Korean J Gastroenterol.
2022 Jul;80(1):38-42. 10.4166/kjg.2022.066.
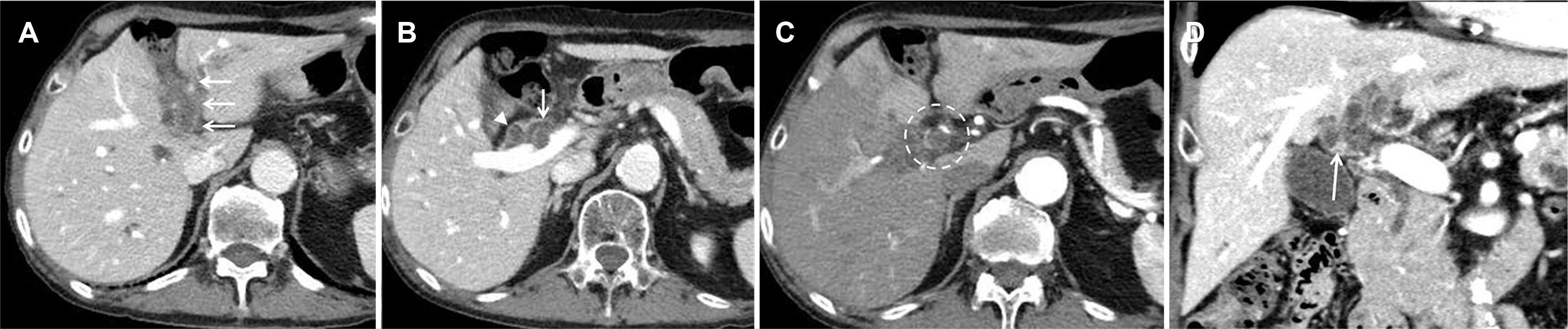
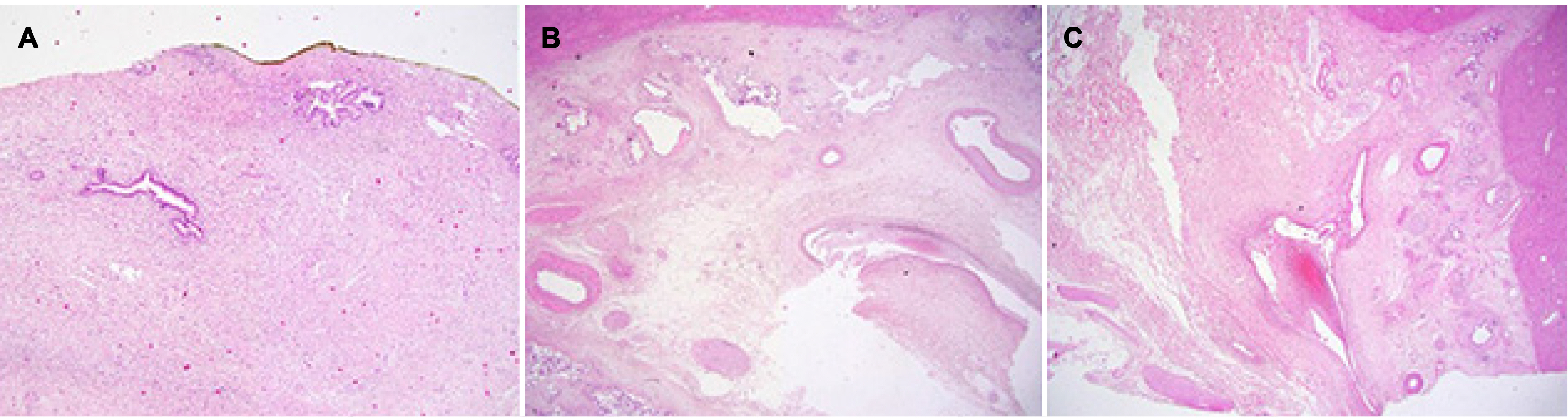
Portal Biliopathy Misdiagnosed as Hilar Cholangiocarcinoma
- Affiliations
-
- 1Departments of Internal Medicine, Hallym University College of Medicine, Anyang, Korea
- 2Departments of Pathology, Hallym University College of Medicine, Anyang, Korea
- 3Departments of Radiology, Hallym University College of Medicine, Anyang, Korea
- KMID: 2532166
- DOI: http://doi.org/10.4166/kjg.2022.066
Abstract
- Portal biliopathy refers to the changes in the bile duct caused by portal vein thrombosis or obstruction. It is assumed to be caused by cavernous transformation due to the development of the venous system surrounding the bile duct, but the exact pathology is still unknown. Biliary morphologic abnormalities of portal biliopathy are discovered incidentally on radiographic images, but it is sometimes difficult to differentiate them from cholangiocarcinoma. Given the poor prognosis of cholangiocarcinoma, a surgical approach can be considered when the diagnosis is uncertain. Herein, we report a case of portal biliopathy with bile ductal wall thickening, which was diagnosed after surgical resection was performed due to the presumed diagnosis of cholangiocarcinoma.
Keyword
Figure
Reference
-
1. Chattopadhyay S, Nundy S. 2012; Portal biliopathy. World J Gastroenterol. 18:6177–6182. DOI: 10.3748/wjg.v18.i43.6177. PMID: 23180936. PMCID: PMC3501764.2. Sogaard KK, Astrup LB, Vilstrup H, Gronbaek H. 2007; Portal vein thrombosis; risk factors, clinical presentation and treatment. BMC Gastroenterol. 7:34. DOI: 10.1186/1471-230X-7-34. PMID: 17697371. PMCID: PMC1976099.3. Song SH, Seo KH, Kim JH, et al. 1999; A case of obstructive jaundice caused by cavernous transformation of the portal vein. Clin Endosc. 19:999–1004.4. Sarin SK, Agarwal SR. 2002; Extrahepatic portal vein obstruction. Semin Liver Dis. 22:43–58. DOI: 10.1055/s-2002-23206. PMID: 11928078.5. Shin SM, Kim S, Lee JW, et al. 2005; Magnetic resonance imaging findings of portal biliopathy. J Korean Soc Radiol. 52:123–132. DOI: 10.3348/jkrs.2005.52.2.123.6. Menias CO, Surabhi VR, Prasad SR, Wang HL, Narra VR, Chintapalli KN. 2008; Mimics of cholangiocarcinoma: spectrum of disease. Radiographics. 28:1115–1129. DOI: 10.1148/rg.284075148. PMID: 18635632.7. Clayton RA, Clarke DL, Currie EJ, Madhavan KK, Parks RW, Garden OJ. 2003; Incidence of benign pathology in patients undergoing hepatic resection for suspected malignancy. Surgeon. 1:32–38. DOI: 10.1016/S1479-666X(03)80006-9. PMID: 15568422.8. Stewart CJ, Mills PR, Carter R, et al. 2001; Brush cytology in the assessment of pancreatico-biliary strictures: a review of 406 cases. J Clin Pathol. 54:449–455. DOI: 10.1136/jcp.54.6.449. PMID: 11376018. PMCID: PMC1731449.9. Yoon SB, Moon SH, Ko SW, Lim H, Kang HS, Kim JH. Brush cytology, forceps biopsy, or endoscopic ultrasound-guided sampling for diagnosis of bile duct cancer: a meta-analysis. Dig Dis Sci. 2021; Jul. 14. [Epub ahead of print]. DOI: 10.1007/s10620-021-07138-4. PMID: 34263382.10. Jeon TY, Choi MH, Yoon SB, Soh JS, Moon SH. 2022; Systematic review and meta-analysis of percutaneous transluminal forceps biopsy for diagnosing malignant biliary strictures. Eur Radiol. 32:1747–1756. DOI: 10.1007/s00330-021-08301-1. PMID: 34537877.11. Manzano-Robleda Mdel C, Barranco-Fragoso B, Uribe M, Méndez-Sánchez N. 2015; Portal vein thrombosis: what is new? Ann Hepatol. 14:20–27. DOI: 10.1016/s1665-2681(19)30797-5. PMID: 25536638.12. Franceschet I, Zanetto A, Ferrarese A, Burra P, Senzolo M. 2016; Therapeutic approaches for portal biliopathy: a systematic review. World J Gastroenterol. 22:9909–9920. DOI: 10.3748/wjg.v22.i45.9909. PMID: 28018098. PMCID: PMC5143758.13. Kim S, Yun YM, Kim IS, et al. 2016; Clinical pharmacogenetic testing and application: laboratory medicine clinical practice guidelines part 2. Lab Med Online. 6:193–213. DOI: 10.3343/lmo.2016.6.4.193.14. Kim JS, Kim BW. 2018; Management of patients on antithrombotic agents undergoing endoscopy. Korean J Gastroenterol. 71:282–285. DOI: 10.4166/kjg.2018.71.5.282. PMID: 29791987.15. Gallego C, Velasco M, Marcuello P, Tejedor D, De Campo L, Friera A. 2002; Congenital and acquired anomalies of the portal venous system. Radiographics. 22:141–159. DOI: 10.1148/radiographics.22.1.g02ja08141. PMID: 11796904.16. Corvera CU, Blumgart LH, Darvishian F, et al. 2005; Clinical and pathologic features of proximal biliary strictures masquerading as hilar cholangiocarcinoma. J Am Coll Surg. 201:862–869. DOI: 10.1016/j.jamcollsurg.2005.07.011. PMID: 16310689.17. Wakai T, Shirai Y, Sakata J, et al. 2012; Clinicopathological features of benign biliary strictures masquerading as biliary malignancy. Am Surg. 78:1388–1391. DOI: 10.1177/000313481207801232. PMID: 23265129.18. Roos E, Hubers LM, Coelen RJS, et al. 2018; IgG4-associated cholangitis in patients resected for presumed perihilar cholangiocarcinoma: a 30-year tertiary care experience. Am J Gastroenterol. 113:765–772. DOI: 10.1038/s41395-018-0036-5. PMID: 29549357.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Portal Vein Occlusion after Biliary Metal Stent Placement in Hilar Cholangiocarcinoma
- Current Status and Recent Update of Imaging Evaluation for Peri-Hilar Cholangiocarcinoma
- Portal biliopathy treated with endoscopic biliary stenting
- Hilar Cholangiocarcinoma
- Clinical features and imaging findings of portal biliopathy