J Pathol Transl Med.
2022 Sep;56(5):289-293. 10.4132/jptm.2022.08.02.
Evaluation of the characteristics of multiple human papillomavirus (HPV) infections identified using the BD Onclarity HPV assay and comparison with those of single HPV infection
- Affiliations
-
- 1Department of Pathology, School of Medicine, Kyungpook National University, Kyungpook National University Chilgok Hospital, Daegu, Korea
- KMID: 2533705
- DOI: http://doi.org/10.4132/jptm.2022.08.02
Abstract
- Background
Human papillomavirus (HPV) infection is a major cause of cervical cancer and associated precursor lesions. Multiple HPV genotype infections have been reported. However, their clinicopathological characteristics still remain elusive.
Methods
For this study, 814 consecutive patients who had undergone colposcopy and HPV genotyping test using BD Onclarity HPV assay were retrospectively selected. Clinicopathological parameters of multiple HPV infections were compared with those of single HPV infection.
Results
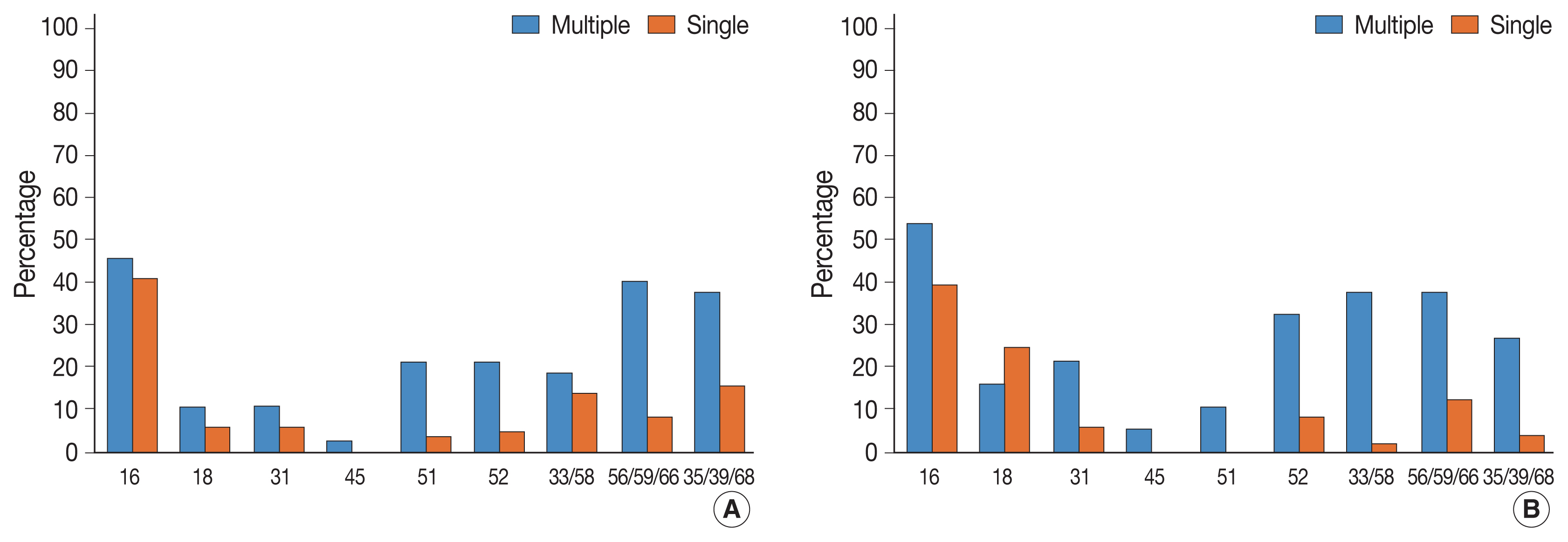
Multiple HPV infections were found in 110 out of 814 cases (13.5%). Multiple HPV infections were associated with a significantly higher incidence of high-grade intraepithelial lesions (HSILs) compared with single HPV infection. Other high-risk HPV genotypes, in addition to HPV 16, were found more frequently in the multiple HPV infections group; these included HPV 51, 52, 33/58, 56/59/66, and 35/39/68. No specific coinfection pattern was not identified. Additionally, the number of HPV genotypes in multiple HPV infections was not associated with the progression to HSIL or squamous cell carcinoma.
Conclusions
Multiple HPV infections have distinct clinicopathological characteristics (compared with single HPV infection). As their biological behavior is uncertain, close and frequent follow-up is warranted.
Keyword
Figure
Reference
-
References
1. Woodman CB, Collins SI, Young LS. The natural history of cervical HPV infection: unresolved issues. Nat Rev Cancer. 2007; 7:11–22.
Article2. Abreu AL, Souza RP, Gimenes F, Consolaro ME. A review of methods for detect human papillomavirus infection. Virol J. 2012; 9:262.3. Munoz N, Bosch FX, de Sanjose S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003; 348:518–27.
Article4. Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999; 189:12–9.
Article5. de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H. Classification of papillomaviruses. Virology. 2004; 324:17–27.
Article6. Van Doorslaer K, Li Z, Xirasagar S, et al. The papillomavirus episteme: a major update to the papillomavirus sequence database. Nucleic Acids Res. 2017; 45:D499–506.
Article7. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. 2007; 90:1–636.8. de Sanjose S, Quint WG, Alemany L, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010; 11:1048–56.9. Munagala R, Dona MG, Rai SN, et al. Significance of multiple HPV infection in cervical cancer patients and its impact on treatment response. Int J Oncol. 2009; 34:263–71.
Article10. Dickson EL, Vogel RI, Geller MA, Downs LS Jr. Cervical cytology and multiple type HPV infection: a study of 8182 women ages 31–65. Gynecol Oncol. 2014; 133:405–8.
Article11. Soto-De Leon S, Camargo M, Sanchez R, et al. Distribution patterns of infection with multiple types of human papillomaviruses and their association with risk factors. PLoS One. 2011; 6:e14705.
Article12. Cuschieri KS, Cubie HA, Whitley MW, et al. Multiple high risk HPV infections are common in cervical neoplasia and young women in a cervical screening population. J Clin Pathol. 2004; 57:68–72.
Article13. Lee SA, Kang D, Seo SS, et al. Multiple HPV infection in cervical cancer screened by HPVDNAChip. Cancer Lett. 2003; 198:187–92.
Article14. Oyervides-Munoz MA, Perez-Maya AA, Sanchez-Dominguez CN, et al. Multiple HPV infections and viral load association in persistent cervical lesions in Mexican women. Viruses. 2020; 12:380.
Article15. De Brot L, Pellegrini B, Moretti ST, et al. Infections with multiple high-risk HPV types are associated with high-grade and persistent low-grade intraepithelial lesions of the cervix. Cancer Cytopathol. 2017; 125:138–43.
Article16. Salazar KL, Zhou HS, Xu J, et al. Multiple human papilloma virus infections and their impact on the development of high-risk cervical lesions. Acta Cytol. 2015; 59:391–8.
Article17. Bonde JH, Pedersen H, Quint W, Xu L, Arbyn M, Ejegod DM. Clinical and analytical performance of the BD onclarity HPV assay with SurePath screening samples from the Danish Cervical Screening Program using the VALGENT framework. J Clin Microbiol. 2020; 58:e01518–19.
Article18. Kim MS, Lee EH, Park MI, et al. Utility of human papillomavirus testing for cervical cancer screening in Korea. Int J Environ Res Public Health. 2020; 17:1726.
Article19. Darragh TM, Colgan TJ, Cox JT, et al. The lower anogenital squamous terminology standardization project for HPV-associated lesions: background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Arch Pathol Lab Med. 2012; 136:1266–97.20. Ejegod D, Bottari F, Pedersen H, Sandri MT, Bonde J. The BD onclarity HPV assay on samples collected in SurePath medium meets the international guidelines for human papillomavirus test requirements for cervical screening. J Clin Microbiol. 2016; 54:2267–72.21. Kim M, Park NJ, Jeong JY, Park JY. Multiple human papilloma virus (HPV) infections are associated with HSIL and persistent HPV infection status in Korean patients. Viruses. 2021; 13:1342.
Article22. Bonde J, Ejegod DM, Cuschieri K, et al. The Valgent4 protocol: Robust analytical and clinical validation of 11 HPV assays with genotyping on cervical samples collected in SurePath medium. J Clin Virol. 2018; 108:64–71.
Article23. Li M, Du X, Lu M, et al. Prevalence characteristics of single and multiple HPV infections in women with cervical cancer and precancerous lesions in Beijing, China. J Med Virol. 2019; 91:473–81.
Article24. Schmitt M, Depuydt C, Benoy I, et al. Multiple human papillomavirus infections with high viral loads are associated with cervical lesions but do not differentiate grades of cervical abnormalities. J Clin Microbiol. 2013; 51:1458–64.
Article25. Trottier H, Mahmud S, Costa MC, et al. Human papillomavirus infections with multiple types and risk of cervical neoplasia. Cancer Epidemiol Biomarkers Prev. 2006; 15:1274–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Methods for Detection of Human Papillomavirus in Head and Neck Cancer
- Comparative Effects of Bivalent, Quadrivalent, and Nonavalent Human Papillomavirus Vaccines in The Prevention of Genotype-Specific Infection: A Systematic Review and Network Meta-Analysis
- Role of Human Papillomavirus Vaccination for Prevention of Male Infertility
- Clinical significance of human papillomavirus genotyping
- Distribution of Human Papillomavirus 52 and 58 Genotypes, and Their Expression of p16 and p53 in Cervical Neoplasia