J Korean Med Sci.
2022 Aug;37(34):e262. 10.3346/jkms.2022.37.e262.
Comprehensive Rehabilitation in Severely Ill Inpatients With COVID-19: A Cohort Study in a Tertiary Hospital
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2532756
- DOI: http://doi.org/10.3346/jkms.2022.37.e262
Abstract
- Background
This study aimed to investigate the effects of comprehensive rehabilitation management on functional recovery and examine the correlation between clinical parameters and improvements in functional outcomes in severe-to-critical inpatients with coronavirus disease 2019 (COVID-19) in a tertiary hospital.
Methods
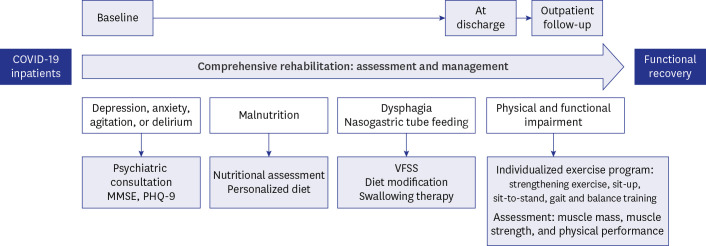
Post-acute COVID-19 patients who had a World Health Organization (WHO) ordinal scale of 5–7, underwent intensive care, and received comprehensive rehabilitation management, including exercise programs, nutritional support, dysphagia evaluation, and psychological care were included. The appendicular skeletal muscle mass index (SMI), Medical Research Council sum score, handgrip strength, number of repetitions in the 1-minute sit-to-stand test, gait speed, Berg Balance Scale (BBS), and Functional Ambulation Classification (FAC) were evaluated at hospital stay, discharge, and 1-month follow-up. The correlation between the rehabilitation dose and improvement in each outcome measure was analyzed.
Results
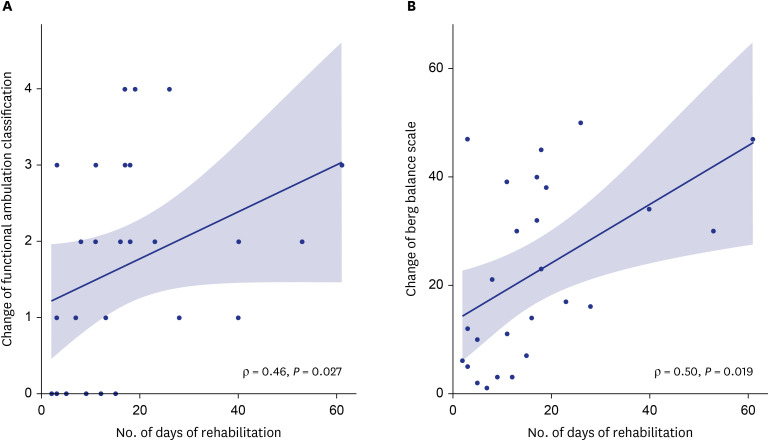
Overall, 37 patients were enrolled, of whom 59.5% and 32.4% had a score of 6 and 7 on the WHO ordinal scale, respectively. Lengths of stay in the intensive care unit and hospital were 33.6 ± 23.9 and 63.8 ± 36.5 days. Outcome measures revealed significant improvements at discharge and 1-month follow-up. The SMI was significantly increased at the 1-month follow-up (6.13 [5.24–7.76]) compared with that during the hospital stay (5.80 [5.39–7.05]). We identified dose-response associations between the rehabilitation dose and FAC (ρ = 0.46) and BBS (ρ = 0.50) scores. Patients with older age, longer hospitalization, longer stay at the intensive care unit, longer duration of mechanical ventilation, tracheostomy, a more depressive mood, and poorer nutritional status revealed poorer improvement in gait speed at the 1-month follow-up.
Conclusion
Comprehensive rehabilitation management effectively improved muscle mass, muscle strength, and physical performance in severe-to-critical COVID-19 patients. Dose-response relationship of rehabilitation and functional improvement emphasizes the importance of intensive post-acute inpatient rehabilitation in COVID-19 survivors.
Keyword
Figure
Reference
-
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382(8):727–733. PMID: 31978945.
Article2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323(13):1239–1242. PMID: 32091533.
Article3. Pascarella G, Strumia A, Piliego C, Bruno F, Del Buono R, Costa F, et al. COVID-19 diagnosis and management: a comprehensive review. J Intern Med. 2020; 288(2):192–206. PMID: 32348588.
Article4. Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020; 201(11):1380–1388. PMID: 32275452.
Article5. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708–1720. PMID: 32109013.
Article6. Sung HK, Kim JY, Heo J, Seo H, Jang YS, Kim H, et al. Clinical course and outcomes of 3,060 patients with coronavirus disease 2019 in Korea, January–May 2020. J Korean Med Sci. 2020; 35(30):e280. PMID: 32743995.
Article7. Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011; 364(14):1293–1304. PMID: 21470008.
Article8. Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A, et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis. J Rehabil Med. 2020; 52(5):jrm00063. PMID: 32449782.
Article9. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020; 77(6):683–690. PMID: 32275288.
Article10. Estraneo A, Ciapetti M, Gaudiosi C, Grippo A. Not only pulmonary rehabilitation for critically ill patients with COVID-19. J Neurol. 2021; 268(1):27–29. PMID: 32676766.
Article11. Zampogna E, Migliori GB, Centis R, Cherubino F, Facchetti C, Feci D, et al. Functional impairment during post-acute COVID-19 phase: preliminary finding in 56 patients. Pulmonology. 2021; 27(5):452–455. PMID: 33454281.
Article12. Liang L, Yang B, Jiang N, Fu W, He X, Zhou Y, et al. Three-month follow-up study of survivors of coronavirus disease 2019 after discharge. J Korean Med Sci. 2020; 35(47):e418. PMID: 33289374.
Article13. Latronico N, Peli E, Calza S, Rodella F, Novelli MP, Cella A, et al. Physical, cognitive and mental health outcomes in 1-year survivors of COVID-19-associated ARDS. Thorax. 2022; 77(3):300–303. PMID: 34588274.
Article14. Stam HJ, Stucki G, Bickenbach J. European Academy of Rehabilitation Medicine. Covid-19 and post intensive care syndrome: a call for action. J Rehabil Med. 2020; 52(4):jrm00044. PMID: 32286675.
Article15. Whiteson JH, Escalón MX, Maltser S, Verduzco-Gutierrez M. Demonstrating the vital role of physiatry throughout the health care continuum: Lessons learned from the impacts of the COVID-19 pandemic on inpatient rehabilitation. PM R. 2021; 13(6):554–562. PMID: 34097361.
Article16. Stutz MR, Leonhard AG, Ward CM, Pearson SD, Osorio PL, Herbst PR, et al. Early rehabilitation feasibility in a COVID-19 ICU. Chest. 2021; 160(6):2146–2148. PMID: 34116067.
Article17. Park YH, Ko RE, Kang D, Park J, Jeon K, Yang JH, et al. Relationship between use of rehabilitation resources and ICU readmission and ER visits in ICU survivors: the Korean ICU National Data Study 2008-2015. J Korean Med Sci. 2020; 35(15):e101. PMID: 32301293.
Article18. Kirby T. COVID-19 survivor experiencing long-term symptoms. Lancet Respir Med. 2021; 9(6):570–572. PMID: 33587889.
Article19. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021; 397(10270):220–232. PMID: 33428867.
Article20. Albu S, Rivas Zozaya N, Murillo N, García-Molina A, Figueroa Chacón CA, Kumru H. Multidisciplinary outpatient rehabilitation of physical and neurological sequelae and persistent symptoms of covid-19: a prospective, observational cohort study. Disabil Rehabil. 2021; 24:1–8.
Article21. Rodrigues M, Costa AJ, Santos R, Diogo P, Gonçalves E, Barroso D, et al. Inpatient rehabilitation can improve functional outcomes of post-intensive care unit COVID-19 patients-a prospective study. Disabil Rehabil. Forthcoming. 2022; DOI: 10.1080/09638288.2022.2032408.
Article22. Piquet V, Luczak C, Seiler F, Monaury J, Martini A, Ward AB, et al. Do patients with Covid-19 benefit from rehabilitation? Functional outcomes of the first 100 patients in a Covid-19 rehabilitation unit. Arch Phys Med Rehabil. 2021; 102(6):1067–1074. PMID: 33548208.
Article23. World Health Organization. COVID-19 therapeutic trial synopsis. Updated 2020. Accessed April 19, 2022. https://www.who.int/publications/i/item/covid-19-therapeutic-trial-synopsis .24. An JA, Song KH, Kim ES, Kwak R, Jung J, Park JY, et al. Pandemic preparedness of an academic medical centre in the Republic of Korea. Clin Microbiol Infect. 2020; 26(12):1595–1599. PMID: 32891767.
Article25. O’Neill B, McDowell K, Bradley J, Blackwood B, Mullan B, Lavery G, et al. Effectiveness of a programme of exercise on physical function in survivors of critical illness following discharge from the ICU: study protocol for a randomised controlled trial (REVIVE). Trials. 2014; 15(1):146. PMID: 24767671.
Article26. White JV, Guenter P, Jensen G, Malone A, Schofield M, et al. Academy Malnutrition Work Group. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr. 2012; 36(3):275–283. PMID: 22535923.
Article27. Arabi YM, Al-Dorzi HM, Sadat M. Protein intake and outcome in critically ill patients. Curr Opin Clin Nutr Metab Care. 2020; 23(1):51–58. PMID: 31743123.
Article28. Boaden E, Nightingale J, Bradbury C, Hives L, Georgiou R. Clinical practice guidelines for videofluoroscopic swallowing studies: a systematic review. Radiography (Lond). 2020; 26(2):154–162. PMID: 32052773.
Article29. Macht M, White SD, Moss M. Swallowing dysfunction after critical illness. Chest. 2014; 146(6):1681–1689. PMID: 25451355.
Article30. Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002; 32(9):509–515.
Article31. Ali NA, O’Brien JM Jr, Hoffmann SP, Phillips G, Garland A, Finley JC, et al. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 2008; 178(3):261–268. PMID: 18511703.
Article32. Turan Z, Topaloglu M, Ozyemisci Taskiran O. Medical Research Council-sumscore: a tool for evaluating muscle weakness in patients with post-intensive care syndrome. Crit Care. 2020; 24(1):562. PMID: 32948221.
Article33. Peolsson A, Hedlund R, Öberg B. Intra- and inter-tester reliability and reference values for hand strength. J Rehabil Med. 2001; 33(1):36–41. PMID: 11480468.
Article34. Hermans G, Clerckx B, Vanhullebusch T, Segers J, Vanpee G, Robbeets C, et al. Interobserver agreement of Medical Research Council sum-score and handgrip strength in the intensive care unit. Muscle Nerve. 2012; 45(1):18–25. PMID: 22190301.
Article35. Bohannon RW, Crouch R. 1-minute sit-to-stand test: systematic review of procedures, performance, and clinimetric properties. J Cardiopulm Rehabil Prev. 2019; 39(1):2–8. PMID: 30489442.36. Reychler G, Boucard E, Peran L, Pichon R, Le Ber-Moy C, Ouksel H, et al. One minute sit-to-stand test is an alternative to 6MWT to measure functional exercise performance in COPD patients. Clin Respir J. 2018; 12(3):1247–1256. PMID: 28621019.
Article37. Jung HY, Park JH, Shim JJ, Kim MJ, Hwang MR, Kim SH. Reliability test of Korean version of berg balance scale. J Korean Acad Rehabil Med. 2006; 30(6):611–618.38. Mehrholz J, Wagner K, Rutte K, Meissner D, Pohl M. Predictive validity and responsiveness of the functional ambulation category in hemiparetic patients after stroke. Arch Phys Med Rehabil. 2007; 88(10):1314–1319. PMID: 17908575.
Article39. Peters DM, Fritz SL, Krotish DE. Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. 2013; 36(1):24–30. PMID: 22415358.
Article40. Busk H, Holm P, Skou ST, Seitner S, Siemsen T, Wienecke T. Inter-rater reliability and agreement of 6 minute Walk Test and 10 meter Walk Test at comfortable walk speed in patients with acute stroke. Physiother Theory Pract. Forthcoming. 2022; DOI: 10.1080/09593985.2022.2030830.
Article41. Zou X, Li S, Fang M, Hu M, Bian Y, Ling J, et al. Acute physiology and chronic health evaluation II score as a predictor of hospital mortality in patients of coronavirus disease 2019. Crit Care Med. 2020; 48(8):e657–e665. PMID: 32697506.
Article42. Parry SM, Puthucheary ZA. The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extrem Physiol Med. 2015; 4(1):16. PMID: 26457181.
Article43. Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011; 39(2):371–379. PMID: 20959786.
Article44. Daher A, Balfanz P, Cornelissen C, Müller A, Bergs I, Marx N, et al. Follow up of patients with severe coronavirus disease 2019 (COVID-19): pulmonary and extrapulmonary disease sequelae. Respir Med. 2020; 174:106197. PMID: 33120193.
Article45. Lau HM, Ng GY, Jones AY, Lee EW, Siu EH, Hui DS. A randomised controlled trial of the effectiveness of an exercise training program in patients recovering from severe acute respiratory syndrome. Aust J Physiother. 2005; 51(4):213–219. PMID: 16321128.
Article46. Puchner B, Sahanic S, Kirchmair R, Pizzini A, Sonnweber B, Wöll E, et al. Beneficial effects of multi-disciplinary rehabilitation in postacute COVID-19: an observational cohort study. Eur J Phys Rehabil Med. 2021; 57(2):189–198. PMID: 33448756.
Article47. Curci C, Negrini F, Ferrillo M, Bergonzi R, Bonacci E, Camozzi DM, et al. Functional outcome after inpatient rehabilitation in postintensive care unit COVID-19 patients: findings and clinical implications from a real-practice retrospective study. Eur J Phys Rehabil Med. 2021; 57(3):443–450. PMID: 33393278.
Article48. Carfì A, Bernabei R, Landi F. Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA. 2020; 324(6):603–605. PMID: 32644129.
Article49. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021; 27(4):601–615. PMID: 33753937.
Article50. Bertolucci F, Sagliocco L, Tolaini M, Posteraro F. Comprehensive rehabilitation treatment for sub-acute COVID-19 patients: an observational study. Eur J Phys Rehabil Med. 2021; 57(2):208–215. PMID: 33541042.
Article51. Olezene CS, Hansen E, Steere HK, Giacino JT, Polich GR, Borg-Stein J, et al. Functional outcomes in the inpatient rehabilitation setting following severe COVID-19 infection. PLoS One. 2021; 16(3):e0248824. PMID: 33788876.
Article52. Welch C, Greig C, Masud T, Wilson D, Jackson TA. COVID-19 and acute sarcopenia. Aging Dis. 2020; 11(6):1345–1351. PMID: 33269092.
Article53. Morley JE, Kalantar-Zadeh K, Anker SD. COVID-19: a major cause of cachexia and sarcopenia? J Cachexia Sarcopenia Muscle. 2020; 11(4):863–865. PMID: 32519505.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fasting Plasma Glucose Level Independently Predicts the Mortality of Patients with Coronavirus Disease 2019 Infection: A Multicenter, Retrospective Cohort Study
- How We Have Treated Severe to Critically Ill Patients With Coronavirus Disease 2019 in Korea
- Factors Influencing Person-Centered Care among Nurses in COVID-19 Special Care Units at Tertiary General Hospitals: A Cross-Sectional Descriptive Study
- Perceptions of Coronavirus Disease 2019 (COVID-19) in Patients With Schizophrenia
- Cardiovascular Manifestations of COVID-19