Arch Hand Microsurg.
2022 Sep;27(3):222-228. 10.12790/ahm.22.0019.
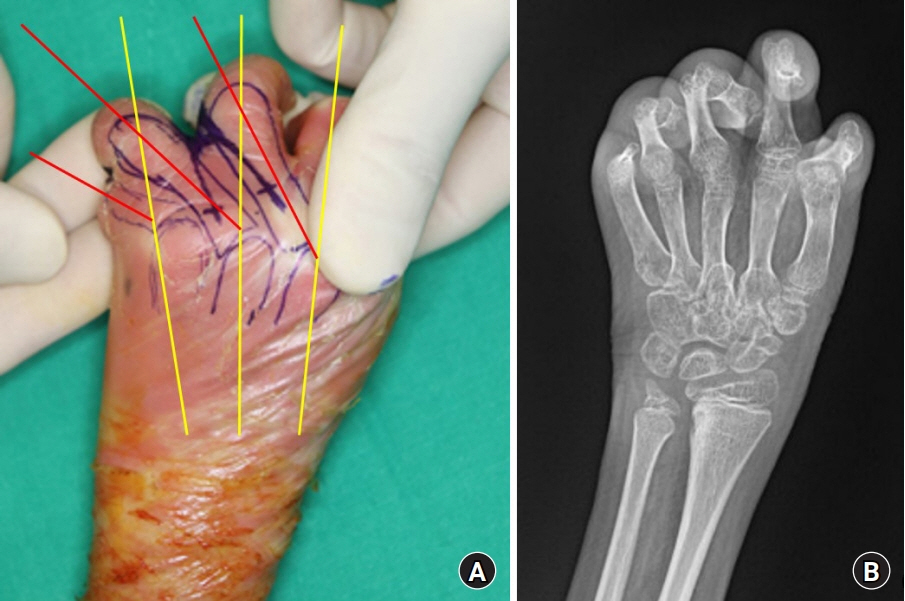
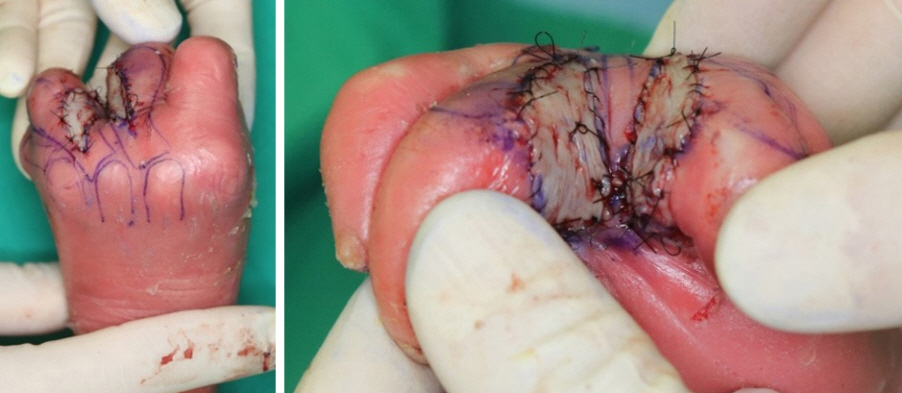
Surgical considerations for syndactyly of the hand in harlequin ichthyosis: a 5-year experience of sequential surgical treatment in a single patient
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Institute for Human Tissue Restoration, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2532738
- DOI: http://doi.org/10.12790/ahm.22.0019
Abstract
- Harlequin ichthyosis (HI) is a rare congenital disease that primarily affects the skin. Its complications include syndactyly, which can cause severe constriction. Surgical release is thought to be helpful, but the details remain unclear due to a lack of data. We share our 5-year experience of a patient with HI with successful outcomes from five syndactyly release operations involving division, local flap interposition, and full-thickness skin grafts. A visible decrease in the ulnar deviation of the metacarpophalangeal joints and a wider range of motion were noted. There were no complications, except for one case of donor site dehiscence that was resolved after minor revision. The surgical design must conform to the anatomical structure, as it can be easily mistaken due to masking of the skin. A suitable donor site is a flat, non-folding surface, such as the lateral thigh.
Figure
Reference
-
References
1. Zapałowicz K, Wygledowska G, Roszkowski T, Bednarowska A. Harlequin ichthyosis--difficulties in prenatal diagnosis. J Appl Genet. 2006; 47:195–7.2. Ahmed H, O'Toole EA. Recent advances in the genetics and management of harlequin ichthyosis. Pediatr Dermatol. 2014; 31:539–46.3. Glick JB, Craiglow BG, Choate KA, et al. Improved management of Harlequin ichthyosis with advances in neonatal intensive care. Pediatrics. 2017; 139:e20161003.4. Overland J, Johnstone B. Surgical management of the hand manifestations of Harlequin ichthyosis. ANZ J Surg. 2019; 89:E325–6.5. Rajpopat S, Moss C, Mellerio J, et al. Harlequin ichthyosis: a review of clinical and molecular findings in 45 cases. Arch Dermatol. 2011; 147:681–6.6. Ahn SJ, Hong JW. Surgical treatment of syndactyly of Harlequin ichthyosis. Arch Hand Microsurg. 2018; 23:184–9.7. Sood RF, Irwin TJ, Taghinia AH. Syndactyly release in the hand: surgical technique. Plast Reconstr Surg. 2022; 149:57e–59e.8. Vekris MD, Lykissas MG, Soucacos PN, Korompilias AV, Beris AE. Congenital syndactyly: outcome of surgical treatment in 131 webs. Tech Hand Up Extrem Surg. 2010; 14:2–7.9. Grahn PM, Nietosvaara NN, Sommarhem AJ, Nietosvaara YA. New simple technique for syndactyly release. Plast Reconstr Surg Glob Open. 2020; 8:e2842.10. Pet MA, Gupta D, Tse RW. Harlequin ichthyosis: a surgical perspective. Pediatr Dermatol. 2016; 33:e327–32.