Cancer Res Treat.
2022 Oct;54(4):996-1004. 10.4143/crt.2021.902.
The Value of the Illness-Death Model for Predicting Outcomes in Patients with Non–Small Cell Lung Cancer
- Affiliations
-
- 1Department of Radiology, Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- 2Department of Statistics and Institute of Applied Statistics, Jeonbuk National University, Jeonju, Korea
- 3Department of Radiology, Chonnam National University Hwasun Hospital, Hwasun, Korea
- 4Department of Applied Statistics, University of Suwon, Hwaseong, Korea
- KMID: 2534179
- DOI: http://doi.org/10.4143/crt.2021.902
Abstract
- Purpose
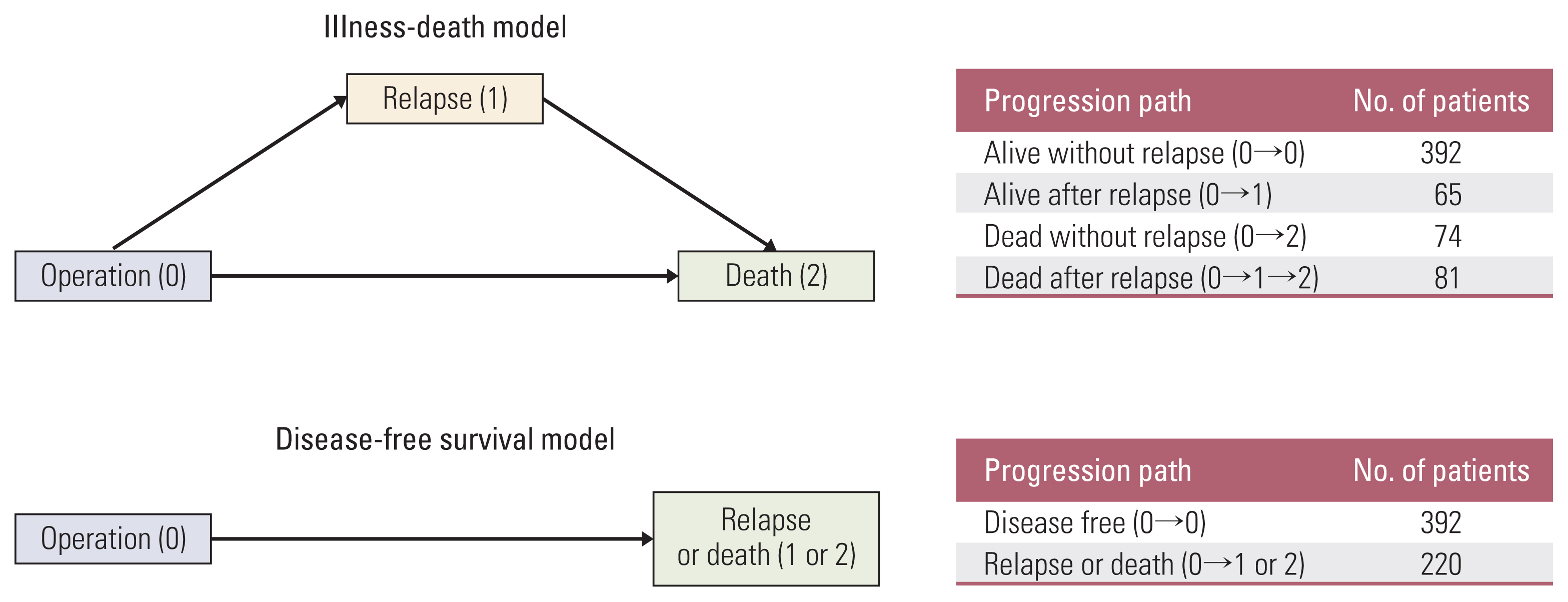
The illness-death model (IDM) is a comprehensive approach to evaluate the relationship between relapse and death. This study aimed to illustrate the value of the IDM for identifying risk factors and evaluating predictive probabilities for relapse and death in patients with non–small cell lung cancer (NSCLC) in comparison with the disease-free survival (DFS) model.
Materials and Methods
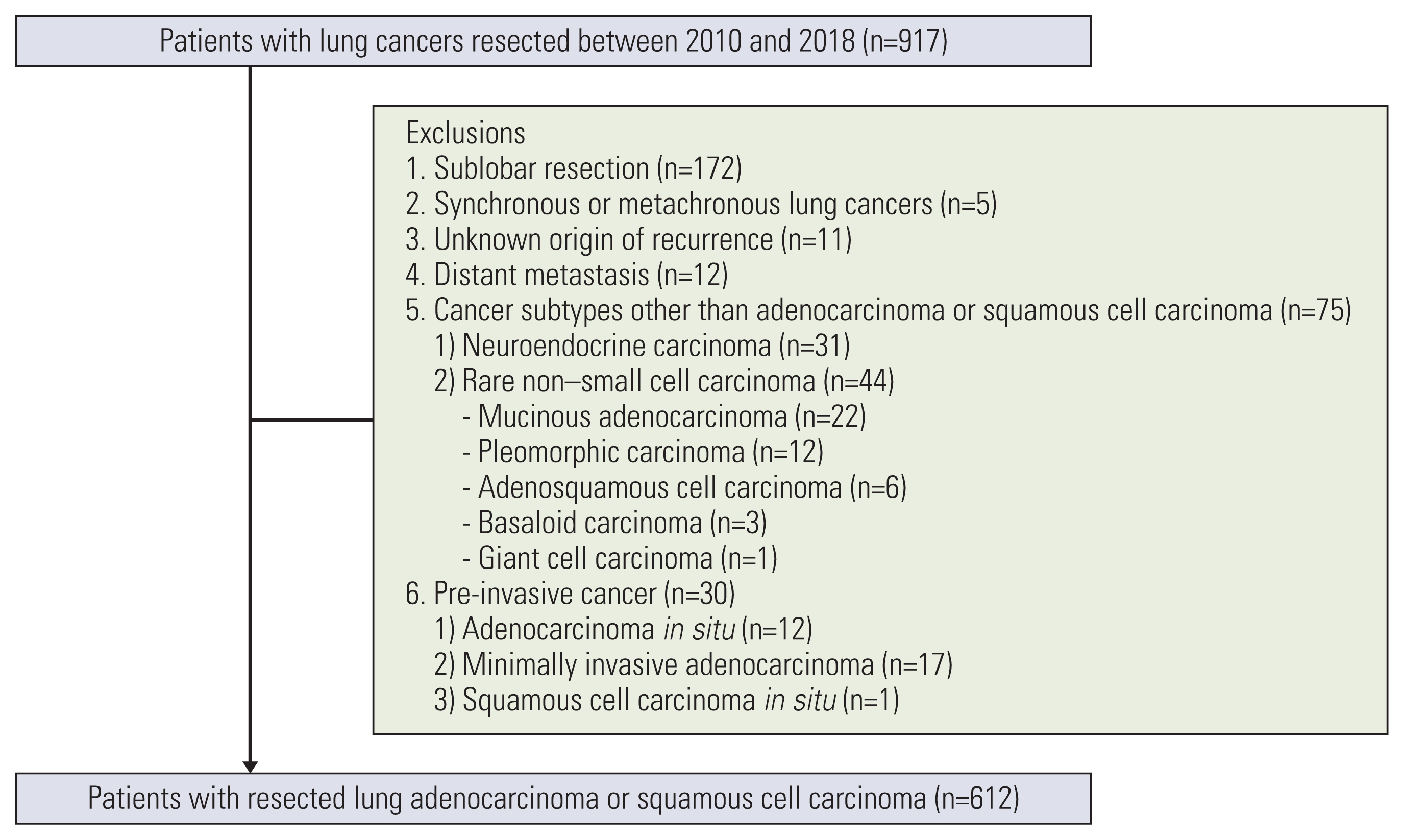
We retrospectively analyzed 612 NSCLC patients who underwent a curative operation. Using the IDM, the risk factors and predictive probabilities for relapse, death without relapse, and death after relapse were simultaneously evaluated and compared to those obtained from a DFS model.
Results
The IDM provided more detailed risk factors according to the patient’s disease course, including relapse, death without relapse, and death after relapse, in patients with resected lung cancer. In the IDM, history of malignancy (other than lung cancer) was related to relapse and smoking history was associated with death without relapse; both were indistinguishable in the DFS model. In addition, the IDM was able to evaluate the predictive probability and risk factors for death after relapse; this information could not be obtained from the DFS model.
Conclusion
Compared to the DFS model, we found that the IDM provides more comprehensive information on transitions between states and disease stages and provides deeper insights with respect to understanding the disease process among lung cancer patients.
Figure
Reference
-
References
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021; 71:7–33.2. Mitsudomi T, Suda K, Yatabe Y. Surgery for NSCLC in the era of personalized medicine. Nat Rev Clin Oncol. 2013; 10:235–44.3. Zappa C, Mousa SA. Non-small cell lung cancer: current treatment and future advances. Transl Lung Cancer Res. 2016; 5:288–300.4. Uramoto H, Tanaka F. Recurrence after surgery in patients with NSCLC. Transl Lung Cancer Res. 2014; 3:242–9.5. Brundage MD, Davies D, Mackillop WJ. Prognostic factors in non-small cell lung cancer: a decade of progress. Chest. 2002; 122:1037–57.6. Fine JP, Jiang H, Chappell R. On semi-competing risks data. Biometrika. 2001; 88:907–19.7. Wang W. Estimating the association parameter for Copula models under dependent censoring. J R Stat Soc Series B Stat Methodol. 2003; 65:257–73.8. Xu J, Kalbfleisch JD, Tai B. Statistical analysis of illness-death processes and semicompeting risks data. Biometrics. 2010; 66:716–25.9. Travis WD, Asamura H, Bankier AA, Beasley MB, Detterbeck F, Flieder DB, et al. The IASLC Lung Cancer Staging Project: proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol. 2016; 11:1204–23.10. Anderson-Bergman C. icenReg: regression models for interval censored data in R. J Stat Softw. 2017; 81:1–23.11. Touraine C, Gerds TA, Joly P. SmoothHazard: an R package for fitting regression models to interval-censored observations of illness-death models. J Stat Softw. 2017; 79:1–22.12. Meier-Hirmer C, Schumacher M. Multi-state model for studying an intermediate event using time-dependent covariates: application to breast cancer. BMC Med Res Methodol. 2013; 13:80.13. Alafchi B, Roshanaei G, Tapak L, Abbasi M, Mahjub H. Joint modelling of colorectal cancer recurrence and death after resection using multi-state model with cured fraction. Sci Rep. 2021; 11:1016.14. Putter H, van der Hage J, de Bock GH, Elgalta R, van de Velde CJ. Estimation and prediction in a multi-state model for breast cancer. Biom J. 2006; 48:366–80.15. Hajihosseini M, Faradmal J, Sadighi-Pashaki A. Survival analysis of breast cancer patients after surgery with an intermediate event: application of illness-death model. Iran J Public Health. 2015; 44:1677–84.16. Eulenburg C, Mahner S, Woelber L, Wegscheider K. A systematic model specification procedure for an illness-death model without recovery. PLoS One. 2015; 10:e0123489.17. Sekihara K, Hishida T, Yoshida J, Oki T, Omori T, Katsumata S, et al. Long-term survival outcome after postoperative recurrence of non-small-cell lung cancer: who is ‘cured’ from postoperative recurrence? Eur J Cardiothorac Surg. 2017; 52:522–8.18. Shimada Y, Saji H, Yoshida K, Kakihana M, Honda H, Nomura M, et al. Prognostic factors and the significance of treatment after recurrence in completely resected stage I non-small cell lung cancer. Chest. 2013; 143:1626–34.19. Choi PJ, Jeong SS, Yoon SS. Prediction and prognostic factors of post-recurrence survival in recurred patients with early-stage NSCLC who underwent complete resection. J Thorac Dis. 2016; 8:152–60.20. Keiding N, Klein JP, Horowitz MM. Multi-state models and outcome prediction in bone marrow transplantation. Stat Med. 2001; 20:1871–85.21. Touraine C, Helmer C, Joly P. Predictions in an illness-death model. Stat Methods Med Res. 2016; 25:1452–70.22. Andersen PK, Pohar Perme M. Inference for outcome probabilities in multi-state models. Lifetime Data Anal. 2008; 14:405–31.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Alterations of the Apoptosis Genes and Their Products in Non-small Cell Lung Cancer Tissues
- Druggable Targets of Squamous Cell Lung Cancer
- Cell Death Induction Mechanism of Non-small Cell Lung Cancer Cell Line, NCI-H1703 by Docetaxel
- Immunotherapy for Non-small-cell Lung Cancer: Current Status and Future Obstacles
- The Incidence Rate and Severity of Orthotopic Lung Cancer in an Animal Model Depends on the Number of A549 Cells and Transplantation Period