Diabetes Metab J.
2022 Jul;46(4):567-577. 10.4093/dmj.2021.0160.
Comparative Effects of Sodium-Glucose Cotransporter 2 Inhibitor and Thiazolidinedione Treatment on Risk of Stroke among Patients with Type 2 Diabetes Mellitus
- Affiliations
-
- 1Department of Internal Medicine, Dongguk University Ilsan Hospital, Goyang, Korea
- 2Data Science Team, Hanmi Pharm. Co. Ltd., Seoul, Korea
- KMID: 2531961
- DOI: http://doi.org/10.4093/dmj.2021.0160
Abstract
- Background
Although cardiovascular outcome trials using sodium-glucose cotransporter-2 inhibitors (SGLT-2i) showed a reduction in risk of 3-point major adverse cardiovascular events (MACE), they did not demonstrate beneficial effects on stroke risk. Additionally, meta-analysis showed SGLT-2i potentially had an adverse effect on stroke risk. Contrarily, pioglitazone, a type of thiazolidinedione (TZD), has been shown to reduce recurrent stroke risk. Thus, we aimed to compare the effect of SGLT-2i and TZD on the risk of stroke in type 2 diabetes mellitus (T2DM) patients.
Methods
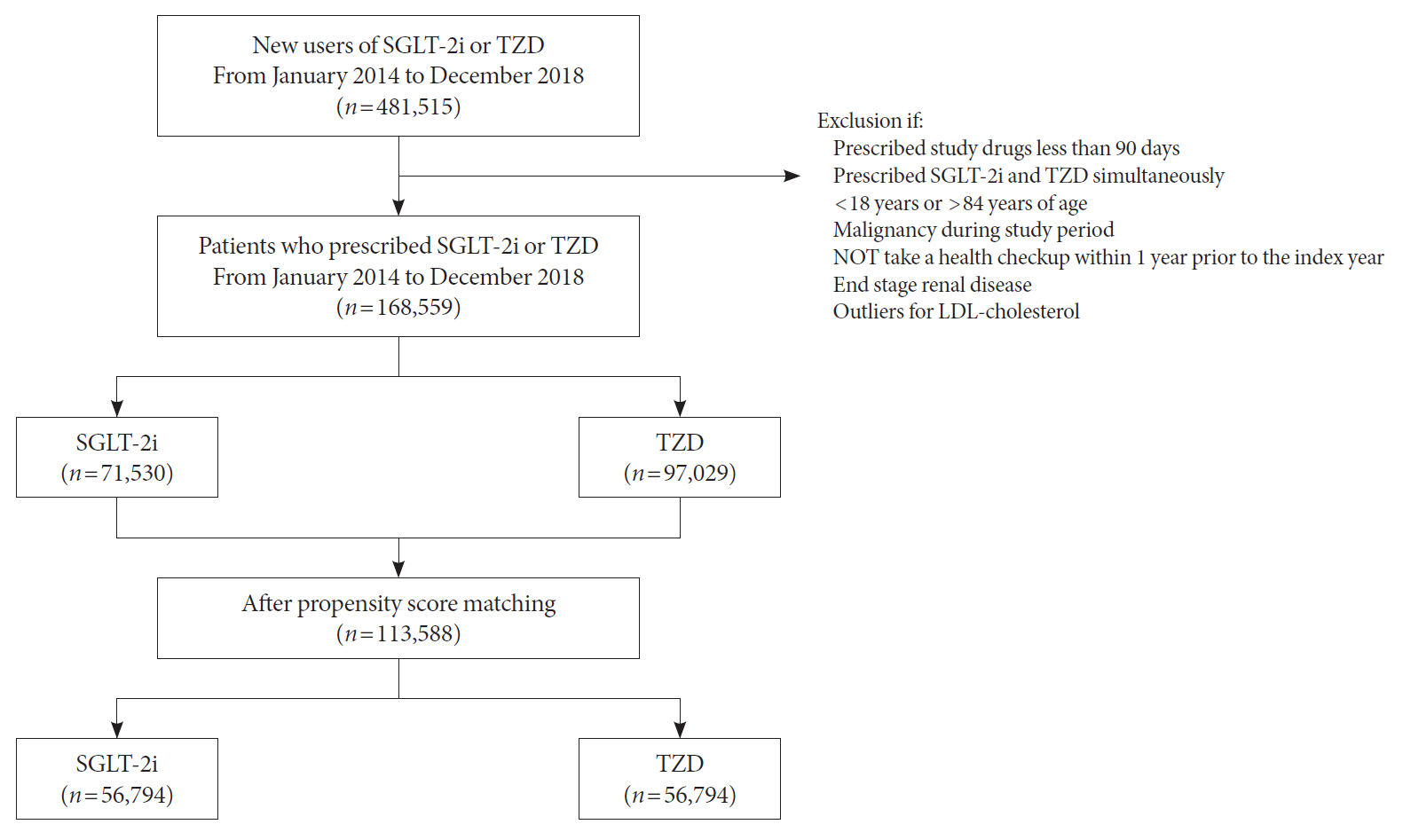
Using the Korean National Health Insurance Service data, we compared a 1:1 propensity score-matched cohort of patients who used SGLT-2i or TZD from January 2014 to December 2018. The primary outcome was stroke. The secondary outcomes were myocardial infarction (MI), cardiovascular death, 3-point MACE, and heart failure (HF).
Results
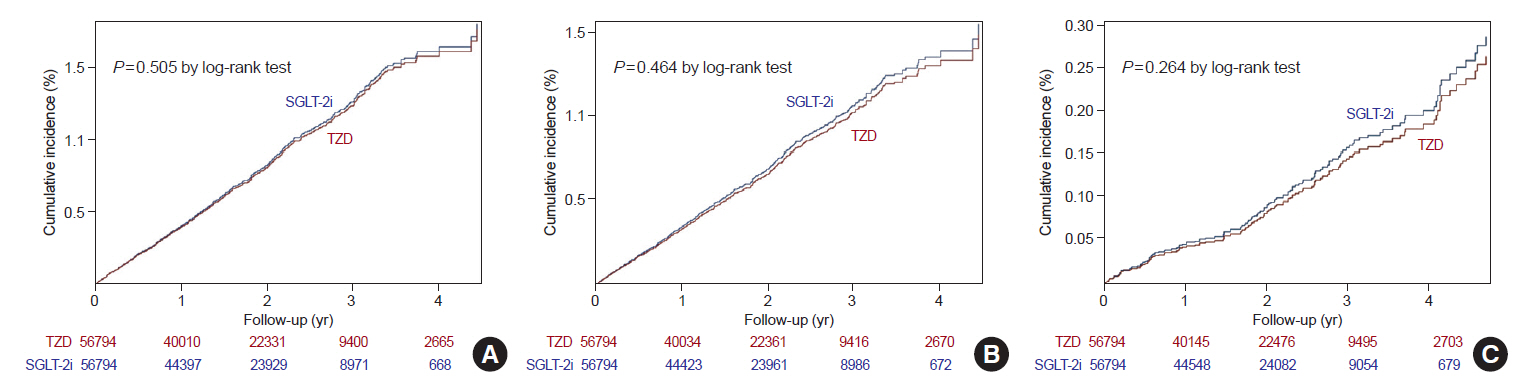
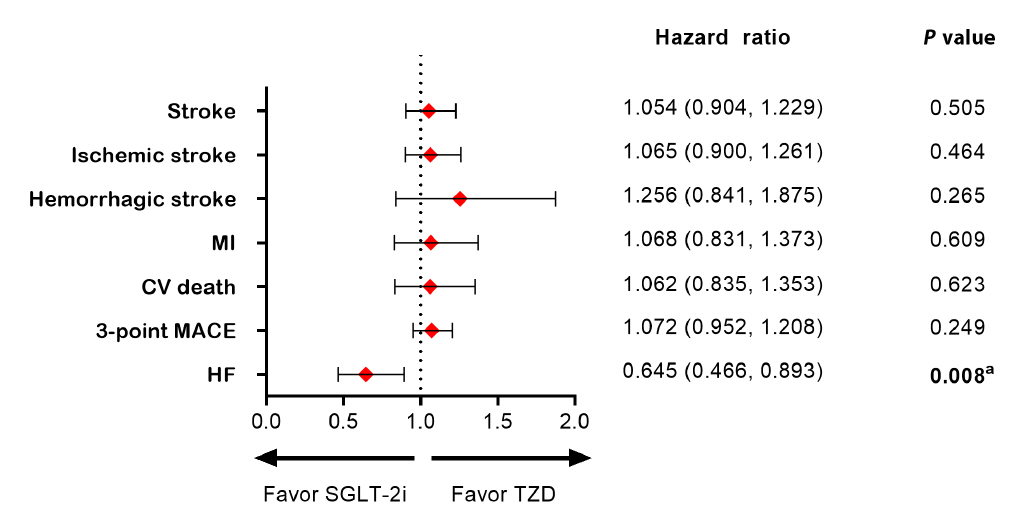
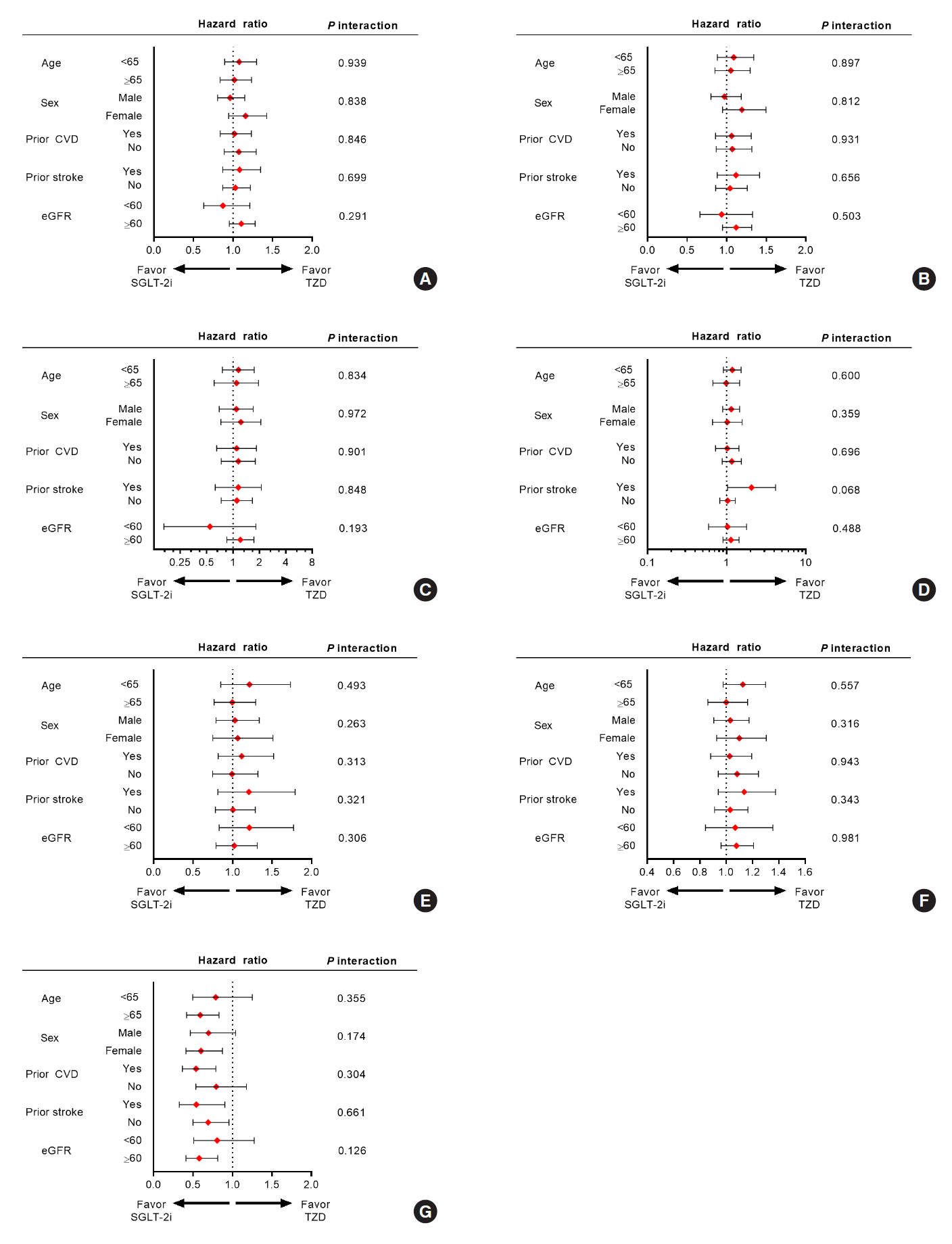
After propensity-matching, each group included 56,794 patients. Baseline characteristics were well balanced. During the follow-up, 862 patients were newly hospitalized for stroke. The incidence rate of stroke was 4.11 and 4.22 per 1,000 person-years for the TZD and SGLT-2i groups respectively. The hazard ratio (HR) of stroke was 1.054 (95% confidence interval [CI], 0.904 to 1.229) in the SGLT-2i group compared to the TZD group. There was no difference in the risk of MI, cardiovascular death, 3-point MACE between groups. Hospitalization for HF was significantly decreased in SGLT-2i-treated patients (HR, 0.645; 95% CI, 0.466 to 0.893). Results were consistent regardless of prior cardiovascular disease.
Conclusion
In this real-world data, the risk of stroke was comparable in T2DM patients treated with SGLT-2i or TZD.
Figure
Cited by 1 articles
-
Cardiovascular Disease & Diabetes Statistics in Korea: Nationwide Data 2010 to 2019
Jin Hwa Kim, Junyeop Lee, Kyungdo Han, Jae-Taek Kim, Hyuk-Sang Kwon
Diabetes Metab J. 2024;48(6):1084-1092. doi: 10.4093/dmj.2024.0275.
Reference
-
1. Martin-Timon I, Sevillano-Collantes C, Segura-Galindo A, Del Canizo-Gomez FJ. Type 2 diabetes and cardiovascular disease: have all risk factors the same strength? World J Diabetes. 2014; 5:444–70.
Article2. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018; 17:83.
Article3. Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008; 118:2702–9.4. American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2020. Diabetes Care. 2020; 43(Suppl 1):S98–110.5. Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018: a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018; 41:2669–701.
Article6. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019; 380:347–57.
Article7. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017; 377:644–57.
Article8. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–28.
Article9. Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020; 383:1425–35.
Article10. Wu JH, Foote C, Blomster J, Toyama T, Perkovic V, Sundstrom J, et al. Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, and major safety outcomes in adults with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2016; 4:411–9.
Article11. Arnott C, Li Q, Kang A, Neuen BL, Bompoint S, Lam CS, et al. Sodium-glucose cotransporter 2 inhibition for the prevention of cardiovascular events in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. J Am Heart Assoc. 2020; 9:e014908.
Article12. Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019; 393:31–9.
Article13. Wilcox R, Bousser MG, Betteridge DJ, Schernthaner G, Pirags V, Kupfer S, et al. Effects of pioglitazone in patients with type 2 diabetes with or without previous stroke: results from PROactive (PROspective pioglitAzone Clinical Trial In macroVascular Events 04). Stroke. 2007; 38:865–73.
Article14. Lee YH, Han K, Ko SH, Ko KS, Lee KU; Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Data analytic process of a nationwide population-based study using national health information database established by National Health Insurance Service. Diabetes Metab J. 2016; 40:79–82.
Article15. Noh J. The diabetes epidemic in Korea. Endocrinol Metab (Seoul). 2016; 31:349–53.
Article16. Lee SE, Han K, Baek JY, Ko KS, Lee KU, Koh EH, et al. Association between diabetic retinopathy and Parkinson disease: the Korean National Health Insurance Service Database. J Clin Endocrinol Metab. 2018; 103:3231–8.
Article17. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009; 28:3083–107.
Article18. Marx N, McGuire DK, Perkovic V, Woerle HJ, Broedl UC, von Eynatten M, et al. Composite primary end points in cardiovascular outcomes trials involving type 2 diabetes patients: should unstable angina be included in the primary end point? Diabetes Care. 2017; 40:1144–51.
Article19. Malhotra K, Katsanos AH, Lambadiari V, Goyal N, Palaiodimou L, Kosmidou M, et al. GLP-1 receptor agonists in diabetes for stroke prevention: a systematic review and meta-analysis. J Neurol. 2020; 267:2117–22.
Article20. Fisher M. The challenge of mixed cerebrovascular disease. Ann N Y Acad Sci. 2010; 1207:18–22.
Article21. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article22. Ohira T, Shahar E, Chambless LE, Rosamond WD, Mosley TH Jr, Folsom AR. Risk factors for ischemic stroke subtypes: the Atherosclerosis Risk in Communities study. Stroke. 2006; 37:2493–8.23. Ryu WS, Schellingerhout D, Hong KS, Jeong SW, Jang MU, Park MS, et al. White matter hyperintensity load on stroke recurrence and mortality at 1 year after ischemic stroke. Neurology. 2019; 93:e578–89.
Article24. Staels B. Cardiovascular protection by sodium glucose cotransporter 2 inhibitors: potential mechanisms. Am J Med. 2017; 130(6S):S30–9.
Article25. Semenkovich CF. Insulin resistance and atherosclerosis. J Clin Invest. 2006; 116:1813–22.
Article26. Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011; 14:575–85.
Article27. Li AC, Brown KK, Silvestre MJ, Willson TM, Palinski W, Glass CK. Peroxisome proliferator-activated receptor gamma ligands inhibit development of atherosclerosis in LDL receptor-deficient mice. J Clin Invest. 2000; 106:523–31.28. Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, MassiBenedetti M, Moules IK, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomized controlled trial. Lancet. 2005; 366:1279–89.29. Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016; 374:1321–31.
Article30. Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016; 375:323–34.
Article31. Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, Jafar TH, Heerspink HJ, Mann JF, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013; 382:339–52.
Article32. Giugliano D, Ceriello A, De Nicola L, Perrone-Filardi P, Cosentino F, Esposito K. Primary versus secondary cardiorenal prevention in type 2 diabetes: which newer anti-hyperglycaemic drug matters? Diabetes Obes Metab. 2020; 22:149–57.
Article33. Kristensen SL, Rorth R, Jhund PS, Docherty KF, Sattar N, Preiss D, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019; 7:776–85.
Article34. Benedetto U, Head SJ, Angelini GD, Blackstone EH. Statistical primer: propensity score matching and its alternatives. Eur J Cardiothorac Surg. 2018; 53:1112–7.
Article35. Gordon DL, Bendixen BH, Adams HP Jr, Clarke W, Kappelle LJ, Woolson RF. Interphysician agreement in the diagnosis of subtypes of acute ischemic stroke: implications for clinical trials. The TOAST Investigators. Neurology. 1993; 43:1021–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Diabetic Ketoacidosis Induced by Sodium-Glucose Cotransporter 2 Inhibitor
- Sodium-Glucose Cotransporter 2 Inhibitors for People with Type 1 Diabetes
- The Side Effects of Sodium Glucose Cotransporter 2 (SGLT2) Inhibitor
- The Non-glycemic Effects of SGLT2 Inhibitor
- Case of hyperosmolar hyperglycemic state by a sodium-glucose cotransporter 2 inhibitor