Arch Hand Microsurg.
2022 Sep;27(3):234-239. 10.12790/ahm.22.0028.
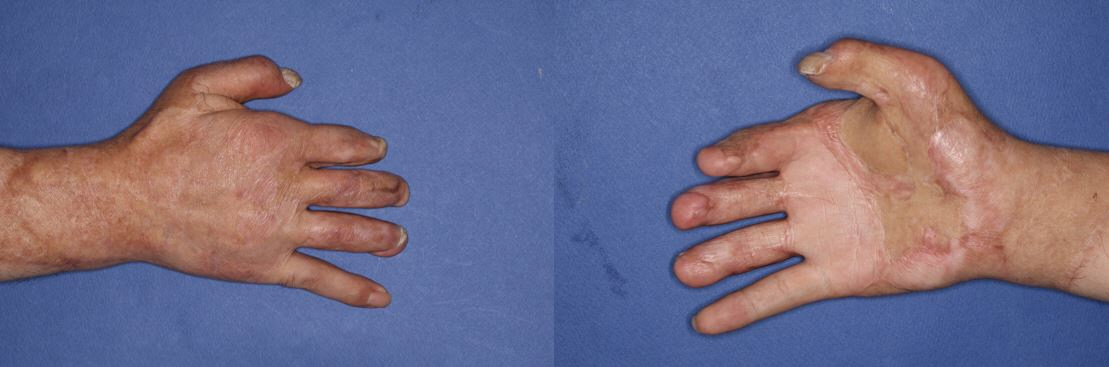
Saving a large volume of soft tissue by using an untailored composite graft after total degloving amputation of the hand: a case report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Gwangmyeong Sung Ae General Hospital, Gwangmyeong, Korea
- KMID: 2532740
- DOI: http://doi.org/10.12790/ahm.22.0028
Abstract
- Total degloving amputations present surgeons with unique challenges to preserve function and prevent amputation of the digits. Obviously, the replantation of avulsed skin is the best option; however, there are situations in which vascular networks are severely contused, making it difficult to restore the circulation, due to the crushing mechanism of injury. As an alternative, defatted or meshed skin grafts from the avulsed skin have been proposed. However, those options have not been proven to guarantee viable digits. Moreover, the application of thinned skin grafts usually results in cosmetically and functionally unsatisfactory outcomes due to the lack of sufficient tissue volume. We present a case in which we successfully saved a large volume of the amputated stump with minimal digit amputation by performing a composite graft of the untailored (i.e., without defatting or meshing) avulsed skin on a totally degloved hand.
Keyword
Figure
Reference
-
References
1. Krishnamoorthy R, Karthikeyan G. Degloving injuries of the hand. Indian J Plast Surg. 2011; 44:227–36.2. Venkatramani H, Sabapathy SR, Zhang D. Revascularization of a circumferential hand and forearm degloving injury using an arteriovenous shunt. J Hand Surg Am. 2021; 46:629. e1-6.3. Ju J, Li J, Hou R. Microsurgery in 46 cases with total hand degloving injury. Asian J Surg. 2015; 38:205–9.4. Wang Y, Rui Y, Zhou J, Li F, Wu Y, Liu J. Successful repair of total hand degloving injury by avulsed skin in situ replantation through vascular transplantation: a case report. Ther Clin Risk Manag. 2018; 14:1429–33.5. Urbaniak JR, Evans JP, Bright DS. Microvascular management of ring avulsion injuries. J Hand Surg Am. 1981; 6:25–30.6. Weinand C. Degloving injuries of upper extremity: a strategy with full thickness skin mesh. World J Plast Surg. 2018; 7:372–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fingertip Reconstruction with Subcutaneous Island Flap and Composite Graft: A Case Report
- Hemorrhagic shock caused by closed internal degloving injury: a case report
- Preserved Superficial Fat Skin Composite Graft for Correction of Burn Scar Contracture of Hand
- Finger Tip Composite Grafting Managed with Moist-Exposed Dressing
- Reconstruction of an Amputated Glans Penis With a Buccal Mucosal Graft: Case Report of a Novel Technique