3) (n=323 with ADHD, n=36 with ASD, and n=275 from women who developed T2DM). GDM exposure was associated with ADHD (hazard ratio [HR]crude, 1.67; 95% confidence interval [CI], 1.33 to 2.07) (HRadjusted, 1.64; 95% CI, 1.31 to 2.05). This association remained significant regardless of the treatment (diet or insulin) and diagnosis after 26 weeks of gestation. Children of mothers who developed T2DM presented higher rates of ADHD (14.2 vs. 10%, P=0.029). However, no interaction was found when T2DM was included in the GDM and ADHD models (P>0.05). GDM was not associated with an increased risk of ASD (HRadjusted, 1.46; 95% CI, 0.74 to 2.84).
Conclusion
Prenatal exposure to GDM increases the risk of ADHD in offspring, regardless of GDM treatment complexity. However, postnatal exposure to maternal T2DM was not related to the development of ADHD.
Figure
Reference
-
1. Ricart W, Lopez J, Mozas J, Pericot A, Sancho MA, Gonzalez N, et al. Potential impact of American Diabetes Association (2000) criteria for diagnosis of gestational diabetes mellitus in Spain. Diabetologia. 2005; 48:1135–41.
Article2. Buckley BS, Harreiter J, Damm P, Corcoy R, Chico A, Simmons D, et al. Gestational diabetes mellitus in Europe: prevalence, current screening practice and barriers to screening: a review. Diabet Med. 2012; 29:844–54.
Article3. HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008; 358:1991–2002.
Article4. Yamamoto JM, Benham JL, Dewey D, Sanchez JJ, Murphy HR, Feig DS, et al. Neurocognitive and behavioural outcomes in offspring exposed to maternal pre-existing diabetes: a systematic review and meta-analysis. Diabetologia. 2019; 62:1561–74.
Article5. Xiang AH, Wang X, Martinez MP, Walthall JC, Curry ES, Page K, et al. Association of maternal diabetes with autism in offspring. JAMA. 2015; 313:1425–34.
Article6. Xiang AH, Wang X, Martinez MP, Getahun D, Page KA, Buchanan TA, et al. Maternal gestational diabetes mellitus, type 1 diabetes, and type 2 diabetes during pregnancy and risk of ADHD in offspring. Diabetes Care. 2018; 41:2502–8.
Article7. Guo D, Ju R, Zhou Q, Mao J, Tao H, Jing H, et al. Association of maternal diabetes with attention deficit/hyperactivity disorder (ADHD) in offspring: a meta-analysis and review. Diabetes Res Clin Pract. 2020; 165:108269.
Article8. Kong L, Norstedt G, Schalling M, Gissler M, Lavebratt C. The risk of offspring psychiatric disorders in the setting of maternal obesity and diabetes. Pediatrics. 2018; 142:e20180776.
Article9. Getahun D, Rhoads GG, Demissie K, Lu SE, Quinn VP, Fassett MJ, et al. In utero exposure to ischemic-hypoxic conditions and attention-deficit/hyperactivity disorder. Pediatrics. 2013; 131:e53–61.
Article10. Biri A, Onan A, Devrim E, Babacan F, Kavutcu M, Durak I. Oxidant status in maternal and cord plasma and placental tissue in gestational diabetes. Placenta. 2006; 27:327–32.
Article11. McCann D, Barrett A, Cooper A, Crumpler D, Dalen L, Grimshaw K, et al. Food additives and hyperactive behaviour in 3-year-old and 8/9-year-old children in the community: a randomised, double-blinded, placebo-controlled trial. Lancet. 2007; 370:1560–7.
Article12. Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and metaanalysis. BMJ. 2020; 369:m1361.
Article13. Salas-Salvado J, Bullo M, Babio N, Martinez-Gonzalez MA, Ibarrola-Jurado N, Basora J, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care. 2011; 34:14–9.14. Metzger BE. Summary and recommendations of the Third International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes. 1991; 40 Suppl 2:197–201.
Article15. Acosta D, Balsells M, Ballesteros M, Bandres MO, Bartha JL, Bellart J, et al. Care of pregnancies complicated by diabetes. Clinical practice guidelines: 2014 update. Av Diabetol. 2015; 31:45–59.16. Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Diabetologia. 2016; 59:1403–11.
Article17. Albareda M, Caballero A, Badell G, Piquer S, Ortiz A, de Leiva A, et al. Diabetes and abnormal glucose tolerance in women with previous gestational diabetes. Diabetes Care. 2003; 26:1199–205.
Article18. Knorr S, Clausen TD, Vlachova Z, Bytoft B, Damm P, BeckNielsen H, et al. Academic achievement in primary school in offspring born to mothers with type 1 diabetes (the EPICOM Study): a register-based prospective cohort study. Diabetes Care. 2015; 38:1238–44.
Article19. Xiang AH, Wang X, Martinez MP, Page K, Buchanan TA, Feldman RK. Maternal type 1 diabetes and risk of autism in offspring. JAMA. 2018; 320:89–91.
Article20. Nielsen TC, Nassar N, Shand AW, Jones H, Guastella AJ, Dale RC, et al. Association of maternal autoimmune disease with attention-deficit/hyperactivity disorder in children. JAMA Pediatr. 2021; 175:e205487.
Article21. Chen S, Zhao S, Dalman C, Karlsson H, Gardner R. Association of maternal diabetes with neurodevelopmental disorders: autism spectrum disorders, attention-deficit/hyperactivity disorder and intellectual disability. Int J Epidemiol. 2021; 50:459–74.
Article22. Menon RK, Cohen RM, Sperling MA, Cutfield WS, Mimouni F, Khoury JC. Transplacental passage of insulin in pregnant women with insulin-dependent diabetes mellitus: its role in fetal macrosomia. N Engl J Med. 1990; 323:309–15.
Article23. Rowan JA, Hague WM, Gao W, Battin MR, Moore MP; MiG Trial Investigators. Metformin versus insulin for the treatment of gestational diabetes. N Engl J Med. 2008; 358:2003–15.
Article24. Picon-Cesar MJ, Molina-Vega M, Suarez-Arana M, GonzalezMesa E, Sola-Moyano AP, Roldan-Lopez R, et al. Metformin for gestational diabetes study: metformin vs insulin in gestational diabetes: glycemic control and obstetrical and perinatal outcomes: randomized prospective trial. Am J Obstet Gynecol. 2021; 225:517.25. Wang X, Liu W, Chen H, Chen Q. Comparison of insulin, metformin, and glyburide on perinatal complications of gestational diabetes mellitus: a systematic review and meta-analysis. Gynecol Obstet Invest. 2021; 86:218–30.
Article26. Miller JA, Ding SL, Sunkin SM, Smith KA, Ng L, Szafer A, et al. Transcriptional landscape of the prenatal human brain. Nature. 2014; 508:199–206.
Article27. Tsakiridis I, Giouleka S, Mamopoulos A, Kourtis A, Athanasiadis A, Filopoulou D, et al. Diagnosis and management of gestational diabetes mellitus: an overview of national and international guidelines. Obstet Gynecol Surv. 2021; 76:367–81.
Article28. Hyman SL, Levy SE, Myers SM; Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. 2020; 145:e20193447.
Article29. Mahmood L, Flores-Barrantes P, Moreno LA, Manios Y, Gonzalez-Gil EM. The influence of parental dietary behaviors and practices on children’s eating habits. Nutrients. 2021; 13:1138.
Article30. Kase BE, Rommelse N, Chen Q, Li L, Andersson A, Du Rietz E, et al. Longitudinal associations between symptoms of ADHD and BMI from late childhood to early adulthood. Pediatrics. 2021; 147:e2020036657.
Article31. Lindekilde N, Rutters F, Erik Henriksen J, Lasgaard M, Schram MT, Rubin KH, et al. Psychiatric disorders as risk factors for type 2 diabetes: an umbrella review of systematic reviews with and without meta-analyses. Diabetes Res Clin Pract. 2021; 176:108855.
Article32. Liu S, Kuja-Halkola R, Larsson H, Lichtenstein P, Ludvigsson JF, Svensson AM, et al. Poor glycaemic control is associated with increased risk of neurodevelopmental disorders in childhood-onset type 1 diabetes: a population-based cohort study. Diabetologia. 2021; 64:767–77.
Article33. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346:393–403.
Article34. Barnard-Kelly KD, Chernavvsky D. Social inequality and diabetes: a commentary. Diabetes Ther. 2020; 11:803–11.35. Posner J, Polanczyk GV, Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet. 2020; 395:450–62.
Article36. Bosch R, Pagerols M, Rivas C, Sixto L, Bricolle L, EspanolMartin G, et al. Neurodevelopmental disorders among Spanish school-age children: prevalence and sociodemographic correlates. Psychol Med. 2021; Jan. 13. [Epub]. https://doi.org/10.1017/S0033291720005115.
Article37. Dani C, Corsini I. Guidelines for management of neonatal hypoglycemia: are they actually applicable? JAMA Pediatr. 2020; 174:638–9.38. Jobe AH, Goldenberg RL. Antenatal corticosteroids: an assessment of anticipated benefits and potential risks. Am J Obstet Gynecol. 2018; 219:62–74.
Article39. de Lusignan S, Sadek N, Mulnier H, Tahir A, Russell-Jones D, Khunti K. Miscoding, misclassification and misdiagnosis of diabetes in primary care. Diabet Med. 2012; 29:181–9.
Article40. Kong L, Nilsson IA, Brismar K, Gissler M, Lavebratt C. Associations of different types of maternal diabetes and body mass index with offspring psychiatric disorders. JAMA Netw Open. 2020; 3:e1920787.
Article41. Benhalima K, Mathieu C, Van Assche A, Damm P, Devlieger R, Mahmood T, et al. Survey by the European Board and College of Obstetrics and Gynaecology on screening for gestational diabetes in Europe. Eur J Obstet Gynecol Reprod Biol. 2016; 201:197–202.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prenatal Factors Influencing Long-Term Neurodevelopmental Outcomes
- Prenatal Topiramate Exposure and Risk of Neurodevelopmental Disorders: A Systematic Review
- Postnatal Treadmill Exercise Alleviates Prenatal Stress-Induced Anxiety in Offspring Rats by Enhancing Cell Proliferation Through 5-Hydroxytryptamine 1A Receptor Activation
- Association between Maternal Adverse Childhood Experiences and Risk of Post-traumatic Stress Disorder in the Offspring
- Influence of clozapine on neurodevelopmental protein expression and behavioral patterns in animal model of psychiatric disorder induced by low-level of lead