Korean J Women Health Nurs.
2022 Jun;28(2):87-99. 10.4069/kjwhn.2022.05.15.
Fatigue relief by aromatherapy use in prenatal and postnatal women: a systematic review and meta-analysis
- Affiliations
-
- 1College of Nursing, Konyang University, Daejeon, Korea
- KMID: 2535426
- DOI: http://doi.org/10.4069/kjwhn.2022.05.15
Abstract
- Purpose
The purpose of this systematic review was to examine aromatherapy interventions for prenatal and postnatal women, and to determine the effectiveness of these interventions on fatigue.
Methods
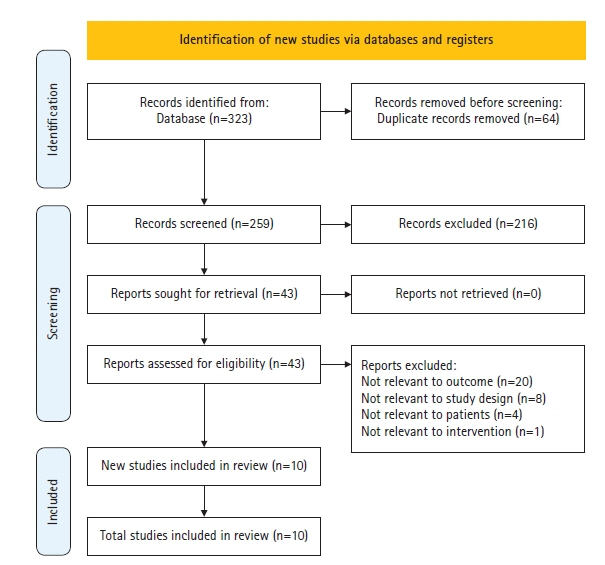
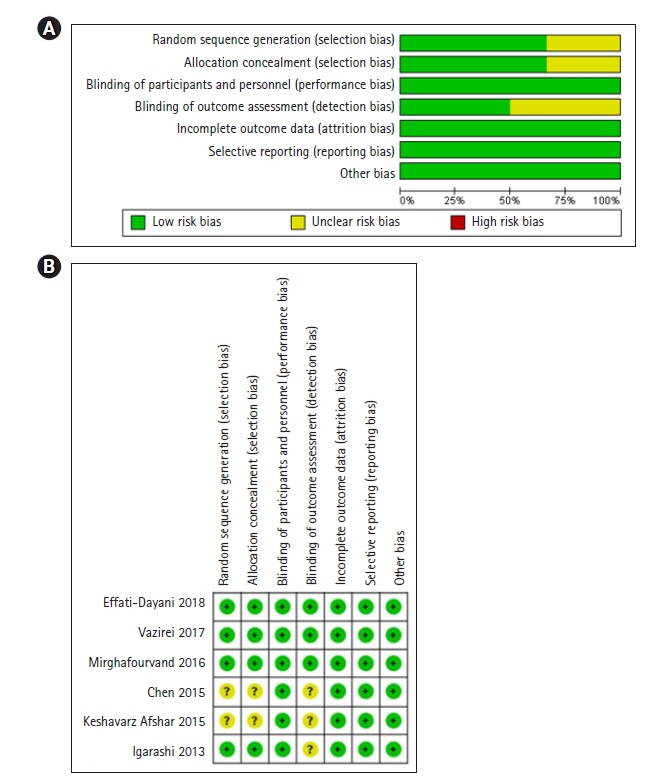
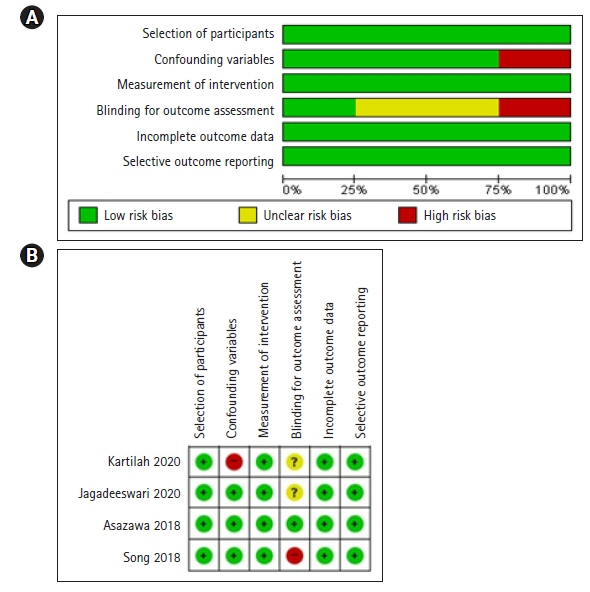
Six national and international databases were reviewed to retrieve and collect studies published up to September 7, 2021, describing randomized controlled trials and controlled clinical trials of aromatherapy interventions for prenatal and postnatal women’s fatigue. Of the 323 articles initially identified, 64 duplicates were excluded and 259 were screened. After further excluding 216 articles not related to PICO framework, 10 were selected for review. Two reviewers independently selected studies and conducted data extraction and quality appraisal using Cochran’s RoB (Risk of Bias) and RoBANS (Risk of Bias Assessment Tool for Non-randomized Studies).
Results
The quality of the 10 selected studies was overall satisfactory. A meta-analysis of three studies showed that aromatherapy with lavender oil? produced a 0.75-point reduction in postnatal mothers’ fatigue when compared to control groups. Sleep quality was also analyzed as a secondary outcome of fatigue. A meta-analysis of four studies using lavender and/or orange peel oil found that aromatherapy produced a 0.98-point improvement in postnatal mothers’ quality of sleep. Although a meta-analysis could not be conducted to synthesize the findings for fatigue in pregnant women, inhalation and massage therapy using lavender oil showed positive effects on prenatal fatigue and sleep quality.
Conclusion
Aromatherapy using lavender oil and orange peel oil is effective in improving prenatal and postnatal fatigue and sleep quality.
Keyword
Figure
Reference
-
References
1. Whitburn LY, Jones LE, Davey MA, Small R. Women’s experiences of labour pain and the role of the mind: an exploratory study. Midwifery. 2014; 30(9):1029–1035. https://doi.org/10.1016/j.midw.2014.04.005.
Article2. Salme D, Hobrani P, Salari P, Banafshe E. Fatigue in pregnancy associated with postpartum blues. J Woman. 2014; 14:7–15.3. Shobeiri F, Manoucheri B, Parsa P, Roshanaei G. Effects of counselling and sole reflexology on fatigue in pregnant women: a randomized clinical trial. J Clin Diagn Res. 2017; 11(6):QC01–QC04. https://doi.org/10.7860/JCDR/2017/22681.9972.
Article4. Cheng CY, Chou YH, Wang P, Tsai JM, Liou SR. Survey of trend and factors in perinatal maternal fatigue. Nurs Health Sci. 2015; 17(1):64–70. https://doi.org/10.1111/nhs.12149.
Article5. Cheng CY, Pickler RH. Perinatal stress, fatigue, depressive symptoms, and immune modulation in late pregnancy and one month postpartum. ScientificWorldJournal. 2014; 2014:652630. https://doi.org/10.1155/2014/652630.
Article6. Yikar SK, Nazik E. Effects of prenatal education on complaints during pregnancy and on quality of life. Patient Educ Couns. 2019; 102(1):119–125. https://doi.org/10.1016/j.pec.2018.08.023.
Article7. Tzeng YL, Yang YL, Kuo PC, Lin YC, Chen SL. Pain, anxiety, and fatigue during labor: a prospective, repeated measures study. J Nurs Res. 2017; 25(1):59–67. https://doi.org/10.1097/jnr.0000000000000165.
Article8. Andersen LB, Melvaer LB, Videbech P, Lamont RF, Joergensen JS. Risk factors for developing post-traumatic stress disorder following childbirth: a systematic review. Acta Obstet Gynecol Scand. 2012; 91(11):1261–1272. https://doi.org/10.1111/j.1600-0412.2012.01476.x.
Article9. Plancoulaine S, Flori S, Bat-Pitault F, Patural H, Lin JS, Franco P. Sleep trajectories among pregnant women and the impact on outcomes: a population-based cohort study. Matern Child Health J. 2017; 21(5):1139–1146. https://doi.org/10.1007/s10995-016-2212-9.
Article10. Hsieh CH, Chen CL, Han TJ, Lin PJ, Chiu HC. Factors influencing postpartum fatigue in vaginal-birth women: testing a path model. J Nurs Res. 2018; 26(5):332–339. https://doi.org/10.1097/jnr.0000000000000249.
Article11. Yan S, Chen J, Zhang F. Infant sleep patterns and maternal postpartum fatigue: a cross-sectional study. J Obstet Gynaecol Res. 2022; 48(5):1193–1201. https://doi.org/10.1111/jog.15191.
Article12. Okun ML. Sleep in pregnancy and the postpartum. In: Okun ML. Encyclopedia of sleep. Elsevier;2013. p. 674–679.13. Doering J, Durfor SL. The process of "persevering toward normalcy" after childbirth. MCN Am J Matern Child Nurs. 2011; 36(4):258–265. https://doi.org/10.1097/NMC.0b013e31821826e7.
Article14. Asazawa K, Kato Y, Yamaguchi A, Inoue A. The effect of aromatherapy treatment on fatigue and relaxation for mothers during the early puerperal period in Japan: a pilot study. Int J Community Based Nurs Midwifery. 2017; 5(4):365–375.15. Khayamim N, Bahadoran P, Mehrabi T. Relationship between fatigue and sleepiness with general health of mothers in the postpartum period. Iran J Nurs Midwifery Res. 2016; 21(4):385–390. https://doi.org/10.4103/1735-9066.185580.
Article16. Aksu S, Varol FG, Hotun Sahin N. Long-term postpartum health problems in Turkish women: prevalence and associations with self-rated health. Contemp Nurse. 2017; 53(2):167–181. https://doi.org/10.1080/10376178.2016.1258315.
Article17. Henderson J, Alderdice F, Redshaw M. Factors associated with maternal postpartum fatigue: an observationalstudy. BMJ Open. 2019; 9(7):e025927. https://doi.org/10.1136/bmjopen-2018-025927.
Article18. Dennis CL, Vigod S. Preventing postpartum depression: fatigue management is a place to start. Evid Based Nurs. 2020; 23(1):25. https://doi.org/10.1136/ebnurs-2019-103073.
Article19. Varney E, Buckle J. Effect of inhaled essential oils on mental exhaustion and moderate burnout: a small pilot study. J Altern Complement Med. 2013; 19(1):69–71. https://doi.org/10.1089/acm.2012.0089.
Article20. Buckle J, Ryan K, Chin KB. Clinical aromatherapy for pregnancy, labor and postpartum. Int J Childbirth Educ. 2014; 29(4):21–27.21. Farrar AJ, Farrar FC. Clinical aromatherapy. Nurs Clin North Am. 2020; 55(4):489–504. https://doi.org/10.1016/j.cnur.2020.06.015.
Article22. Karadag E, Samancioglu Baglama S. The effect of aromatherapy on fatigue and anxiety in patients undergoing hemodialysis treatment: a randomized controlled study. Holist Nurs Pract. 2019; 33(4):222–229. https://doi.org/10.1097/HNP.0000000000000334.
Article23. Farahani MA, Afsargharehbagh R, Marandi F, Moradi M, Hashemi SM, Moghadam MP, et al. Effect of aromatherapy on cancer complications: a systematic review. Complement Ther Med. 2019; 47:102169. https://doi.org/ 10.1016/j.ctim.2019.08.003.
Article24. Gok Metin Z, Ozdemir L. The effects of aromatherapy massage and reflexology on pain and fatigue in patients with rheumatoid arthritis: a randomized controlled trial. Pain Manag Nurs. 2016; 17(2):140–149. https://doi.org/10.1016/j.pmn.2016.01.004.
Article25. Park S, Park HJ. Effects of aroma hand massage on stress, fatigue, and sleep in nursing students. J Korean Acad Fundam Nurs. 2019; 26(2):86–95. https://doi.org/10.7739/jkafn.2019.26.2.86.
Article26. Hur MH, Hong JH, Yeo S. Effects of aromatherapy on stress, fructosamine, fatigue, and sleep quality in prediabetic middle-aged women: a randomised controlled trial. Eur J Integr Med. 2019; 31:100978. https://doi.org/10.1016/j.eujim.2019.100978.
Article27. Kim ME, Jun JH, Hur MH. Effects of aromatherapy on sleep quality: a systematic review and meta-analysis. J Korean Acad Nurs. 2019; 49(6):655–676. https://doi.org/10.4040/jkan.2019.49.6.655.
Article28. Coleman Smith V. Aromatherapy as a comfort measure: during the childbearing year. Int J Childbirth Educ. 2012; 27(3):26–30.29. Song J, Park MY, Jung EY. The effect of aroma hand massage on stress, fatigue and depression among mothers in the postpartum period. J Korean Soc Wellness. 2018; 13(3):389–398. https://doi.org/10.21097/ksw.2018.08.13.3.389.
Article30. Keshavarz Afshar M, Behboodi Moghadam Z, Taghizadeh Z, Bekhradi R, Montazeri A, Mokhtari P. Lavender fragrance essential oil and the quality of sleep in postpartum women. Iran Red Crescent Med J. 2015; 17(4):e25880. https://doi.org/10.5812/ircmj.17(4)2015.25880.
Article31. Effati-Daryani F, Mohammad-Alizadeh-Charandabi S, Mirghafourvand M, Taghizadeh M, Bekhradi R, Zarei S. Effect of lavender cream with or without footbath on sleep quality and fatigue in pregnancy and postpartum: a randomized controlled trial. Women Health. 2018; 58(10):1179–1191. https://doi.org/10.1080/03630242.2017.1414101.
Article32. Kianpour M, Mansouri A, Mehrabi T, Asghari G. Effect of lavender scent inhalation on prevention of stress, anxiety and depression in the postpartum period. Iran J Nurs Midwifery Res. 2016; 21(2):197–201. https://doi.org/10.4103/1735-9066.178248.
Article33. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Chichester, UK: John Wiley & Sons;2019. p. 3–640.34. Igarashi T. Physical and psychologic effects of aromatherapy inhalation on pregnant women: a randomized controlled trial. J Altern Complement Med. 2013; 19(10):805–810. https://doi.org/10.1089/acm.2012.0103.
Article35. Chen SL, Chen CH. Effects of lavender tea on fatigue, depression, and maternal-infant attachment in sleep-disturbed postnatal women. Worldviews Evid Based Nurs. 2015; 12(6):370–379. https://doi.org/10.1111/wvn.12122.
Article36. Mirghafourvand M, Charandabi SMA, Hakimi S, Khodaie L, Galeshi M. Effect of orange peel essential oil on postpartum sleep quality: a randomized controlled clinical trial. Eur J Integr Med. 2016; 8(1):62–66. https://doi.org/10.1016/j.eujim.2015.07.044.
Article37. Vaziri F, Shiravani M, Najib FS, Pourahmad S, Salehi A, Yazdanpanahi Z. Effect of lavender oil aroma in the early hours of postpartum period on maternal pains, fatigue, and mood: a randomized clinical trial. Int J Prev Med. 2017; 8:29. https://doi.org/10.4103/ijpvm.IJPVM_137_16.
Article38. Asazawa K, Kato Y, Koinuma R, Takemoto N, Tsutsui S. Effectiveness of aromatherapy treatment in alleviating fatigue and promoting relaxation of mothers during the early postpartum period. Open J Nurs. 2018; 8(3):196–209. https://doi.org/10.4236/ojn.2018.83017.
Article39. Jagadeeswari J, Soniya M. Effectiveness of aromatherapy on after pain and fatigue among postnatal mothers. Drug Interv Today. 2020; 13(7):1084–1088.40. Kartilah T, Februanti S. Effectiveness of progressive muscle relaxation and aromatherapy on fatigue in pregnant mothers. Medisains, J Ilm Ilmu-Ilmu Kesehat. 2020; 18(1):14–18. https://doi.org/10.30595/medisains.v18i1.6421.
Article41. Rezaie-Keikhaie K, Hastings-Tolsma M, Bouya S, Shad FS, Sari M, Shoorvazi M, et al. Effect of aromatherapy on post-partum complications: a systematic review. Complement Ther Clin Pract. 2019; 35:290–295. https://doi.org/ 10.1016/j.ctcp.2019.03.010.
Article42. Ali B, Al-Wabel NA, Shams S, Ahamad A, Khan SA, Anwar F. Essential oils used in aromatherapy: a systemic review. Asian Pac J Trop Biomed. 2015; 5(8):601–611. https://doi.org/10.1016/j.apjtb.2015.05.007.
Article43. Koulivand PH, Khaleghi Ghadiri M, Gorji A. Lavender and the nervous system. Evid Based Complementary Altern Med. 2013; 2013:681304. https://doi.org/10.1155/2013/681304.
Article44. Tsai SS, Wang HH, Chou FH. The effects of aromatherapy on postpartum women: a systematic review. J Nurs Res. 2020; 28(3):e96. https://doi.org/10.1097/jnr.0000000000000331.
Article45. Fujita K, Chavasiri W, Kubo I. Anti-salmonella activity of volatile compounds of Vietnam coriander. Phytother Res. 2015; 29(7):1081–1087. https://doi.org/10.1002/ptr.5351.
Article46. Faydalı S, Çetinkaya F. The effect of aromatherapy on sleep quality of elderly people residing in a nursing home. Holist Nurs Pract. 2018; 32(1):8–16. https://doi.org/10.1097/HNP.0000000000000244.
Article47. Arbianingsih A, Amal AA, Hidayah N, Azhari N, Tahir T. Massage with lavender aromatherapy reduced sleep disturbances on infant. Enfermería Clínica. 2020; 30(3):62–65. https://doi.org/10.1016/j.enfcli.2019.12.028.
Article48. Dos Reis Lucena L, Dos Santos-Junior JG, Tufik S, Hachul H. Lavender essential oil on postmenopausal women with insomnia: double-blind randomized trial. Complement Ther Med. 2021; 59:102726. https://doi.org/10.1016/j.ctim.2021.102726.
Article49. Dobetsberger C, Buchbauer G. Actions of essential oils on the central nervous system: an updated review. Flavour Fragr J. 2011; 26(5):300–316. https://doi.org/10.1002/ffj.2045.
Article50. Ngo-Mback MN, Babii C, Jazet Dongmo PM, Kouipou Toghueo MR, Stefan M, Fekam Boyom F. Anticandidal and synergistic effect of essential oil fractions from three aromatic plants used in Cameroon. J Mycol Med. 2020; 30(2):100940. https://doi.org/10.1016/j.mycmed.2020.100940.
Article51. Tsai SY, Lin JW, Kuo LT, Thomas KA. Daily sleep and fatigue characteristics in nulliparous women during the third trimester of pregnancy. Sleep. 2012; 35(2):257–262. https://doi.org/10.5665/sleep.1634.
Article52. Mascarenhas VHA, Caroci-Becker A, Riesco ML. Effectiveness of aromatherapy versus standard care on physiological and psychological symptoms in pregnant women: a systematic review protocol. JBI Evid Synth. 2021; 20(2):658–665. https://doi.org/10.11124/JBIES-20-00562.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Aromatherapy Program on Depression and Fatigue in Middle Aged Women
- A Systematic Review of the Effects of Aromatherapy on Depression and Anxiety in Postmenopausal Women
- Aromatherapy for Sexual Problems in Menopausal Women: A Systematic Review and Meta-analysis
- Effects of Aromatherapy on Sleep Quality: A Systematic Review and Meta-Analysis
- Is aromatherapy associated with patient’s dental anxiety levels? A systematic review and meta-analysis