Korean J Gastroenterol.
2022 Sep;80(3):149-153. 10.4166/kjg.2022.047.
Langerhans Cell Histiocytosis with the Synchronous Invasion of Stomach and Colon in an Adult Patient: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University College of Medicine, Korea.
- 2Institute of Health Sciences, Gyeongsang National University, Jinju, Korea.
- KMID: 2533318
- DOI: http://doi.org/10.4166/kjg.2022.047
Abstract
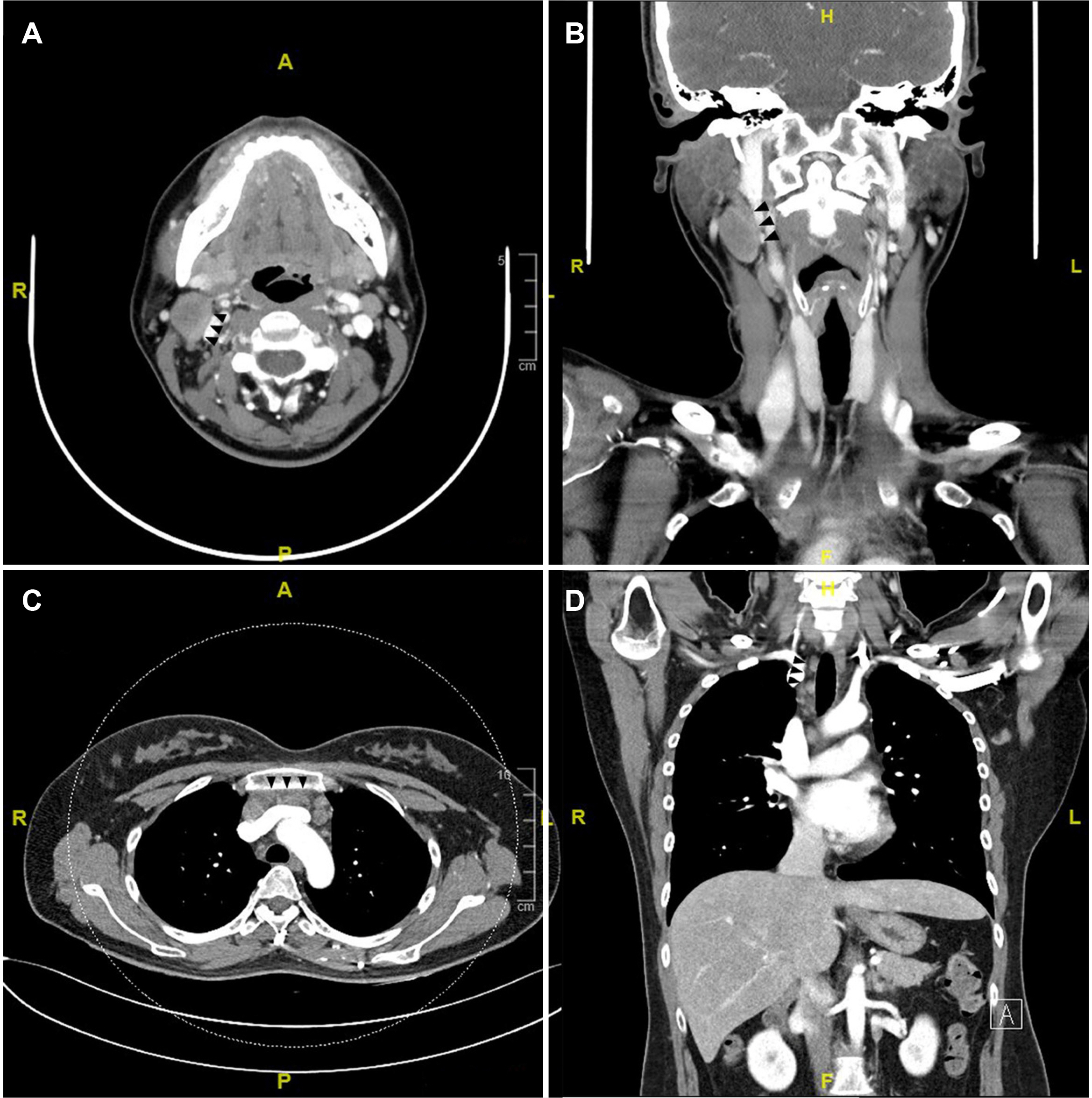
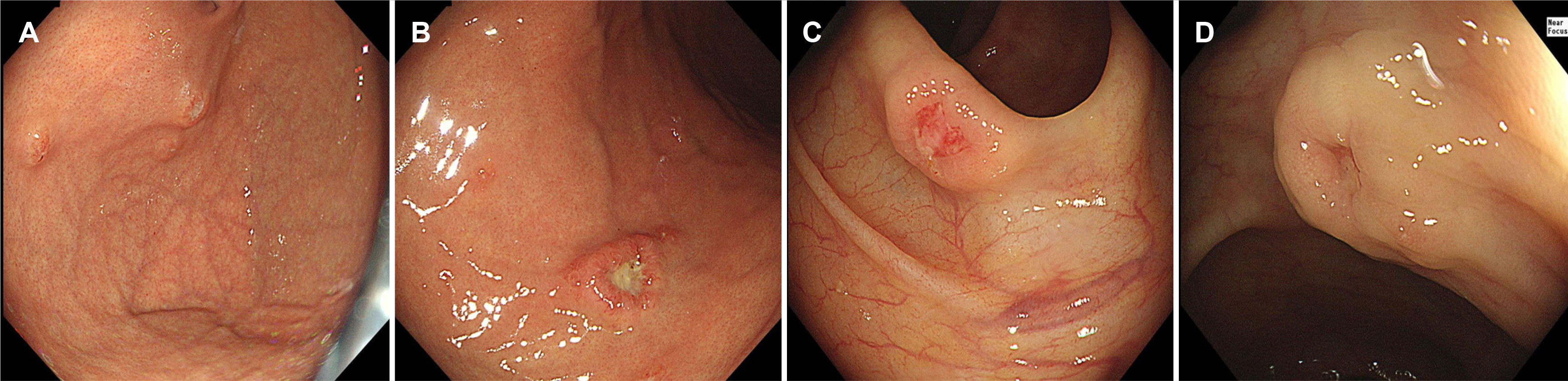
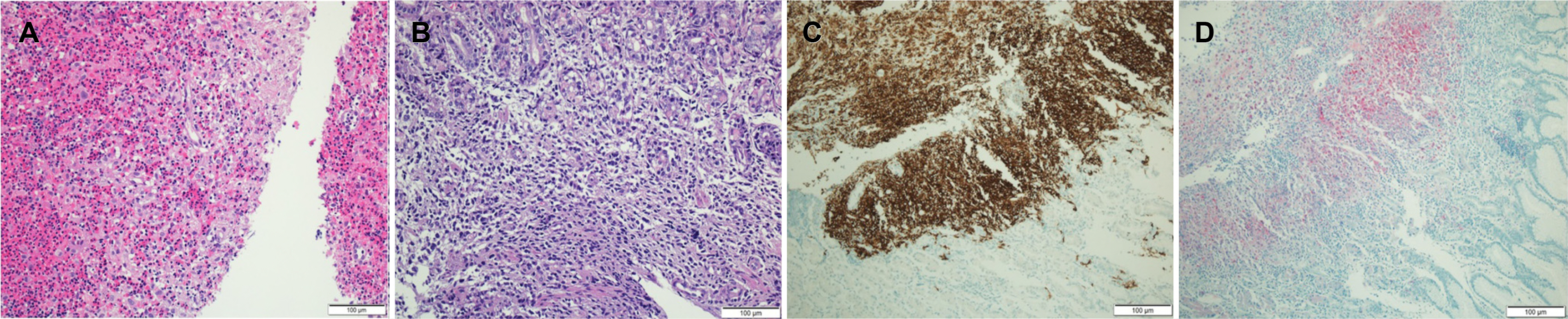
- Langerhans cell histiocytosis (LCH) is reported less frequently in adults than in children. The most common site of involvement in adults is the bone, accounting for 30-50% of cases. The gastrointestinal tract is very rare, accounting for approximately 2%. We present a case of Langerhans cell histiocytosis that simultaneously invaded multiple organs, including the stomach and colon, in an adult. A 37-year-old woman with no underlying disease complained of chest discomfort and a palpable right submandibular mass. A right Level II neck mass and mediastinal LN enlargement were confirmed on the pharynx and chest CT scan. Multiple subepithelial masses with central ulceration and erosion were observed in the corpus and fundus on the esophagogastroduodenoscopy and in the right colon on the colonoscopy. The histopathology findings were the same in each tissue biopsied from the stomach, colon, and right neck lymph nodes. Langerhans cells with classical reniform nuclei and prominent eosinophils invaded the normal glands, and S100 and CD1a were positive in the immunohistochemical stain. Gastrointestinal involvement of LCH in adults is rare, asymptomatic,and can involve multiple digestive organs simultaneously, so upper endoscopy and colonoscopy should be considered for a diagnosis.
Keyword
Figure
Reference
-
1. Rao DG, Trivedi MV, Havale R, Shrutha SP. 2017; A rare and unusual case report of Langerhans cell histiocytosis. J Oral Maxillofac Pathol. 21:140–144. DOI: 10.4103/jomfp.JOMFP_10_17. PMID: 28479703. PMCID: PMC5406796.2. Aricò M, Girschikofsky M, Généreau T, et al. 2003; Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 39:2341–2348. DOI: 10.1016/S0959-8049(03)00672-5.3. Singhi AD, Montgomery EA. 2011; Gastrointestinal tract langerhans cell histiocytosis: a clinicopathologic study of 12 patients. Am J Surg Pathol. 35:305–310. DOI: 10.1097/PAS.0b013e31820654e4. PMID: 21263252.4. Shankar U, Prasad M, Chaurasia OP. 2012; A rare case of langerhans cell histiocytosis of the gastrointestinal tract. World J Gastroenterol. 18:1410–1413. DOI: 10.3748/wjg.v18.i12.1410. PMID: 22493557. PMCID: PMC3319970.5. Gulati N, Allen CE. 2021; Langerhans cell histiocytosis: version 2021. Hematol Oncol. 39 Suppl 1(Suppl 1):15–23. DOI: 10.1002/hon.2857. PMID: 34105821. PMCID: PMC9150752.6. Jezierska M, Stefanowicz J, Romanowicz G, Kosiak W, Lange M. 2018; Langerhans cell histiocytosis in children - a disease with many faces. Recent advances in pathogenesis, diagnostic examinations and treatment. Postepy Dermatol Alergol. 35:6–17. DOI: 10.5114/pdia.2017.67095. PMID: 29599667. PMCID: PMC5872238.7. Lee SJ, Hwang CS, Huh GY, Lee CH, Park DY. 2015; Gastric Langerhans cell histiocytosis: case report and review of the literature. J Pathol Transl Med. 49:421–423. DOI: 10.4132/jptm.2015.05.19. PMID: 26056155. PMCID: PMC4579285.8. Haupt R, Minkov M, Astigarraga I, et al. 2013; Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 60:175–184. DOI: 10.1002/pbc.24367. PMID: 23109216. PMCID: PMC4557042.9. Allen CE, Ladisch S, McClain KL. 2015; How I treat Langerhans cell histiocytosis. Blood. 126:26–35. DOI: 10.1182/blood-2014-12-569301. PMID: 25827831. PMCID: PMC4492195.10. Grana N. 2014; Langerhans cell histiocytosis. Cancer Control. 21:328–334. DOI: 10.1177/107327481402100409. PMID: 25310214.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Pneumothorax due to Pulmonary Invasion in Multisystemic Langerhans Cell Histiocytosis: A case report
- A Case of Gastric Langerhans Cell Histiocytosis Showing Hypertrophic Folds
- A Case of Xanthoma Dissemiantum with Laryngeal and Stomach Mucosal Involvement
- A Case of Pulmonary Langerhans Cell Histiocytosis with Pneumothorax
- A Case of Gastric Langerhans Cell Histiocytosis with Spontaneous Regression