Ann Hepatobiliary Pancreat Surg.
2022 Aug;26(3):235-243. 10.14701/ahbps.21-173.
Changing incidence and survival of intrahepatic cholangiocarcinoma based on Surveillance, Epidemiology, and End Results Database (2000–2017)
- Affiliations
-
- 1Department of Internal Medicine, East Carolina University/Vidant Medical Center, Greenville, NC, United States
- 2Department of Internal Medicine, State University of New York, Brooklyn, NY, United States
- 3Department of Gastroenterology, East Carolina University/Vidant Medical Center, Greenville, NC, United States
- KMID: 2532639
- DOI: http://doi.org/10.14701/ahbps.21-173
Abstract
- Backgrounds/Aims
Historically, the incidence and prognosis of patients diagnosed with intrahepatic cholangiocarcinoma (ICC) have been inadequately understood. Survival analysis in ICC has yet to be investigated in a population-based study.
Methods
We conducted a retrospective cohort study using the Surveillance, Epidemiology, and End Results Program (SEER) 18 Registry. Risk ratios were estimated via Poisson regression. Hazard ratios for 5-year survival were estimated using hierarchical Cox regression models.
Results
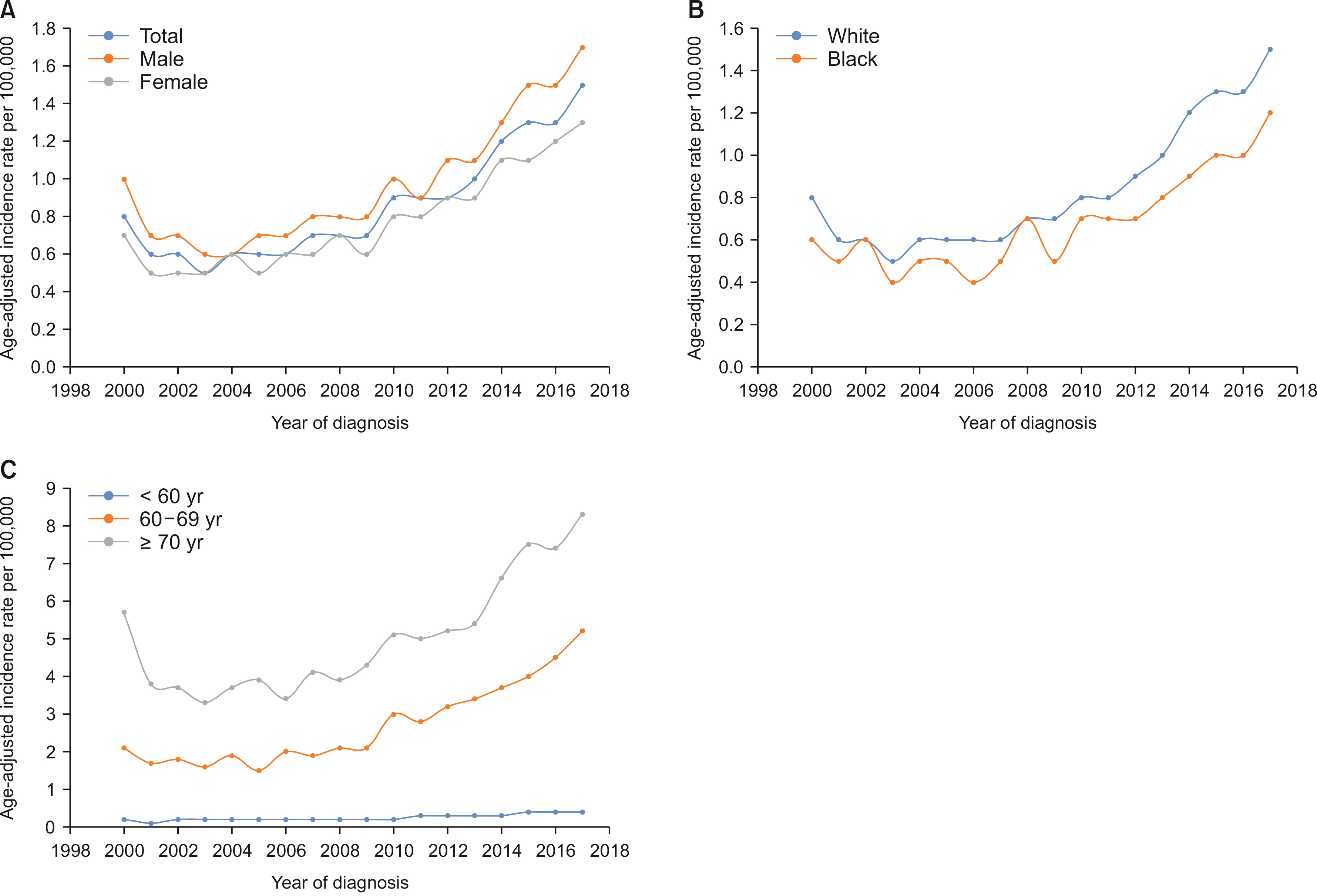
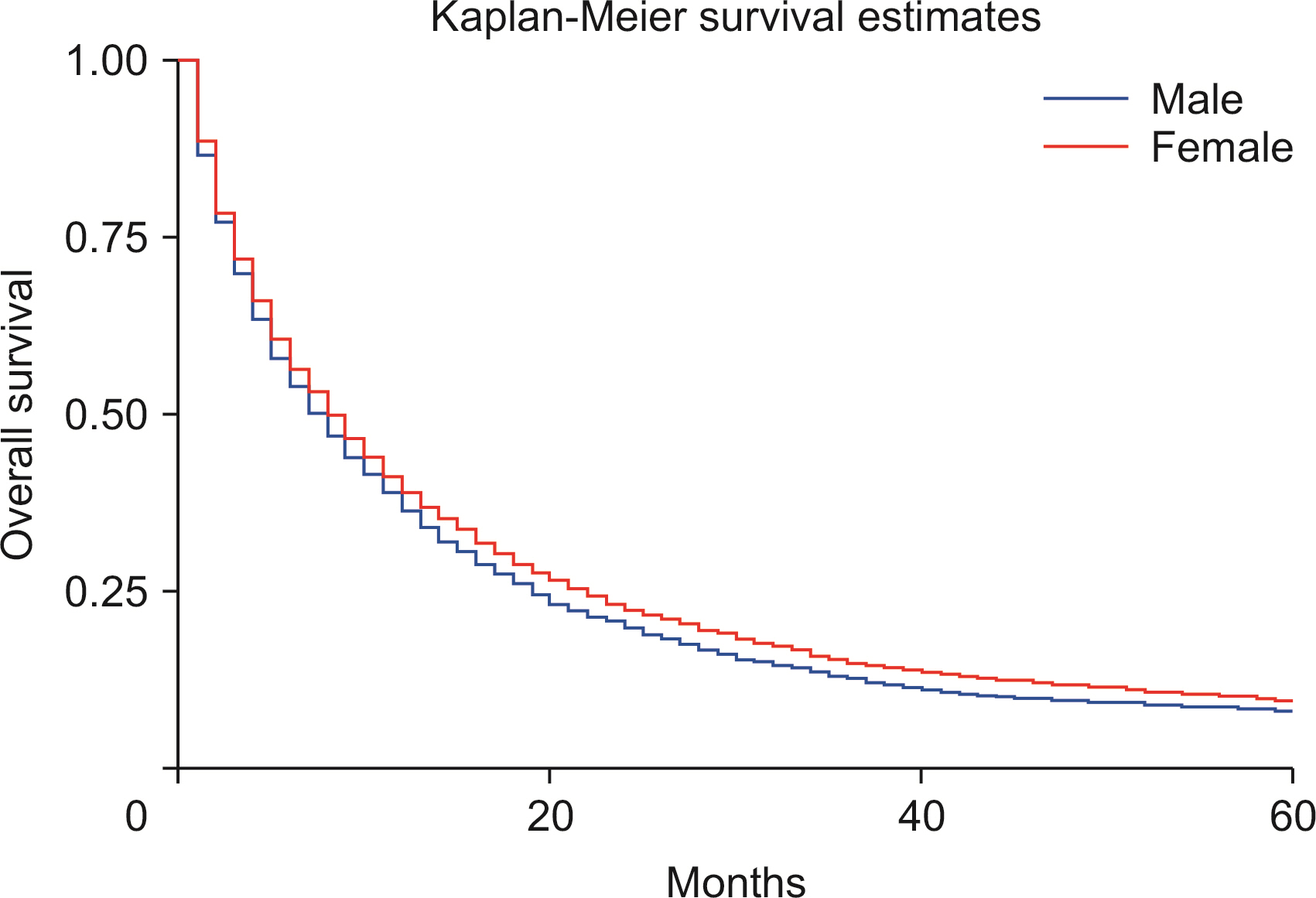
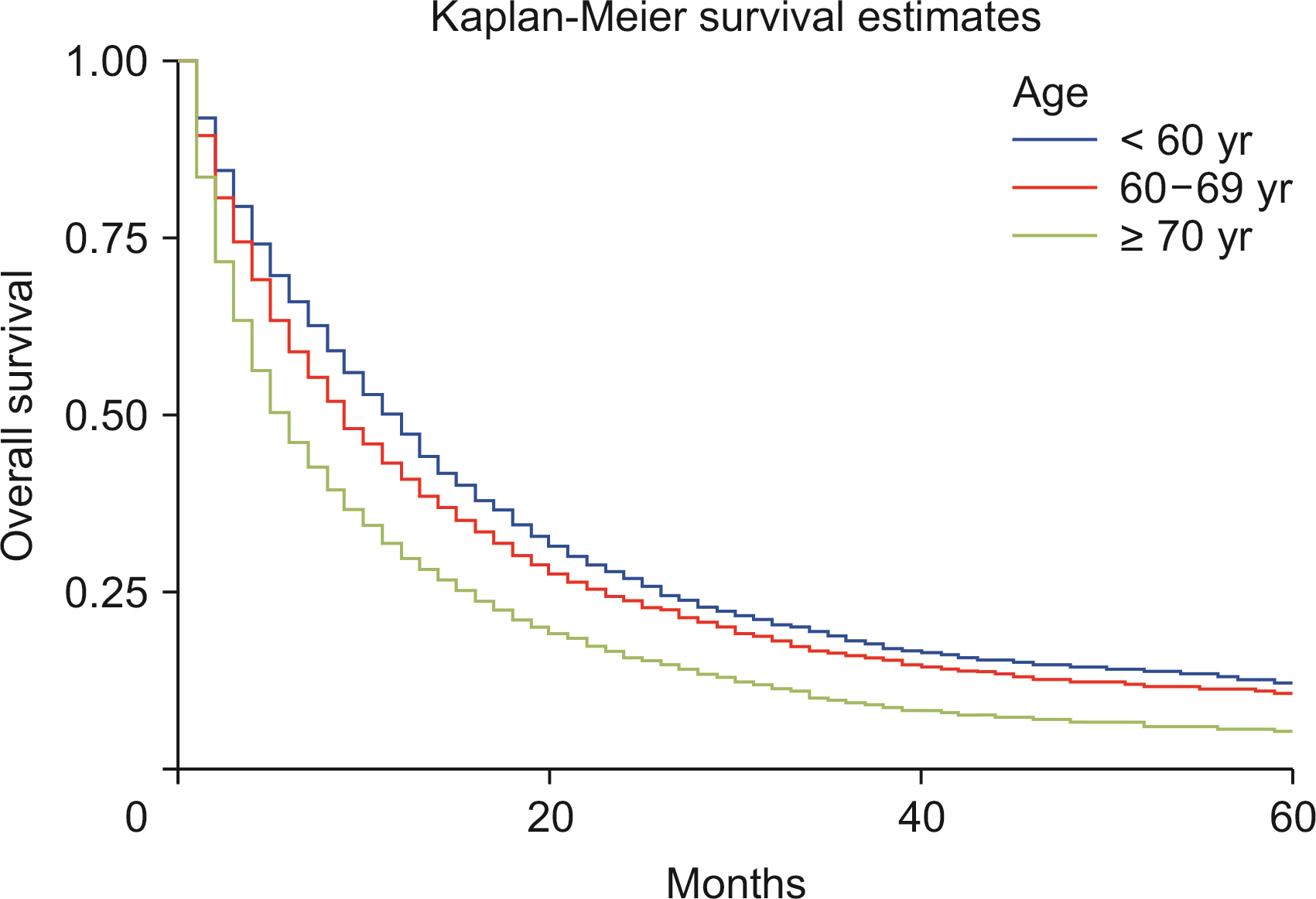
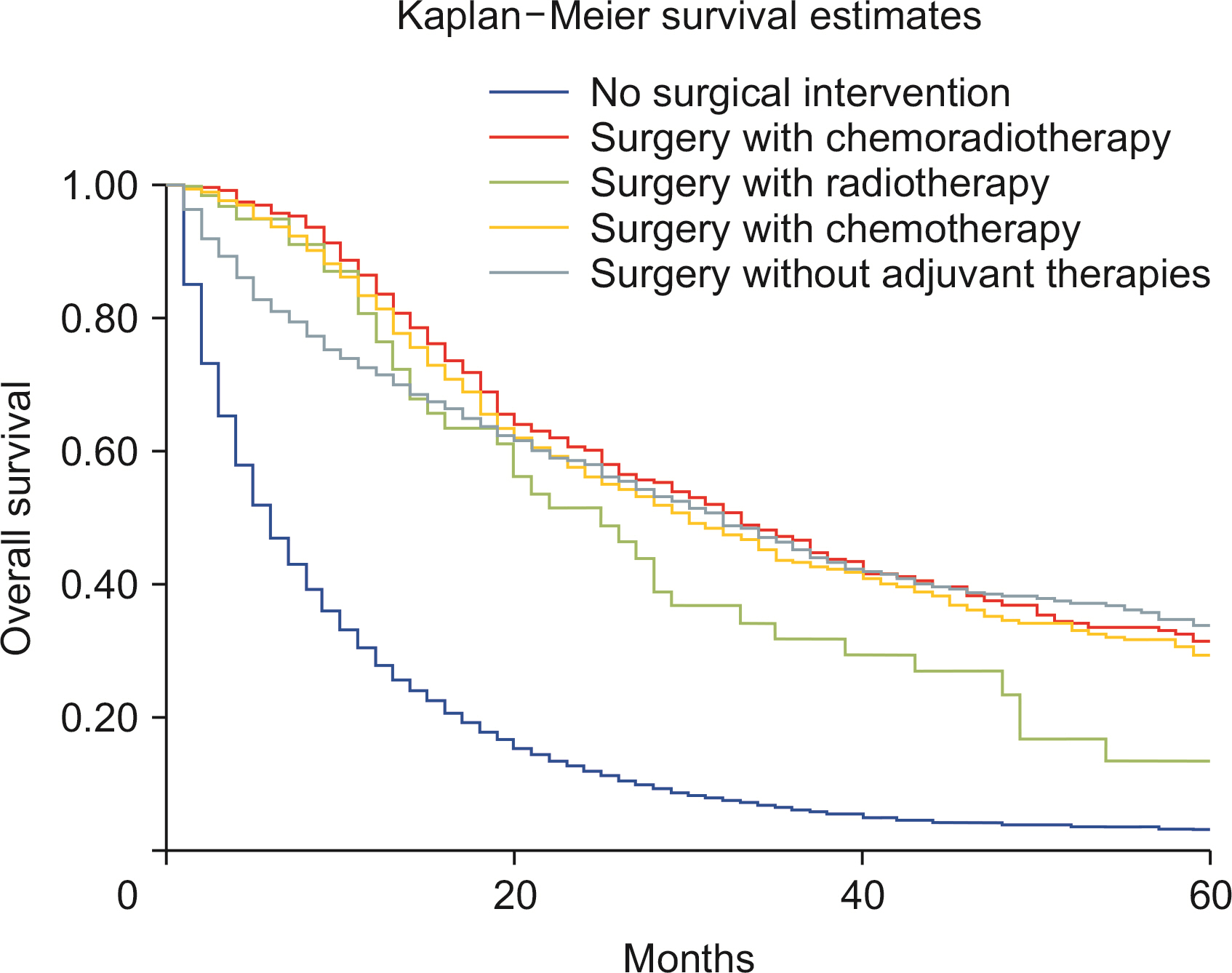
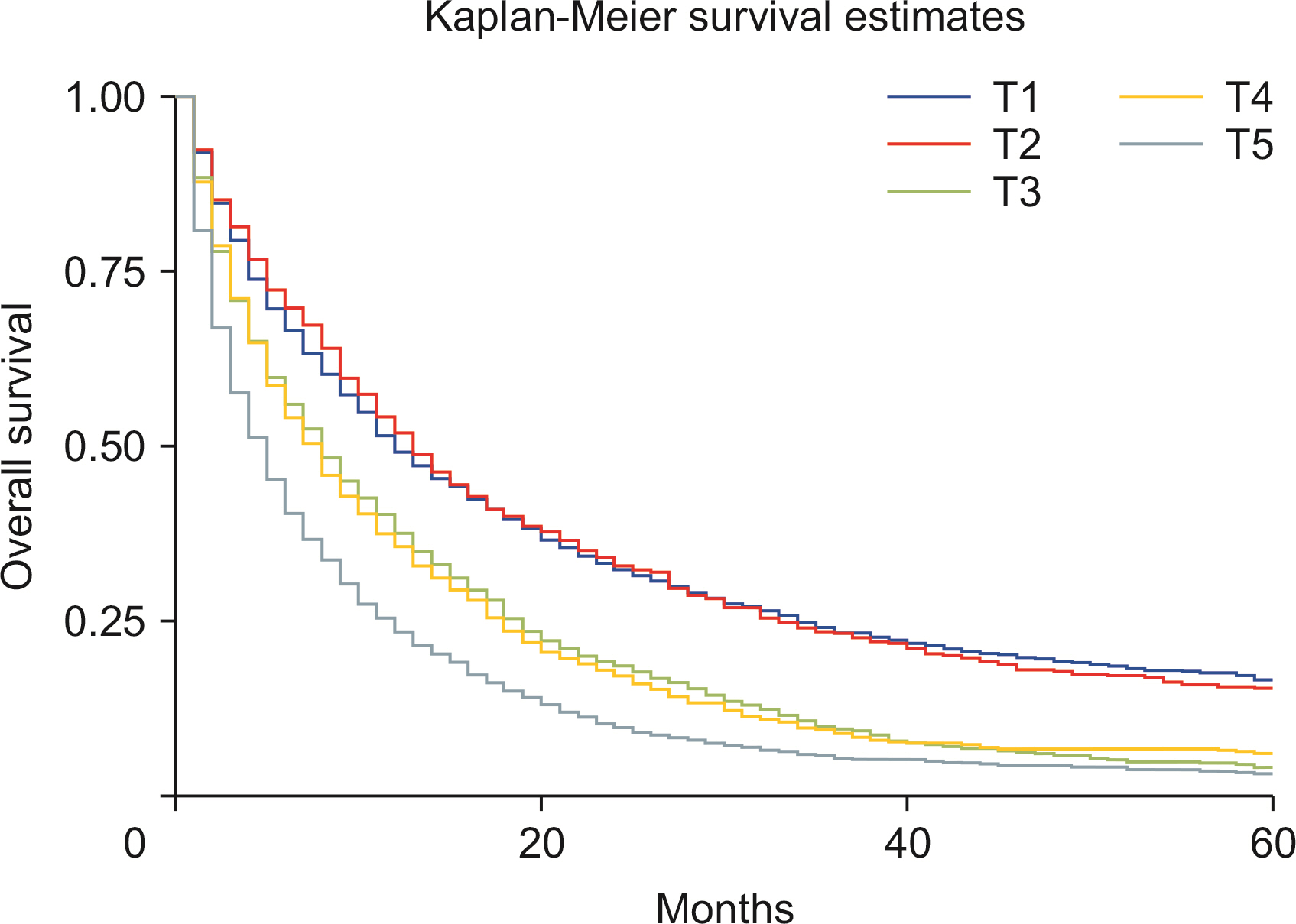
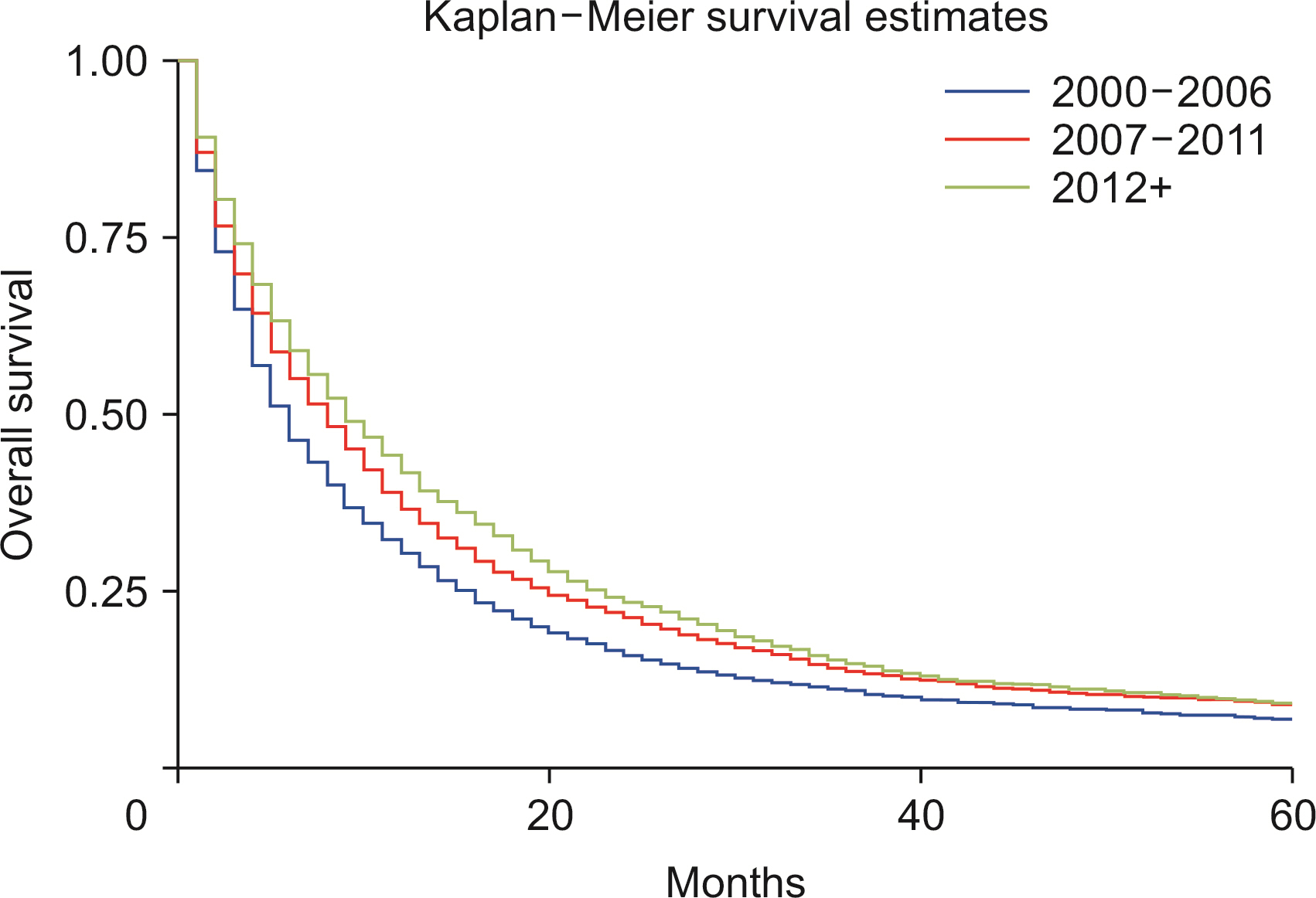
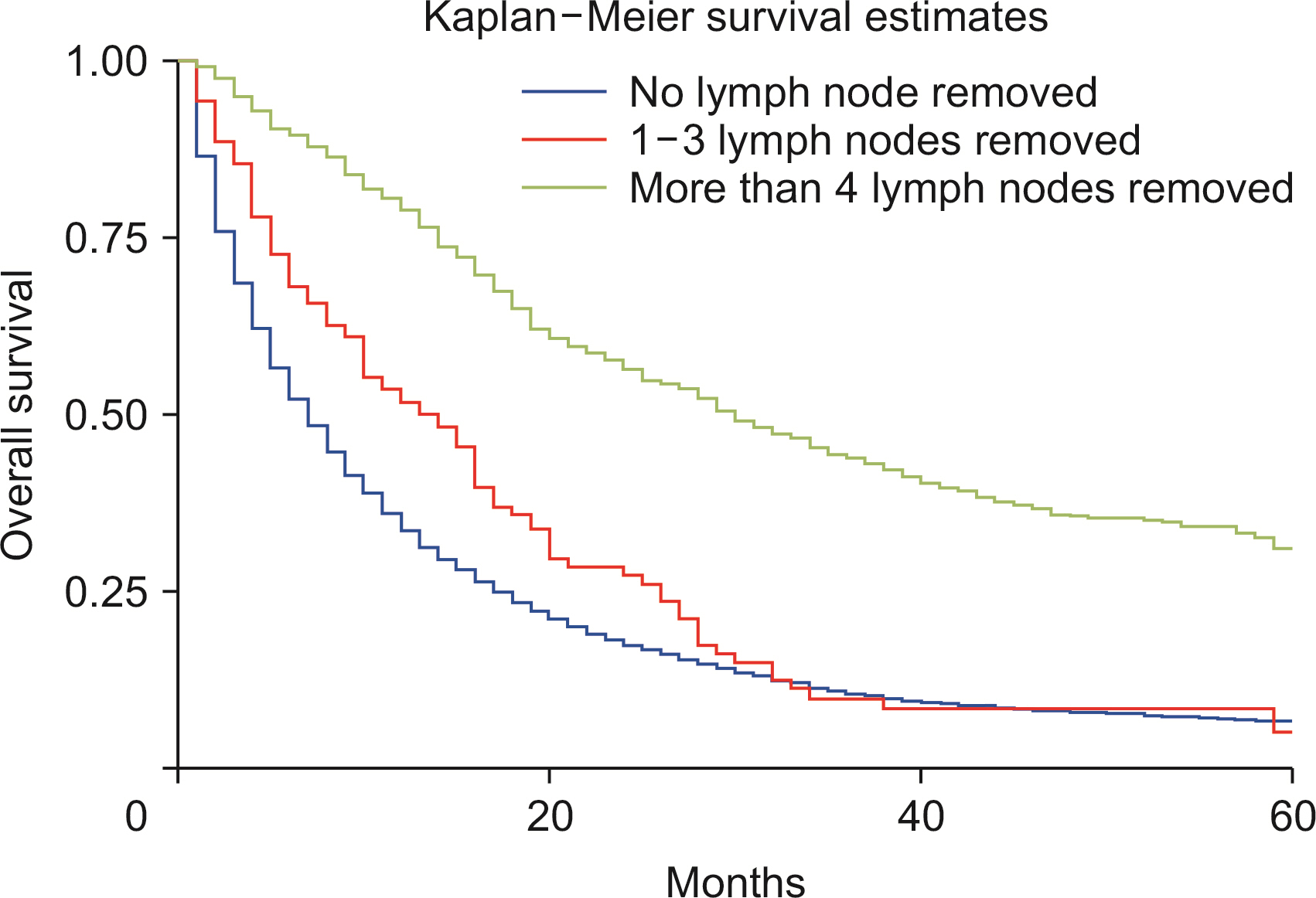
Males show a higher rate of age-adjusted ICC incidence. Blacks carried a decreased risk of ICC diagnosis than Whites, while Asians revealed a higher risk of ICC diagnosis when compared with Whites. The observed survival rates at 12, 36, and 60 months were 36.3%, 12.8%, and 8.1%, respectively. Compared with Whites, Blacks showed an increased risk of death (p < 0.01). Lymph node resection during surgery was associated with a 64.1% reduced risk of mortality (p < 0.01). A higher T stage at diagnosis was associated with poor survival (p < 0.01). Surgery combined with chemoradiotherapy, radiotherapy, or chemotherapy was associated with a reduced risk of mortality compared with nonsurgical interventions (p < 0.01).
Conclusions
ICC incidence has been increasing since 2000, especially in White males. The risk of ICC rises with age. Lymph node removal is associated with better survival. In recent years, survival had worsened, and surgical intervention improved survival compared with nonsurgical management.
Figure
Cited by 2 articles
-
Survival analysis of extrahepatic cholangiocarcinoma based on surveillance, epidemiology, and end results database
Hassam Ali, Joshua Zweigle, Pratik Patel, Brandon Tedder, Rafeh Khan, Saurabh Agrawal
Ann Hepatobiliary Pancreat Surg. 2023;27(2):151-157. doi: 10.14701/ahbps.22-090.Preoperative neutrophil-to-lymphocyte ratio is prognostic for early recurrence after curative intrahepatic cholangiocarcinoma resection
Woo Jin Choi, Fiorella Murillo Perez, Annabel Gravely, Tommy Ivanics, Marco P. A. W. Claasen, Liza Abraham, Phillipe Abreu, Robin Visser, Steven Gallinger, Bettina E. Hansen, Gonzalo Sapisochin
Ann Hepatobiliary Pancreat Surg. 2023;27(2):158-165. doi: 10.14701/ahbps.22-114.
Reference
-
1. Zhang H, Yang T, Wu M, Shen F. 2016; Intrahepatic cholangiocarcinoma: epidemiology, risk factors, diagnosis and surgical management. Cancer Lett. 379:198–205. DOI: 10.1016/j.canlet.2015.09.008. PMID: 26409434.2. Chapman RW. 1999; Risk factors for biliary tract carcinogenesis. Ann Oncol. 10 Suppl 4:308–311. DOI: 10.1023/A:1008313809752. PMID: 10436847.3. Welzel TM, Graubard BI, El-Serag HB, Shaib YH, Hsing AW, Davila JA, et al. 2007; Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: a population-based case-control study. Clin Gastroenterol Hepatol. 5:1221–1228. DOI: 10.1016/j.cgh.2007.05.020. PMID: 17689296. PMCID: PMC2083573.4. Dodson RM, Weiss MJ, Cosgrove D, Herman JM, Kamel I, Anders R, et al. 2013; Intrahepatic cholangiocarcinoma: management options and emerging therapies. J Am Coll Surg. 217:736–750.e4. DOI: 10.1016/j.jamcollsurg.2013.05.021. PMID: 23890842.5. Welzel TM, McGlynn KA, Hsing AW, O'Brien TR, Pfeiffer RM. 2006; Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the United States. J Natl Cancer Inst. 98:873–875. DOI: 10.1093/jnci/djj234. PMID: 16788161.6. DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, et al. 2007; Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 245:755–762. DOI: 10.1097/01.sla.0000251366.62632.d3. PMID: 17457168. PMCID: PMC1877058.7. Nakeeb A, Tran KQ, Black MJ, Erickson BA, Ritch PS, Quebbeman EJ, et al. 2002; Improved survival in resected biliary malignancies. Surgery. 132:555–563. discission 563-564. DOI: 10.1067/msy.2002.127555. PMID: 12407338.8. Hashimoto N, Yachida S, Okano K, Wakabayashi H, Imaida K, Kurokohchi K, et al. 2009; Immunohistochemically detected expression of p27(Kip1) and Skp2 predicts survival in patients with intrahepatic cholangiocarcinomas. Ann Surg Oncol. 16:395–403. DOI: 10.1245/s10434-008-0236-0. PMID: 19034576.9. Surveillance Research Program, NCIs Division of Cancer Control, Population Sciences. 2021. SEER Registries [Internet]. Available from: https://seer.cancer.gov/. cited 2021 Sep 29. Washington, D.C.: National Cancer Institute.10. Surveillance Research Program, National Cancer Institute. 2021. SEER*Stat software version 8.3.9.2 [Internet]. Available from: https://seer.cancer.gov/seerstat/. cited 2021 Sep 29. Washington, D.C.: National Cancer Institute.11. Deadmond MA, Smith-Gagen JA. 2015; Changing incidence of myeloproliferative neoplasms: trends and subgroup risk profiles in the USA, 1973-2011. J Cancer Res Clin Oncol. 141:2131–2138. DOI: 10.1007/s00432-015-1983-5. PMID: 25968903.12. Devesa SS, Donaldson J, Fears T. 1995; Graphical presentation of trends in rates. Am J Epidemiol. 141:300–304. DOI: 10.1093/aje/141.4.300. PMID: 7840107.13. Tyson GL, Ilyas JA, Duan Z, Green LK, Younes M, El-Serag HB, et al. 2014; Secular trends in the incidence of cholangiocarcinoma in the USA and the impact of misclassification. Dig Dis Sci. 59:3103–3110. DOI: 10.1007/s10620-014-3276-2. PMID: 25204668. PMCID: PMC4823008.14. Ailawadhi S, Aldoss IT, Yang D, Razavi P, Cozen W, Sher T, et al. 2012; Outcome disparities in multiple myeloma: a SEER-based comparative analysis of ethnic subgroups. Br J Haematol. 158:91–98. DOI: 10.1111/j.1365-2141.2012.09124.x. PMID: 22533740.15. Shin HR, Oh JK, Masuyer E, Curado MP, Bouvard V, Fang Y, et al. 2010; Comparison of incidence of intrahepatic and extrahepatic cholangiocarcinoma--focus on East and South-Eastern Asia. Asian Pac J Cancer Prev. 11:1159–1166. PMID: 21198257.16. Brito AF, Abrantes AM, Encarnação JC, Tralhão JG, Botelho MF. 2015; Cholangiocarcinoma: from molecular biology to treatment. Med Oncol. 32:245. DOI: 10.1007/s12032-015-0692-x. PMID: 26427701.17. Khan SA, Toledano MB, Taylor-Robinson SD. 2008; Epidemiology, risk factors, and pathogenesis of cholangiocarcinoma. HPB (Oxford). 10:77–82. DOI: 10.1080/13651820801992641. PMID: 18773060. PMCID: PMC2504381.18. Bonnie RJ, Ford MA, Phillips JK. Bonnie RJ, Ford MA, Phillips JK, editors. 2017. Trends in opioid use, harms, and treatment. Pain management and the opioid epidemic: balancing societal and individual benefits and risks of prescription opioid use. Washington, D.C: National Academies Press;p. 187–266. DOI: 10.17226/24781.19. Toy E, Balasubramanian S, Selmi C, Li CS, Bowlus CL. 2011; The prevalence, incidence and natural history of primary sclerosing cholangitis in an ethnically diverse population. BMC Gastroenterol. 11:83. DOI: 10.1186/1471-230X-11-83. PMID: 21767410. PMCID: PMC3160402.20. Gupta A, Dixon E. 2017; Epidemiology and risk factors: intrahepatic cholangiocarcinoma. Hepatobiliary Surg Nutr. 6:101–104. DOI: 10.21037/hbsn.2017.01.02. PMID: 28503557. PMCID: PMC5411279.21. Mody K, Antwi SO, Hodge DO, Ailawadhi S, Roberts L, Bekaii-Saab T. 2018; A SEER-based multi-ethnic picture of advanced intrahepatic cholangiocarcinoma in the United States pre- and post-the advent of gemcitabine/cisplatin. J Gastrointest Oncol. 9:1063–1073. DOI: 10.21037/jgo.2018.07.09. PMID: 30603125. PMCID: PMC6286951.22. Haider AH, Scott VK, Rehman KA, Velopulos C, Bentley JM, Cornwell EE 3rd, et al. 2013; Racial disparities in surgical care and outcomes in the United States: a comprehensive review of patient, provider, and systemic factors. J Am Coll Surg. 216:482–492.e12. DOI: 10.1016/j.jamcollsurg.2012.11.014. PMID: 23318117. PMCID: PMC5995336.23. Spolverato G, Vitale A, Cucchetti A, Popescu I, Marques HP, Aldrighetti L, et al. 2015; Can hepatic resection provide a long-term cure for patients with intrahepatic cholangiocarcinoma? Cancer. 121:3998–4006. DOI: 10.1002/cncr.29619. PMID: 26264223.24. Hartog H, Ijzermans JN, van Gulik TM, Groot Koerkamp B. 2016; Resection of perihilar cholangiocarcinoma. Surg Clin North Am. 96:247–267. DOI: 10.1016/j.suc.2015.12.008. PMID: 27017863.25. Gurusamy KS, Li J, Vaughan J, Sharma D, Davidson BR. 2012; Cardiopulmonary interventions to decrease blood loss and blood transfusion requirements for liver resection. Cochrane Database Syst Rev. 2012:CD007338. DOI: 10.1002/14651858.CD007338.pub3. PMCID: PMC6718233. PMID: 22592720.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence, mortality, and survival of liver cancer using Korea central cancer registry database: 1999–2019
- Survival analysis of extrahepatic cholangiocarcinoma based on surveillance, epidemiology, and end results database
- A personalized prognostic model for long-term survival in patients with intrahepatic cholangiocarcinoma: a retrospective cohort study
- Review: Analysis of Survival Rate and Prognostic Factors of Intrahepatic Cholangiocarcinoma: 318 Cases in Single Institute
- Surgical Treatment for Intrahepatic Cholangiocarcinoma