J Korean Med Sci.
2022 Aug;37(34):e258. 10.3346/jkms.2022.37.e258.
Respiratory Syncytial Virus Outbreak Without Influenza in the Second Year of the Coronavirus Disease 2019 Pandemic: A National Sentinel Surveillance in Korea, 2021–2022 Season
- Affiliations
-
- 1Department of Social and Preventive Medicine, Sungkyunkwan University School of Medicine, Suwon, Korea
- 2Biostatistics Collaboration Unit, Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea
- 4Institute for Immunology and Immunological Diseases, Yonsei University College of Medicine, Seoul, Korea
- 5Division of Infectious Diseases, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 6Artificial Intelligence and Big-Data Convergence Center, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 7Department of Preventive Medicine, Gachon University College of Medicine, Incheon, Korea
- KMID: 2532754
- DOI: http://doi.org/10.3346/jkms.2022.37.e258
Abstract
- Background
This study aimed to investigate whether respiratory syncytial virus (RSV) and influenza virus (IFV) infections would occur in 2021–2022 as domestic nonpharmaceutical interventions (NPIs) are easing.
Methods
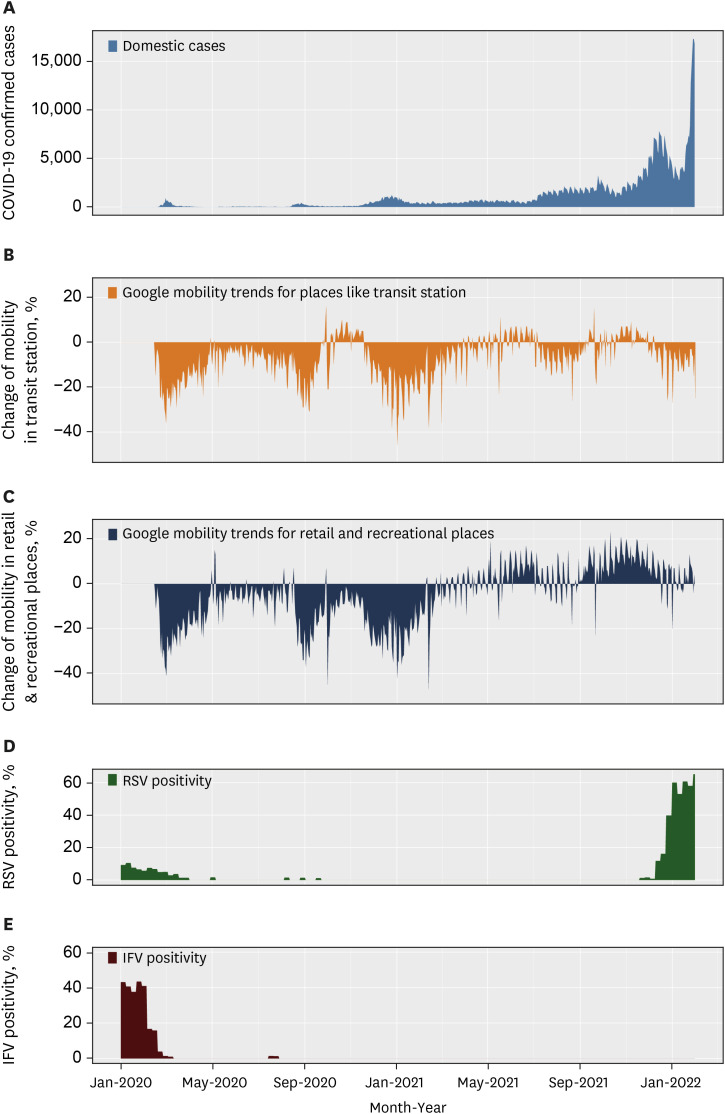
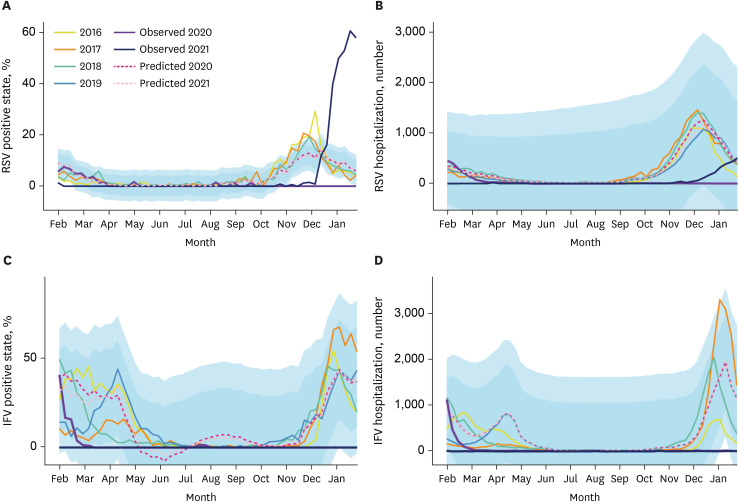
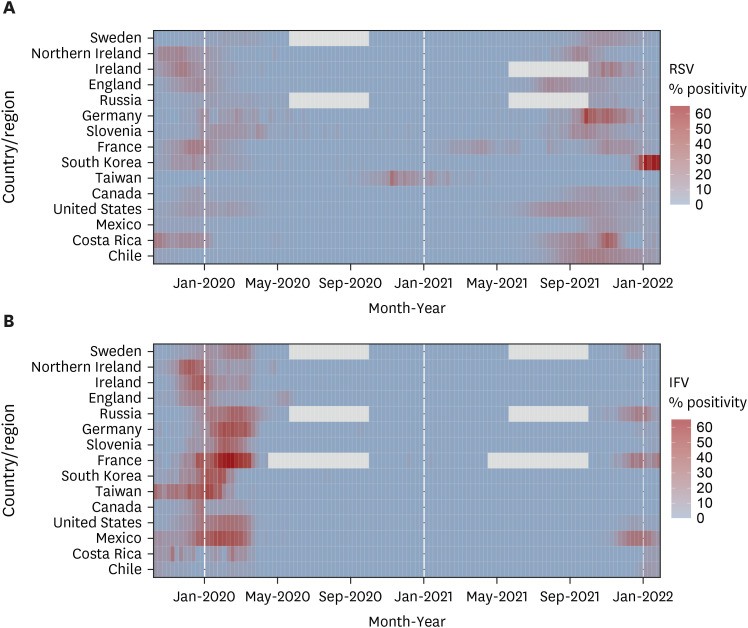
Data were collected from the Korean Influenza and Respiratory Virus Monitoring System database. The weekly positivity rates of respiratory viruses and number of hospitalizations for acute respiratory infections were evaluated (January 2016–2022). The period from February 2020 to January 2022 was considered the NPI period. The autoregressive integrated moving average model and Poisson analysis were used for data analysis. Data from 14 countries/regions that reported positivity rates of RSV and IFV were also investigated.
Results
Compared with the pre-NPI period, the positivity and hospitalization rates for IFV infection during 2021–2022 significantly decreased to 0.0% and 1.0%, respectively, at 0.0% and 1.2% of the predicted values, respectively. The RSV infection positivity rate in 2021–2022 was 1.8-fold higher than that in the pre-NPI period at 1.5-fold the predicted value. The hospitalization rate for RSV was 20.0% of that in the pre-NPI period at 17.6% of the predicted value. The re-emergence of RSV and IFV infections during 2020–2021 was observed in 13 and 4 countries, respectively.
Conclusion
During 2021–2022, endemic transmission of the RSV, but not IFV, was observed in Korea.
Keyword
Figure
Reference
-
1. Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009; 360(6):588–598. PMID: 19196675.
Article2. Shi T, McAllister DA, O’Brien KL, Simoes EA, Madhi SA, Gessner BD, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet. 2017; 390(10098):946–958. PMID: 28689664.3. Leung NH. Transmissibility and transmission of respiratory viruses. Nat Rev Microbiol. 2021; 19(8):528–545. PMID: 33753932.
Article4. Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005; 352(17):1749–1759. PMID: 15858184.
Article5. van Summeren J, Meijer A, Aspelund G, Casalegno JS, Erna G, Hoang U, et al. Low levels of respiratory syncytial virus activity in Europe during the 2020/21 season: what can we expect in the coming summer and autumn/winter? Euro Surveill. 2021; 26(29):2100639.
Article6. Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, et al. Decreased influenza activity during the COVID-19 pandemic - United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(37):1305–1309. PMID: 32941415.
Article7. Huh K, Jung J, Hong J, Kim M, Ahn JG, Kim JH, et al. Impact of nonpharmaceutical interventions on the incidence of respiratory infections during the coronavirus disease 2019 (COVID-19) outbreak in Korea: a nationwide surveillance study. Clin Infect Dis. 2021; 72(7):e184–e191. PMID: 33150393.
Article8. Kim JH, Roh YH, Ahn JG, Kim MY, Huh K, Jung J, et al. Respiratory syncytial virus and influenza epidemics disappearance in Korea during the 2020–2021 season of COVID-19. Int J Infect Dis. 2021; 110:29–35. PMID: 34245886.
Article9. Nolen LD, Seeman S, Bruden D, Klejka J, Desnoyers C, Tiesinga J, et al. Impact of social distancing and travel restrictions on non-coronavirus disease 2019 (non-COVID-19) respiratory hospital admissions in young children in rural Alaska. Clin Infect Dis. 2021; 72(12):2196–2198. PMID: 32888007.
Article10. Rodgers L, Sheppard M, Smith A, Dietz S, Jayanthi P, Yuan Y, et al. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin Infect Dis. 2021; 73(Suppl 1):S110–S117. PMID: 33912902.
Article11. Fourgeaud J, Toubiana J, Chappuy H, Delacourt C, Moulin F, Parize P, et al. Impact of public health measures on the post-COVID-19 respiratory syncytial virus epidemics in France. Eur J Clin Microbiol Infect Dis. 2021; 40(11):2389–2395. PMID: 34347190.
Article12. Yeoh DK, Foley DA, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. Impact of coronavirus disease 2019 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021; 72(12):2199–2202. PMID: 32986804.
Article13. Gomez GB, Mahé C, Chaves SS. Uncertain effects of the pandemic on respiratory viruses. Science. 2021; 372(6546):1043–1044. PMID: 34083477.
Article14. KDCA. Quarantine management flow chart for overseas entrants (entrants via an airport). Updated 2022. Accessed August 11, 2022. https://overseas.mofa.go.kr/dk-en/brd/m_7038/view.do?seq=761185&page=1 .15. Belongia EA, Simpson MD, King JP, Sundaram ME, Kelley NS, Osterholm MT, et al. Variable influenza vaccine effectiveness by subtype: a systematic review and meta-analysis of test-negative design studies. Lancet Infect Dis. 2016; 16(8):942–951. PMID: 27061888.
Article16. Nguyen C, Kaku S, Tutera D, Kuschner WG, Barr J. Viral respiratory infections of adults in the intensive care unit. J Intensive Care Med. 2016; 31(7):427–441. PMID: 25990273.
Article17. Lessler J, Reich NG, Brookmeyer R, Perl TM, Nelson KE, Cummings DA. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis. 2009; 9(5):291–300. PMID: 19393959.
Article18. Edwards KM. The impact of social distancing for severe acute respiratory syndrome coronavirus 2 on respiratory syncytial virus and influenza burden. Clin Infect Dis. 2021; 72(12):2076–2078. PMID: 33038221.
Article19. Eden JS, Sikazwe C, Xie R, Deng YM, Sullivan SG, Michie A, et al. Off-season RSV epidemics in Australia after easing of COVID-19 restrictions. Nat Commun. 2022; 13(1):2884. PMID: 35610217.
Article20. Baker RE, Park SW, Yang W, Vecchi GA, Metcalf CJ, Grenfell BT. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc Natl Acad Sci U S A. 2020; 117(48):30547–30553. PMID: 33168723.
Article21. Zheng Z, Pitzer VE, Shapiro ED, Bont LJ, Weinberger DM. Estimation of the timing and intensity of reemergence of respiratory syncytial virus following the COVID-19 pandemic in the US. JAMA Netw Open. 2021; 4(12):e2141779. PMID: 34913973.
Article22. Sombetzki M, Lücker P, Ehmke M, Bock S, Littmann M, Reisinger EC, et al. Impact of changes in infection control measures on the dynamics of COVID-19 infections in schools and pre-schools. Front Public Health. 2021; 9:780039. PMID: 34988054.
Article23. Hayden FG, Whitley RJ. Respiratory syncytial virus antivirals: problems and progress. J Infect Dis. 2020; 222(9):1417–1421. PMID: 31974551.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The National Influenza Surveillance System of Korea
- Recovery of respiratory syncytial virus, adenovirus, influenza virus , and parainfluenza virus from nasopharyngeal aspirates from children with acute respiratory tract infections
- Epidemiology and Characteristics of Pediatric Respiratory Virus Infection From 2017 to 2019 Focusing on Human Coronavirus: A Retrospective Study of a Single Center in Northwestern Gyeonggi-do
- Changes in respiratory virus infection trends during the COVID-19 pandemic in South Korea: the effectiveness of public health measures
- Changes in epidemiology of parainfluenza virus and respiratory syncytial virus infection during coronavirus disease 2019 pandemic in Korea