J Yeungnam Med Sci.
2022 Jul;39(3):262-265. 10.12701/jyms.2022.00220.
Prolonged oral sildenafil use-induced Mondor disease: a case report
- Affiliations
-
- 1Department of Emergency Medicine, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2532081
- DOI: http://doi.org/10.12701/jyms.2022.00220
Abstract
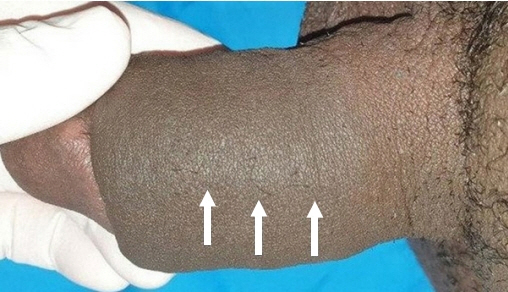
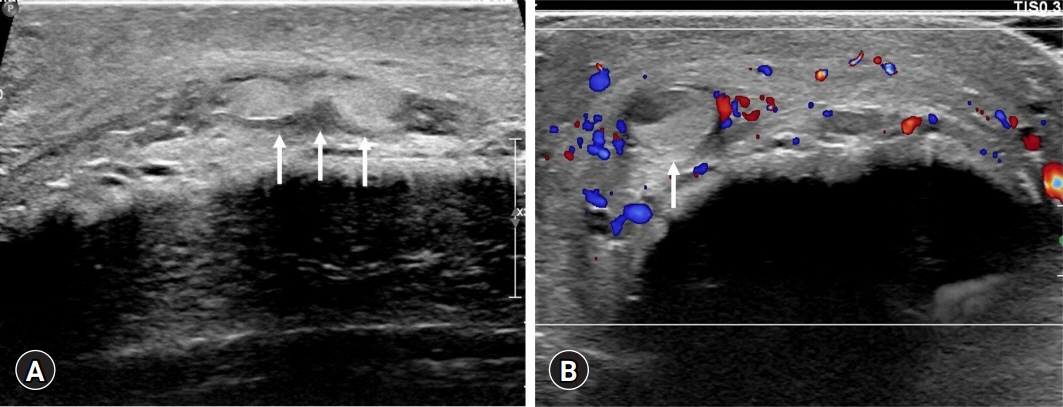
- Penile Mondor disease (MD) is a palpable, painful, subcutaneous induration caused by superficial dorsal penile vein thrombosis. We report a case of penile MD that was suspected to be related to prolonged oral sildenafil use. A 46-year-old man visited our emergency department with sustained penile pain and swelling that began 7 hours after sexual intercourse. He had used oral sildenafil intermittently for 11 years and engaged in sexual intercourse the previous night after taking sildenafil. Examination revealed no evidence of intercourse-related trauma to the genital area or an increase in penile skin temperature. However, penile swelling and tenderness over the protruding dorsal penile vein were noted. A color Doppler ultrasound examination was performed immediately, which showed hyperechoic thrombosis in the right superficial dorsal penile vein that was dilated, with soft tissue swelling and no detectable flow signal in the thrombotic lesion. The patient was diagnosed as having penile MD. The patient was treated conservatively. Some reports have indicated the involvement of sildenafil in thrombogenesis. Physicians should be aware that prolonged oral sildenafil use may be associated with penile MD.
Keyword
Figure
Reference
-
References
1. Amano M, Shimizu T. Mondor’s disease: a review of the literature. Intern Med. 2018; 57:2607–12.
Article2. Laroche JP, Galanaud J, Labau D, Van Kien AK, Brisot D, Boge G, et al. Mondor’s disease: what’s new since 1939? Thromb Res. 2012; 130(Suppl 1):S56–8.
Article3. Walsh JC, Poimboeuf S, Garvin DS. A common presentation to an uncommon disease: Penile Mondor’s disease: a case report and literature review. Int Med Case Rep J. 2014; 7:155–7.4. Kadioglu H, Yildiz S, Ersoy YE, Yücel S, Müslümanoğlu M. An unusual case caused by a common reason: Mondor’s disease by oral contraceptives. Int J Surg Case Rep. 2013; 4:855–7.
Article5. Rufa A, Cerase A, Monti L, Dotti MT, Giorgio A, Sicurelli F, et al. Recurrent venous thrombosis including cerebral venous sinus thrombosis in a patient taking sildenafil for erectile dysfunction. J Neurol Sci. 2007; 260:293–5.
Article6. Al-Mwalad M, Loertzer H, Wicht A, Fornara P. Subcutaneous penile vein thrombosis (penile Mondor’s disease): pathogenesis, diagnosis, and therapy. Urology. 2006; 67:586–8.
Article7. Sasso F, Gulino G, Basar M, Carbone A, Torricelli P, Alcini E. Penile Mondors’ disease: an underestimated pathology. Br J Urol. 1996; 77:729–32.
Article8. Kim KK, Kim DG, Ku YH, Lee YJ, Kim WC, Kim OJ, et al. Bilateral cerebral hemispheric infarction associated with sildenafil citrate (Viagra) use. Eur J Neurol. 2008; 15:306–8.
Article9. Karti DT, Karti O, Aktert D, Gokcay F, Celebisoy N. Sildenafil-related cerebral venous sinus thrombosis and papilledema: a case report of a rare entity. Neurol Sci. 2017; 38:1727–9.
Article10. Haslam RJ, Dickinson NT, Jang EK. Cyclic nucleotides and phosphodiesterases in platelets. Thromb Haemost. 1999; 82:412–23.
Article11. Li Z, Xi X, Gu M, Feil R, Ye RD, Eigenthaler M, et al. A stimulatory role for cGMP-dependent protein kinase in platelet activation. Cell. 2003; 112:77–86.
Article12. Zusman RM, Morales A, Glasser DB, Osterloh IH. Overall cardiovascular profile of sildenafil citrate. Am J Cardiol. 1999; 83(5A):35C–44C.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mondor's Disease after Operation for Axillary Osmidrosis: A Case Report
- Two Cases of Mondor's Disease in Patients with Malignant Lymphoma
- A Case of Mondor's Disease
- Acute Unilateral Vestibular Weakness Following Sildenafil Ingestion
- Pulsed and Color Doppler Sonographic Findings of Penile Mondor's Disease