Ann Surg Treat Res.
2022 Sep;103(3):145-152. 10.4174/astr.2022.103.3.145.
Safety of performing distal pancreatosplenectomy in patients who underwent distal gastrectomy previously: a multicenter cohort analysis with systematic literature review
- Affiliations
-
- 1Department of Hepatobiliary and Pancreas Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Surgery, Yeoiudo St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Surgery, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Surgery, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Surgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 6Department of Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 7Department of Surgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2532926
- DOI: http://doi.org/10.4174/astr.2022.103.3.145
Abstract
- Purpose
In patients who have previously undergone subtotal gastrectomy (STG), the remnant stomach is supplied with arterial blood through the splenic artery. It is currently unclear whether the remnant stomach can be safely preserved when performing distal pancreatosplenectomy (DPS) in these patients. Thus, this study aimed to evaluate the safety and feasibility of performing DPS in patients who had undergone a previous STG.
Methods
A multicenter cohort study was performed to identify patients who underwent DPS. Electronic medical data of Clinical Data Warehouse from 7 representative high-volume centers in 5 cities were retrospectively reviewed. A propensity score-matched analysis was performed to match patients who had no history of upper abdominal surgery with patients who had undergone a previous STG.
Results
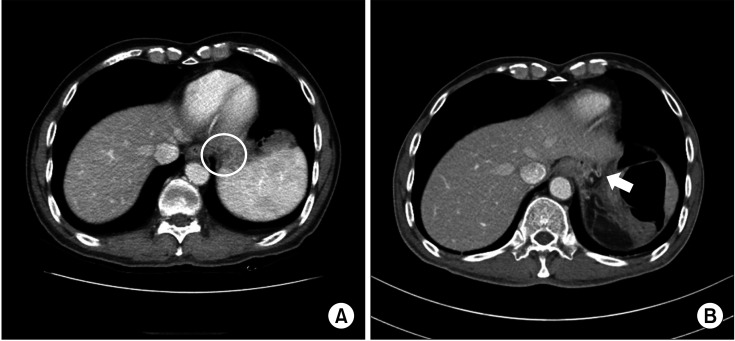
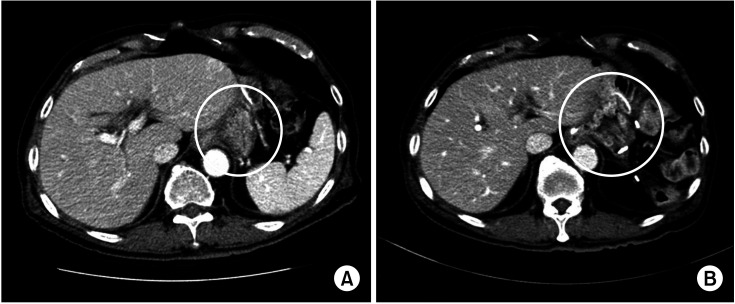
Fourteen DPS patients who had a history of STG (STG group) were studied and matched to 70 patients who underwent DPS without any history of upper abdominal surgery (non-STG group). All patients in the STG group had the remnant stomach preserved. In most patients, the blood vessel supplying blood to the remnant stomach was the left inferior phrenic artery. There was no significant difference in the incidence of stomach-related complications or length of hospital stay between the 2 groups.
Conclusion
Our study results suggest that the remnant stomach could be safely preserved when performing DPS in patients with a prior STG. However, it is necessary to carefully evaluate the vascular structure of the remnant stomach through preoperative imaging study and closely observe changes to the blue stomach during the operation.
Figure
Reference
-
1. Kim TH, Lee YJ, Bae K, Park JH, Hong SC, Jung EJ, et al. The investigation of diet recovery after distal gastrectomy. Medicine (Baltimore). 2019; 98:e17543. PMID: 31593134.
Article2. Milito P, Aiolfi A, Asti E, Rausa E, Bonitta G, Bonavina L. Impact of spleen preserving laparoscopic distal pancreatectomy on postoperative infectious complications: systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A. 2019; 29:167–177. PMID: 30592691.
Article3. Takahashi H, Nara S, Ohigashi H, Sakamoto Y, Gotoh K, Esaki M, et al. Is preservation of the remnant stomach safe during distal pancreatectomy in patients who have undergone distal gastrectomy? World J Surg. 2013; 37:430–436. PMID: 23188537.
Article4. Kimura J, Okabayashi T, Sui K, Matsumoto T, Murokawa T, Iwata J, et al. Feasibility of preserving the remnant stomach during distal pancreatectomy after distal gastrectomy. Surg Today. 2020; 50:1394–1401. PMID: 32358628.
Article5. Kelly KJ, Greenblatt DY, Wan Y, Rettammel RJ, Winslow E, Cho CS, et al. Risk stratification for distal pancreatectomy utilizing ACS-NSQIP: preoperative factors predict morbidity and mortality. J Gastrointest Surg. 2011; 15:250–259. PMID: 21161427.
Article6. Gockel I, Pietzka S, Gönner U, Hommel G, Junginger T. Subtotal or total gastrectomy for gastric cancer: impact of the surgical procedure on morbidity and prognosis--analysis of a 10-year experience. Langenbecks Arch Surg. 2005; 390:148–155. PMID: 15711817.
Article7. Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020; 52:335–350. PMID: 32178489.
Article8. Tascilar M, van Rees BP, Sturm PD, Tytgat GN, Hruban RH, Goodman SN, et al. Pancreatic cancer after remote peptic ulcer surgery. J Clin Pathol. 2002; 55:340–345. PMID: 11986336.
Article9. Offerhaus GJ, Giardiello FM, Moore GW, Tersmette AC. Partial gastrectomy: a risk factor for carcinoma of the pancreas? Hum Pathol. 1987; 18:285–288. PMID: 3028929.
Article10. Maringhini A, Thiruvengadam R, Melton LJ, Hench VS, Zinsmeister AR, DiMagno EP. Pancreatic cancer risk following gastric surgery. Cancer. 1987; 60:245–247. PMID: 3594361.
Article11. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.12. Isabella V, Marotta E, Bianchi F. Ischemic necrosis of proximal gastric remnant following subtotal gastrectomy with splenectomy. J Surg Oncol. 1984; 25:124–132. PMID: 6420621.
Article13. Alshehri A, Kim HS, Kim BS. Laparoscopic management of gastric remnant ischemia after laparoscopic distal gastrectomy with Billroth-I anastomosis: a case report. Int J Surg Case Rep. 2020; 66:265–269. PMID: 31884262.
Article14. Yovanovitch BY. Contribution to the study of ischemic necrosis of the stump after subtotal gastrectomy. Ann Chir. 1960; 14:261–264. PMID: 13846674.15. Cate WR Jr, Dawson RE. The viability of proximal gastric remnants following radical subtotal gastrectomy and gastroduodenostomy; an experimental study. Surgery. 1957; 41:401–405. PMID: 13409217.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Port-site metastasis after laparoscopic radical pancreatosplenectomy in left-sided pancreatic cancer
- Laparoscopic distal pancreatosplenectomy for left-sided pancreatic cancer in patients with radical subtotal gastrectomy for gastric cancer
- Laparoscopic Distal Gastrectomy for Gastric Cancer
- Comparison of laparoscopy-assisted and totally laparoscopic Billroth-II distal gastrectomy for gastric cancer
- Comparison of Laparoscopy-Assisted and Totally Laparoscopic Distal Gastrectomy: The Short-Term Outcome at a Low Volume Center