Anesth Pain Med.
2022 Jul;17(3):249-255. 10.17085/apm.22163.
Ventilation through a straw
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2535316
- DOI: http://doi.org/10.17085/apm.22163
Abstract
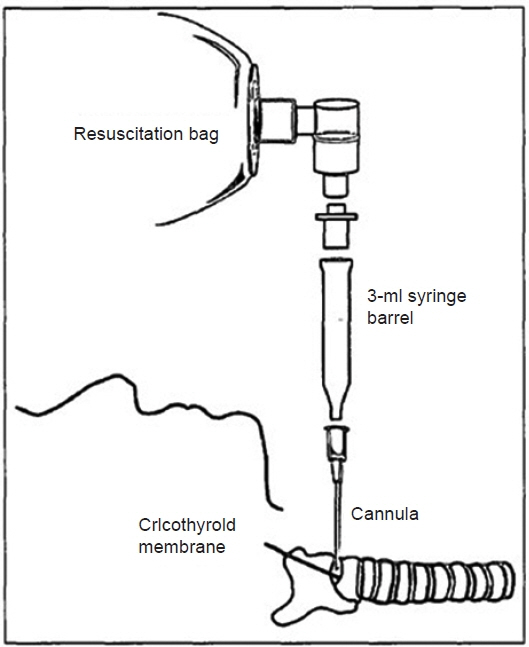
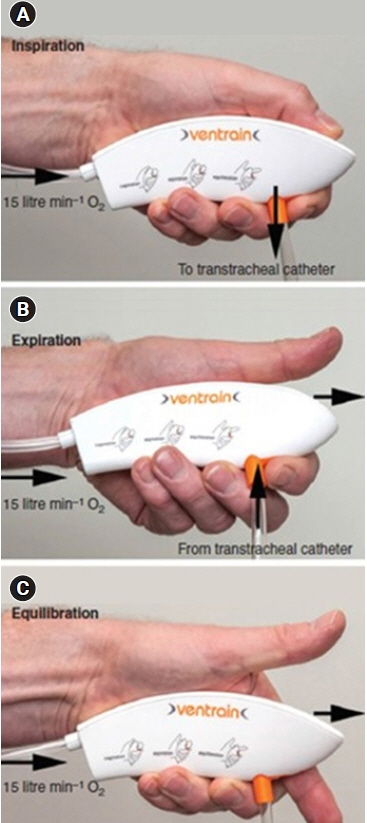
- Transtracheal jet ventilation can be used for resuscitation of partial airway obstruction. A prerequisite for jet ventilation is that at least a minimum airway opening for gas escape must be secured. Therefore, another option should be considered in cases of complete airway obstruction. The following methods or devices has been used under cricothyrotomy using an intravenous cannula: 1) Ambu (bag valve mask) bagging, 2) Ventrain® , 3) Rapid-O2 oxygen insufflation device (Rapid-O2), and 4) jet ventilation using a dual lumen catheter. During Ambu bagging, extraordinarily high insufflation pressure is required to force oxygen through the cannula. When using a 12-G cannula, long and slow positive-pressure ventilations (10–12 breaths/min) are required, which makes it extremely difficult to compress the bag. Therefore, a 10-G or larger is recommended. Ventrain® is an expiratory assist device capable of forcibly expelling insufflated oxygen through a transtracheal cannula. It is recommended to adjust the inspiratory and expiratory times while observing the chest wall movements. Rapid-O2 is a rescue oxygenation device with adequate ventilation of less importance; therefore, the resulting hypercarbia is inevitable. A 14-G cannula is used. Lastly, jet ventilation using a dual-lumen catheter with a 16-G inflow lumen and 10-G outflow lumen was used to obtain both oxygenation and ventilation. However, the addition of the outer diameters of 16-G and 10-G results in an outer diameter of 5.1 mm, which is too large to puncture the cricothyroid membrane. In conclusion, Ventrain® is considered the most ideal device for use among the devices developed to date.
Figure
Reference
-
1. Frumin MJ, Epstein RM, Cohen G. Apneic oxygenation in man. Anesthesiology. 1959; 20:789–98.
Article2. Patel A, Nouraei SA. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015; 70:323–9.
Article3. Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult Airway Society Intubation Guidelines Working Group. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015; 115:827–48.4. Yealy DM, Stewart RD, Kaplan RM. Clarifications on translaryngeal ventilation. Ann Emerg Med. 1988; 17:1130.
Article5. Neff CC, Pfister RC, Van Sonnenberg E. Percutaneous transtracheal ventilation: experimental and practical aspects. J Trauma. 1983; 23:84–90.6. Hooker EA, Danzl DF, O'Brien D, Presley M, Whitaker G, Sharp MK. Percutaneous transtracheal ventilation: resuscitation bags do not provide adequate ventilation. Prehosp Disaster Med. 2006; 21:431–5.
Article7. Coté CJ, Eavey RD, Todres ID, Jones DE. Cricothyroid membrane puncture: oxygenation and ventilation in a dog model using an intravenous catheter. Crit Care Med. 1988; 16:615–9.8. Marx JA, Hockberger RS, Walls RM, Adams J, Rosen P, et al. Rosen's emergency medicine: concepts and clinical practice. 5th ed. St. Louis: Mosby;2002. p. 18.9. Hamaekers AE, Borg PA, Götz T, Enk D. Ventilation through a small-bore catheter: optimizing expiratory ventilation assistance. Br J Anaesth. 2011; 106:403–9.
Article10. Hamaekers AE, Borg PA, Enk D. Ventrain: an ejector ventilator for emergency use. Br J Anaesth. 2012; 108:1017–21.
Article11. Schmidt AR, Ruetzler K, Haas T, Schmitz A, Weiss M. Impact of oxygen sources on performance of the Ventrain(®) ventilation device in an in vitro set-up. Acta Anaesthesiol Scand. 2016; 60:241–9.12. Hamaekers AE, van der Beek T, Theunissen M, Enk D. Rescue ventilation through a small-bore transtracheal cannula in severe hypoxic pigs using expiratory ventilation assistance. Anesth Analg. 2015; 120:890–4.
Article13. Borg PA, Hamaekers AE, Lacko M, Jansen J, Enk D. Ventrain® for ventilation of the lungs. Br J Anaesth. 2012; 109:833–4.
Article14. Willemsen MG, Noppens R, Mulder AL, Enk D. Ventilation with the Ventrain through a small lumen catheter in the failed paediatric airway: two case reports. Br J Anaesth. 2014; 112:946–7.
Article15. Morrison S, Aerts S, Van Rompaey D, Vanderveken O. Failed awake intubation for critical airway obstruction recued with the Ventrain device and an Arndt exchange catheter: A case report. A A Pract. 2019; 13:23–6.16. Insufflation device RAPID O2. Meditech Systems Limited [Internet]. Available from https://www.meditechsystems.co.uk/product/insufflation-device-rapid-o2/.17. Heard A. Percutaneous emergency oxygenation strategies in the “Can’t Intubate, Can’t Oxygenate” scenario. Smashwords edition; 2013. Available from https://www.smashwords.com/books/view/377530.18. Heard AM, Green RJ, Eakins P. The formulation and introduction of a 'can't intubate, can't ventilate' algorithm into clinical practice. Anaesthesia. 2009; 64:601–8.
Article19. Wexler S, Prineas SN, Suharto TA. Transtracheal flow-regulated oxygen insufflation-a simple and safe method for prolonging safe apnoea time in difficult airway management: a report of two cases. Anaesth Intensive Care. 2019; 47:553–60.
Article20. Dworkin R, Benumof JL, Benumof R, Karagianes TG. The effective tracheal diameter that causes air trapping during jet ventilation. J Cardiothorac Anesth. 1990; 4:731–6.
Article21. Rone CA, Pavlin EG, Cummings CW, Weymuller EA. Studies in transtracheal ventilation catheters. Laryngoscope. 1982; 92:1259–64.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bioconversion of Straw into Improved Fodder: Preliminary Treatment of Rice Straw Using Mechanical, Chemical and/or Gamma Irradiation
- Bioconversion of Straw Into Improved Fodder: Mycoprotein Production and Cellulolytic Acivity of Rice Straw Decomposing Fungi
- Using of a Straw as Liposuction Protector at the Treatment of Osmidrosis
- Bioconversion of Straw into Improved Fodder: Fungal Flora Decomposing Rice Straw
- The Comparative Study of Central Venous Pressure Measurements during Mechanical Ventilation and after Disconnection of Ventilation