J Liver Cancer.
2022 Sep;22(2):188-193. 10.17998/jlc.2022.08.17.
Hepatocellular carcinoma diagnosed in a patient who had Fontan operation 30 years ago: a case report
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Pathology, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2534246
- DOI: http://doi.org/10.17998/jlc.2022.08.17
Abstract
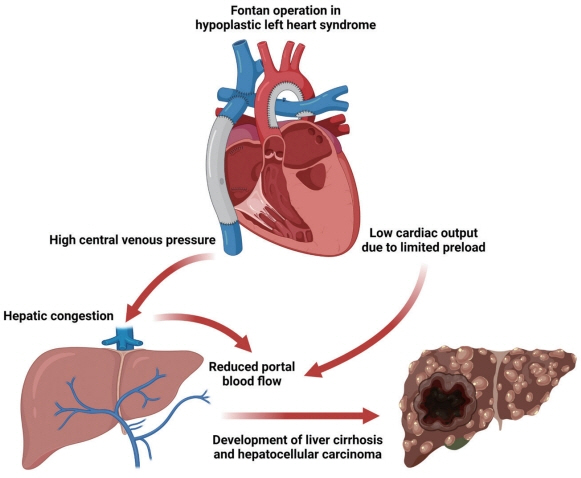
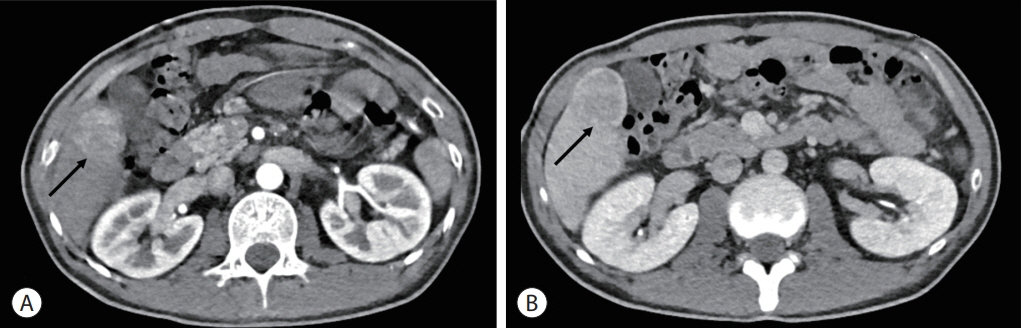
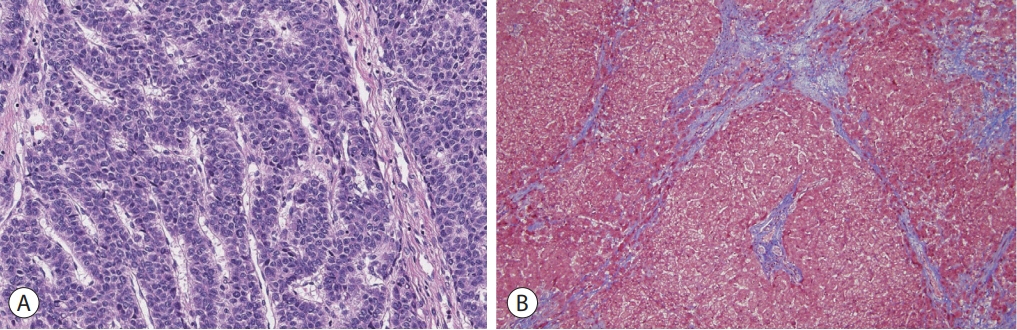
- The Fontan operation is performed in patients with a single ventricle. As the systemic venous return is directly connected to the pulmonary circulation during this procedure, chronic hepatic congestion is induced, leading to Fontan-associated liver disease (FALD) including liver cirrhosis and hepatocellular carcinoma (HCC). In this report, we present a case of HCC diagnosed in a patient who underwent the Fontan operation 30 years ago. The patient underwent regular surveillance for FALD, which revealed a 4 cm-sized hepatic mass with elevated serum alpha-fetoprotein. After surgical treatment, there was no evidence of HCC recurrence during 3 years of follow-up. As the risk of HCC and Fontan-associated liver cirrhosis increases with the duration elapsed since the operation, regular surveillance should be emphasized. Serial follow-up of serum alpha-fetoprotein levels and abdominal imaging are necessary to achieve early and accurate diagnosis of HCC in post-Fontan patients.
Figure
Reference
-
1. Fontan F, Baudet E. Surgical repair of tricuspid atresia. Thorax. 1971; 26:240–248.2. Gewillig M. The Fontan circulation. Heart. 2005; 91:839–846.3. Gordon-Walker TT, Bove K, Veldtman G. Fontan-associated liver disease: a review. J Cardiol. 2019; 74:223–232.4. Munsterman ID, Duijnhouwer AL, Kendall TJ, Bronkhorst CM, Ronot M, van Wettere M, et al. The clinical spectrum of Fontanassociated liver disease: results from a prospective multimodality screening cohort. Eur Heart J. 2019; 40:1057–1068.5. Yoon JS, Lee DH, Cho EJ, Song MK, Choi YH, Kim GB, et al. Risk of liver cirrhosis and hepatocellular carcinoma after Fontan operation: a need for surveillance. Cancers (Basel). 2020; 12:1805.6. Gersony WM. Fontan operation after 3 decades: what we have learned. Circulation. 2008; 117:13–15.7. Khairy P, Fernandes SM, Mayer JE Jr, Triedman JK, Walsh EP, Lock JE, et al. Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery. Circulation. 2008; 117:85–92.8. Emamaullee J, Zaidi AN, Schiano T, Kahn J, Valentino PL, Hofer RE, et al. Fontan-associated liver disease: screening, management, and transplant considerations. Circulation. 2020; 142:591–604.9. Olsen AL, Bloomer SA, Chan EP, Gaça MD, Georges PC, Sackey B, et al. Hepatic stellate cells require a stiff environment for myofibroblastic differentiation. Am J Physiol Gastrointest Liver Physiol. 2011; 301:G110–G118.10. Iwakiri Y, Shah V, Rockey DC. Vascular pathobiology in chronic liver disease and cirrhosis - current status and future directions. J Hepatol. 2014; 61:912–924.11. Baek JS, Bae EJ, Ko JS, Kim GB, Kwon BS, Lee SY, et al. Late hepatic complications after Fontan operation; non-invasive markers of hepatic fibrosis and risk factors. Heart. 2010; 96:1750–1755.12. Shimizu M, Miyamoto K, Nishihara Y, Izumi G, Sakai S, Inai K, et al. Risk factors and serological markers of liver cirrhosis after Fontan procedure. Heart Vessels. 2016; 31:1514–1521.13. Asrani SK, Warnes CA, Kamath PS. Hepatocellular carcinoma after the Fontan procedure. N Engl J Med. 2013; 368:1756–1757.14. Yamada K, Shinmoto H, Kawamura Y, Wakamatsu H, Kawauchi T, Soga S, et al. Transarterial embolization for pediatric hepatocellular carcinoma with cardiac cirrhosis. Pediatr Int. 2015; 57:766–770.15. Kogiso T, Tokushige K. Fontan-associated liver disease and hepatocellular carcinoma in adults. Sci Rep. 2020; 10:21742.16. Possner M, Gordon-Walker T, Egbe AC, Poterucha JT, Warnes CA, Connolly HM, et al. Hepatocellular carcinoma and the Fontan circulation: clinical presentation and outcomes. Int J Cardiol. 2021; 322:142–148.17. Rodriguez De Santiago E, Téllez L, Guerrero A, Albillos A. Hepatocellular carcinoma after Fontan surgery: a systematic review. Hepatol Res. 2021; 51:116–134.18. Egbe AC, Poterucha JT, Warnes CA, Connolly HM, Baskar S, Ginde S, et al. Hepatocellular carcinoma after Fontan operation: multicenter case series. Circulation. 2018; 138:746–748.19. Asrani SK, Asrani NS, Freese DK, Phillips SD, Warnes CA, Heimbach J, et al. Congenital heart disease and the liver. Hepatology. 2012; 56:1160–1169.20. Wells ML, Hough DM, Fidler JL, Kamath PS, Poterucha JT, Venkatesh SK. Benign nodules in post-Fontan livers can show imaging features considered diagnostic for hepatocellular carcinoma. Abdom Radiol (NY). 2017; 42:2623–2631.21. Wells ML, Fenstad ER, Poterucha JT, Hough DM, Young PM, Araoz PA, et al. Imaging findings of congestive hepatopathy. Radiographics. 2016; 36:1024–1037.22. Nandwana SB, Olaiya B, Cox K, Sahu A, Mittal P. abdominal imaging surveillance in adult patients after fontan procedure: risk of chronic liver disease and hepatocellular carcinoma. Curr Probl Diagn Radiol. 2018; 47:19–22.23. Téllez L, Rodríguez de Santiago E, Minguez B, Payance A, Clemente A, Baiges A, et al. Prevalence, features and predictive factors of liver nodules in Fontan surgery patients: The VALDIG Fonliver prospective cohort. J Hepatol. 2020; 72:702–710.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver transplantation in an adult patient with hepatocellular carcinoma following liver cirrhosis as a complication of the Fontan procedure -A case report-
- The Extracardiac Fontan Operation in Adult: A case report
- Unusual Semimembranosus Muscle Metastasis from Hepatocellular Carcinoma
- clinical Evaluation for the Progrosis after the Fontan Operation
- Treatment of Protein-losing Enteropathy After Fontan Procedure by Conversion to the Total Cavopulmonary Connection with Fenestration