Ann Surg Treat Res.
2022 Oct;103(4):244-251. 10.4174/astr.2022.103.4.244.
Unroofing curettage for treatment of simple and complex sacrococcygeal pilonidal disease
- Affiliations
-
- 1Department of Surgery, University of Health Science, Diskapi Yildirim Beyazit Training and Research Hospital, Ankara, Turkey
- 2Department of Surgery, University of Health Science, Konya City Hospital, Konya, Turkey
- KMID: 2534130
- DOI: http://doi.org/10.4174/astr.2022.103.4.244
Abstract
- Purpose
Sacrococcygeal pilonidal disease is a chronic inflammatory condition with an incidence of 26:100,000 in the United States. However, its etiology and optimal treatment remain controversial.
Methods
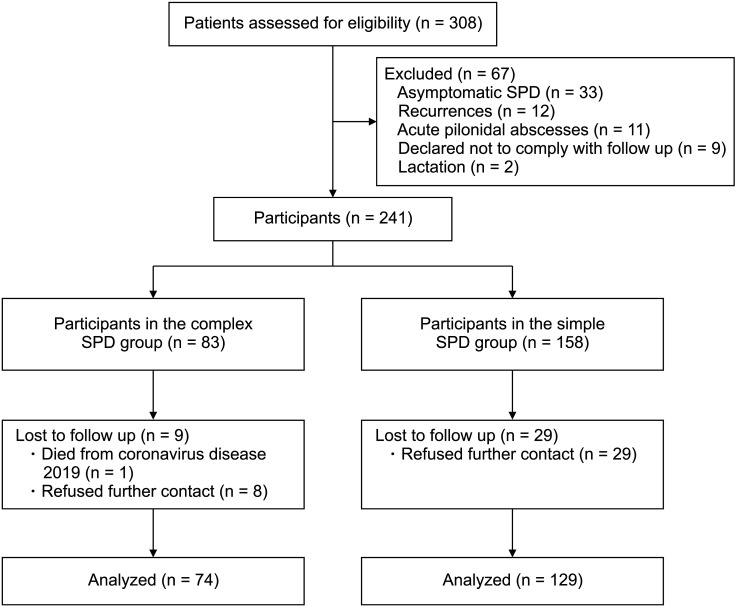
We included 129 and 74 patients with simple and complex sacrococcygeal pilonidal disease, respectively. The primary outcome was pilonidal sinus recurrence after unroofing curettage. Secondary outcomes were pain scores, time to return to work/school, and time to complete recovery.
Results
At a median follow-up of 53 months, the recurrence rate was 4.9% in all patients, not significantly higher in subjects with the complex disease. Duration of surgery (15.4 minutes vs. 12.2 minutes), time to return to school/work (9.8 days vs. 7.7 days), and complete healing time (44 days vs. 36 days) were longer in patients with the complex disease. Postoperative complication rates, pain scores, and quality of life scores between the 2 groups did not differ.
Conclusion
Unroofing curettage may be a good first-choice treatment for both simple and complex sacrococcygeal pilonidal disease.
Keyword
Figure
Reference
-
1. Mayo OH. Observations on injuries and diseases of the rectum. London: Burgess and Hill;1883. p. 45–46.2. Steele SR, Perry WB, Mills S, Buie WD. Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of pilonidal disease. Dis Colon Rectum. 2013; 56:1021–1027. PMID: 23929010.
Article3. Beal EM, Lee MJ, Hind D, Wysocki AP, Yang F, Brown SR. A systematic review of classification systems for pilonidal sinus. Tech Coloproctol. 2019; 23:435–443. PMID: 31098861.
Article4. Gecim IE, Goktug UU, Celasin H. Endoscopic pilonidal sinus treatment combined with crystalized phenol application may prevent recurrence. Dis Colon Rectum. 2017; 60:405–407. PMID: 28267008.
Article5. Harries RL, Alqallaf A, Torkington J, Harding KG. Management of sacrococcygeal pilonidal sinus disease. Int Wound J. 2019; 16:370–378. PMID: 30440104.
Article6. Kepenekci I, Demirkan A, Celasin H, Gecim IE. Unroofing and curettage for the treatment of acute and chronic pilonidal disease. World J Surg. 2010; 34:153–157. PMID: 19820992.
Article7. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370:1453–1457. PMID: 18064739.
Article8. Tezel E. A new classification according to navicular area concept for sacrococcygeal pilonidal disease. Colorectal Dis. 2007; 9:575–576. PMID: 17573759.
Article9. Sahin A, Simsek G, Arslan K. Unroofing curettage versus modified limberg flap in pilonidal disease: a retrospective cohort study. Dis Colon Rectum. 2022; 65:1241–1250. PMID: 34840296.
Article10. Calikoglu I, Gulpinar K, Oztuna D, Elhan AH, Dogru O, Akyol C, et al. Phenol injection versus excision with open healing in pilonidal disease: a prospective randomized trial. Dis Colon Rectum. 2017; 60:161–169. PMID: 28059912.
Article11. Stauffer VK, Luedi MM, Kauf P, Schmid M, Diekmann M, Wieferich K, et al. Common surgical procedures in pilonidal sinus disease: a meta-analysis, merged data analysis, and comprehensive study on recurrence. Sci Rep. 2018; 8:3058. PMID: 29449548.
Article12. McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008; 336:868–871. PMID: 18390914.
Article13. Karakayali F, Karagulle E, Karabulut Z, Oksuz E, Moray G, Haberal M. Unroofing and marsupialization vs. rhomboid excision and Limberg flap in pilonidal disease: a prospective, randomized, clinical trial. Dis Colon Rectum. 2009; 52:496–502. PMID: 19333052.
Article14. Gencosmanoglu R, Inceoglu R. Modified lay-open (incision, curettage, partial lateral wall excision and marsupialization) versus total excision with primary closure in the treatment of chronic sacrococcygeal pilonidal sinus: a prospective, randomized clinical trial with a complete two-year follow-up. Int J Colorectal Dis. 2005; 20:415–422. PMID: 15714292.
Article15. Garg P, Menon GR, Gupta V. Laying open (deroofing) and curettage of sinus as treatment of pilonidal disease: a systematic review and meta-analysis. ANZ J Surg. 2016; 86:27–33. PMID: 26612320.
Article16. Garg P, Garg M, Gupta V, Mehta SK, Lakhtaria P. Laying open (deroofing) and curettage under local anesthesia for pilonidal disease: an outpatient procedure. World J Gastrointest Surg. 2015; 7:214–218. PMID: 26425271.
Article17. Abbas MA, Tejerian T. Unroofing and marsupialization should be the first procedure of choice for most pilonidal disease. Dis Colon Rectum. 2006; 49:1242. PMID: 16826329.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pilonidal Cysts Occurring in the Sacrococcygeal Region and that were Misdiagnosed as a Simple Abscess
- A Case of Pilonidal Sinus Mimicking Inflammatory Epidermal Cyst
- Wide Excision Using Indigo-Carmine to Minimize the Recurrence of a Pilonidal Cyst: Technical Note
- Pilonidal Abscess Associated With Primary Actinomycosis
- Surgical Excision and Postoperative IPL Epilation for Preventing Recurrence of Pilonidal Sinus