J Pathol Transl Med.
2022 Sep;56(5):260-269. 10.4132/jptm.2022.07.05.
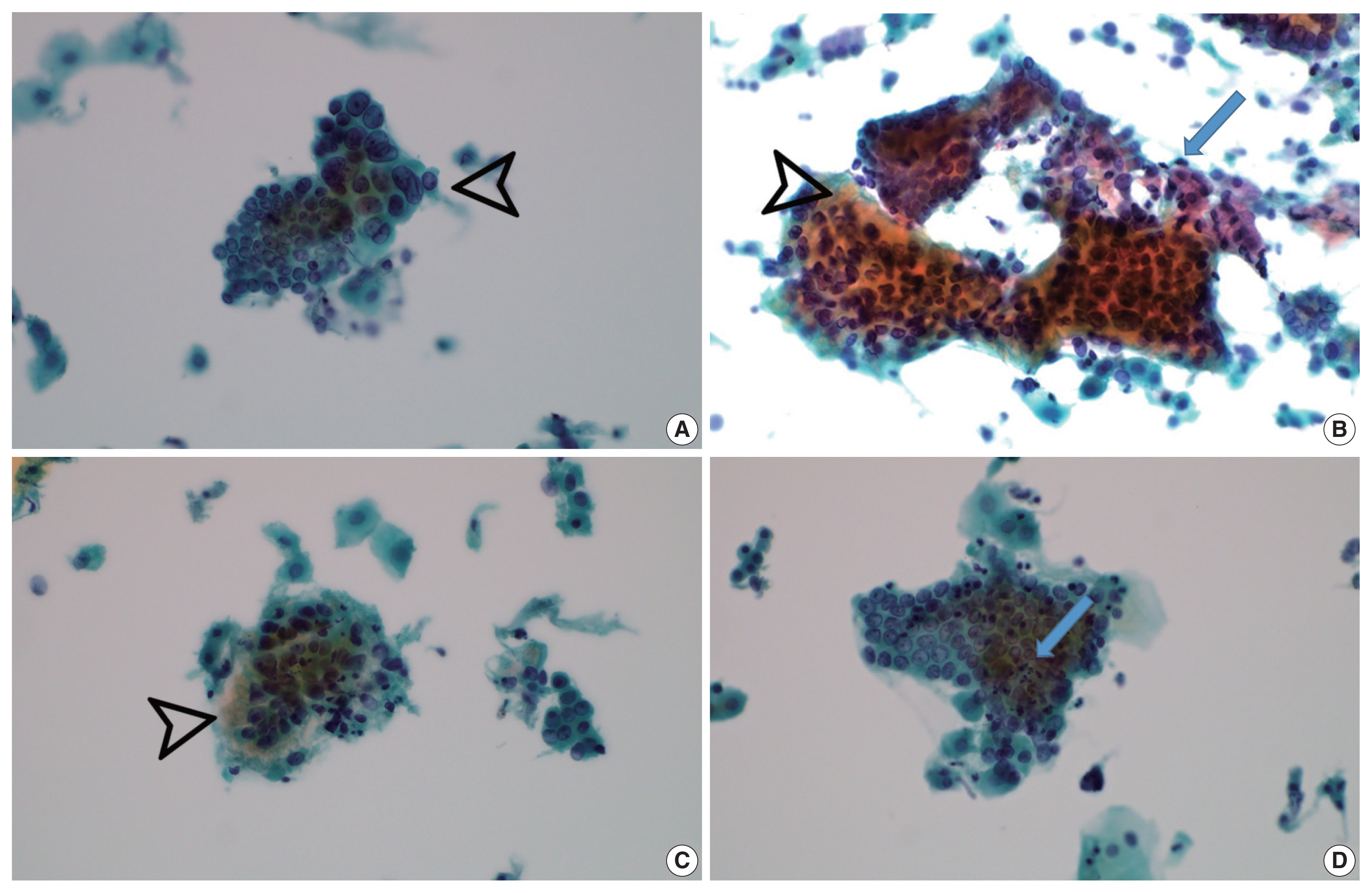
Cytopathologic features of human papillomavirus–independent, gastric-type endocervical adenocarcinoma
- Affiliations
-
- 1Department of Pathology, Chungnam National University School of Medicine, Daejeon, Korea
- KMID: 2533702
- DOI: http://doi.org/10.4132/jptm.2022.07.05
Abstract
- Background
Gastric-type endocervical adenocarcinoma (GEA) is unrelated to human papillomavirus (HPV) infection and is clinically aggressive compared with HPV-associated usual-type endocervical adenocarcinoma (UEA). The cytological diagnosis falls short of a definitive diagnosis of GEA and is often categorized as atypical glandular cells (AGCs). To improve cytologic recognition, cytological findings of HPV-independent GEA were analyzed and the results compared with HPV-associated UEA.
Methods
Cervical Papanicolaou (Pap) smears from eight patients with a histopathologic diagnosis of GEA and 12 control cases of UEA were reviewed. All slides were conventionally prepared and/or liquid-based prepared (ThinPrep) and stained following the Pap method. A mucinous background, architectural, nuclear, and cytoplasmic features were analyzed and compared with UEA.
Results
Preoperative cytologic diagnoses of the eight GEA cases were AGCs, favor neoplastic in three cases, adenocarcinoma in situ in one case, and adenocarcinoma in four cases. Cytologically, monolayered honeycomb-like sheets (p = .002) of atypical endocervical cells with vacuolar granular cytoplasm (p = .001) were extensive in GEA, and three-dimensional clusters (p = .010) were extensive in UEA. Although the differences were not statistically significant, background mucin (p = .058), vesicular nuclei (p = .057), and golden-brown intracytoplasmic mucin (p = .089) were also discriminatory findings for GEA versus UEA.
Conclusions
Although GEA is difficult to diagnose on cytologic screening, GEA can be recognized based on cytologic features of monolayered honeycomb sheets of atypical endocervical cells with abundant vacuolar cytoplasm and some golden-brown intracytoplasmic mucin. UEA cases are characterized by three-dimensional clusters.
Figure
Reference
-
References
1. WHO. Classification of Tumours Editorial Board WHO classification of tumours, 5th ed Female genital tumours. Lyon: International Agency for Research on Cancer;2020.2. Kojima A, Mikami Y, Sudo T, et al. Gastric morphology and immunophenotype predict poor outcome in mucinous adenocarcinoma of the uterine cervix. Am J Surg Pathol. 2007; 31:664–72.
Article3. Kawakami F, Mikami Y, Kojima A, Ito M, Nishimura R, Manabe T. Diagnostic reproducibility in gastric-type mucinous adenocarcinoma of the uterine cervix: validation of novel diagnostic criteria. Histopathology. 2010; 56:551–3.
Article4. Kondo T, Hashi A, Murata SI, et al. Gastric mucin is expressed in a subset of endocervical tunnel clusters: type A tunnel clusters of gastric phenotype. Histopathology. 2007; 50:843–50.
Article5. Hodgson A, Parra-Herran C, Mirkovic J. Immunohistochemical expression of HIK1083 and MUC6 in endometrial carcinomas. Histopathology. 2019; 75:552–8.
Article6. Castanon A, Landy R, Sasieni PD. Is cervical screening preventing adenocarcinoma and adenosquamous carcinoma of the cervix? Int J Cancer. 2016; 139:1040–5.
Article7. Wilbur DC, Chhieng DC, Guidos B, Mody DR. Epithelial abnormalities: glandular. Nayar R, Wilbur DC, editors. The Bethesda system for reporting cervical cytology: definitions, criteria, and explanatory notes. 3rd ed. Heidelberg: Springer;2015. p. 193–240.
Article8. Bhatla N, Berek JS, Cuello Fredes M, et al. Revised FIGO staging for carcinoma of the cervix uteri. Int J Gynaecol Obstet. 2019; 145:129–35.
Article9. Stolnicu S, Barsan I, Hoang L, et al. International Endocervical Adenocarcinoma Criteria and Classification (IECC): a new pathogenetic classification for invasive adenocarcinomas of the endocervix. Am J Surg Pathol. 2018; 42:214–26.10. Talia KL, Oliva E, Rabban JT, Singh N, Stolnicu S, McCluggage WG. Grading of endocervical adenocarcinomas: review of the literature and recommendations from the International Society of Gynecological Pathologists. Int J Gynecol Pathol. 2021; 40(Suppl 1):S66–74.
Article11. Lu S, Shen D, Zhao Y, Kang N, Wang X. Primary endocervical gastric-type adenocarcinoma: a clinicopathologic and immunohistochemical analysis of 23 cases. Diagn Pathol. 2019; 14:72.
Article12. Kawakami F, Mikami Y, Sudo T, Fujiwara K, Hirose T, Itoh T. Cytologic features of gastric-type adenocarcinoma of the uterine cervix. Diagn Cytopathol. 2015; 43:791–6.
Article13. Schwock J, Starova B, Khan ZF, et al. Cytomorphologic features of gastric-type endocervical adenocarcinoma in liquid-based preparations. Acta Cytol. 2021; 65:56–66.
Article14. Hissong E, Yoxtheimer LM, Pacecca A, Hoda RS. Cytology of minimal deviation endocervical adenocarcinoma (adenoma malignum) on a ThinPrep Pap test. Diagn Cytopathol. 2016; 44:552–5.
Article15. Ryu A, Nagata S, Kubo C, et al. Conventional direct smear yields diagnostic indicators of gastric-type mucinous carcinoma compared with cytomorphological features identified by liquid-based cervical cytology. Acta Cytol. 2021; 65:150–7.
Article16. Hata S, Mikami Y, Manabe T. Diagnostic significance of endocervical glandular cells with “golden-yellow” mucin on pap smear. Diagn Cytopathol. 2002; 27:80–4.
Article17. Omori M, Kondo T, Nakazawa K, et al. Interpretation of endocervical cells with gastric-type mucin on Pap smears. Am J Clin Pathol. 2018; 150:259–66.
Article18. Hashi A, Yuminamochi T, Xu JY, Kondo T, Katoh R, Hoshi K. Intranuclear cytoplasmic inclusion is a significant diagnostic feature for the differentiation of lobular endocervical glandular hyperplasia from minimal deviation adenocarcinoma of the cervix. Diagn Cytopathol. 2008; 36:535–44.
Article19. Lee Y, Lee C, Park IA, An HJ, Kim H. Cytomorphological features of hyperchromatic crowded groups in liquid-based cervicovaginal cytology: a single institutional experience. J Pathol Transl Med. 2019; 53:393–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gastric type mucinous endocervical adenocarcinoma of the uterine cervix: very rare and interesting case
- Endocervical Glandular Lesions in Invasive and Intraepithelial Squamous Neoplasms of the Uterine Cervix
- Human Papillomavirus 16/18 Expression of Endocervical Glandular Lesions: Relationship with p53 and MIB-1 Expressions
- Histochemical and Immunohistochemical Properties of Endometrial and Endocervical Adenocarcinoma
- Evaluation of human papillomavirus (HPV) prediction using the International Endocervical Adenocarcinoma Criteria and Classification system, compared to p16 immunohistochemistry and HPV RNA in-situ hybridization