Arch Hand Microsurg.
2022 Jun;27(2):134-139. 10.12790/ahm.21.0152.
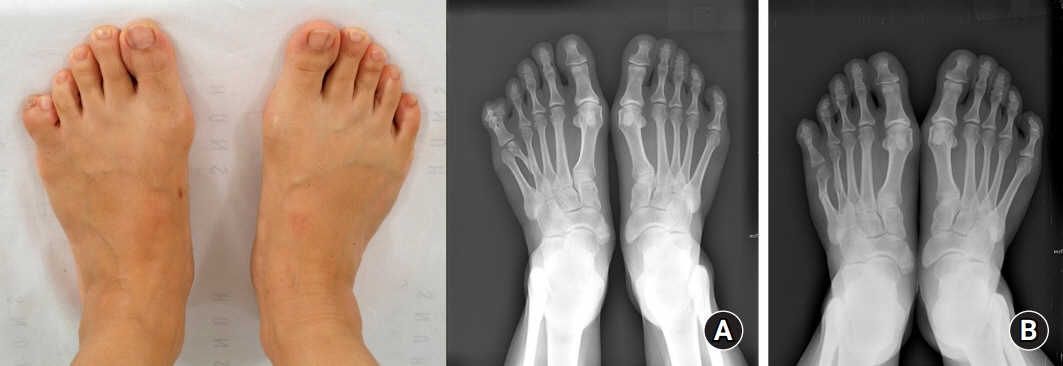
Surgical outcomes of untreated congenital polysyndactyly of the foot in adult patients
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2531919
- DOI: http://doi.org/10.12790/ahm.21.0152
Abstract
- Purpose
Polydactyly of the foot is a common congenital anomaly. The goal of surgery for polydactyly is to increase similarity to the contralateral foot, with a well-aligned arcade of toes that allows patients to wear normal footwear and ambulate painlessly. Foot appearance is especially important in Asian countries where people remove their shoes indoors. This study reviewed the surgical results in patients who underwent surgery for correction of untreated foot polydactyly after the age of 18 years.
Methods
We retrospectively analyzed the data of 11 patients who underwent surgery between 2006 and 2019. The forefoot width, angulation difference, and toe length ratios between the affected and unaffected feet were compared before and after the operation. In addition, the purpose of the surgery and postoperative cosmetic satisfaction were collected for each patient.
Results
The median age at the time of the operation was 25 years (interquartile range, 22–32 years) and most patients presented with postaxial polydactyly. The primary reasons to undergo surgery were both functional and cosmetic. The forefoot width and angle difference ratios became significantly more similar to the contralateral side postoperatively (p<0.05). No significant difference was found in the toe length ratio. Postoperative Global Aesthetic Improvement Scale scores showed satisfactory results.
Conclusion
The main reasons for surgery in adulthood included the diverse consequences of functional and cosmetic aspects of the anomaly. Surgery for patients with untreated polydactyly of the foot can yield satisfactory objective and subjective results regardless of the intervention timing.
Keyword
Figure
Reference
-
References
1. Kelly DM, Mahmoud K, Mauck BM. Polydactyly of the foot: a review. J Am Acad Orthop Surg. 2021; 29:361–9.
Article2. Cetik O, Uslu M, Cirpar M, Eksioglu F. Experience with the surgical treatment of radial polydactyly in adults. Ann Plast Surg. 2005; 55:363–6.
Article3. Light T, Buck-Gramcko D. Polydactyly: terminology and classification. In : Buck-Gramcko D, editor. Congenital malformations of the hand and forearm. London: Churchill Livingstone;1998. p. 217–24.4. Dobyns JH, Wood VE, Bayne LG, et al. Congenital hand deformities. In : Green DP, editor. Operative hand surgery, Vol. 2. 2nd ed. New York: Churchill Livingstone;1988. p. 255–536.5. Kim JH, Kim BJ, Kwon ST. Foot syndactyly: a clinical and demographic analysis. Arch Plast Surg. 2016; 43:559–63.
Article6. Venn-Watson EA. Problems in polydactyly of the foot. Orthop Clin North Am. 1976; 7:909–27.
Article7. Cowan RJ. Surgical problems associated with congenital malformations of the forefoot. Can J Surg. 1965; 8:29–41.8. Seok HH, Park JU, Kwon ST. New classification of polydactyly of the foot on the basis of syndactylism, axis deviation, and metatarsal extent of extra digit. Arch Plast Surg. 2013; 40:232–7.
Article9. Woo SJ, Kim BJ, Kwon ST. Case-control study of the treatment of postaxial polysyndactyly of the foot: comparison of surgical results after removal of the fifth or sixth toe. Arch Plast Surg. 2021; 48:91–7.
Article10. Narins RS, Brandt F, Leyden J, Lorenc ZP, Rubin M, Smith S. A randomized, double-blind, multicenter comparison of the efficacy and tolerability of Restylane versus Zyplast for the correction of nasolabial folds. Dermatol Surg. 2003; 29:588–95.
Article11. Uda H, Sugawara Y, Niu A, Sarukawa S. Treatment of lateral ray polydactyly of the foot: focusing on the selection of the toe to be excised. Plast Reconstr Surg. 2002; 109:1581–91.
Article12. Chan CW, Rudins A. Foot biomechanics during walking and running. Mayo Clin Proc. 1994; 69:448–61.
Article13. Johnson SP, Sebastin SJ, Rehim SA, Chung KC. The importance of hand appearance as a patient-reported outcome in hand surgery. Plast Reconstr Surg Glob Open. 2015; 3:e552.
Article14. McDougall L, Kennedy J, Coombs C, Penington A. The psychosocial impact of congenital hand and upper limb differences on children: a qualitative study. J Hand Surg Eur Vol. 2021; 46:391–7.
Article15. Andersson GB, Gillberg C, Fernell E, Johansson M, Nachemson A. Children with surgically corrected hand deformities and upper limb deficiencies: self-concept and psychological well-being. J Hand Surg Eur Vol. 2011; 36:795–801.
Article16. Hughes MJ. The social consequences of facial disfigurement. Milton: Routledge;2019.17. Franzblau LE, Chung KC, Carlozzi N, Chin AY, Nellans KW, Waljee JF. Coping with congenital hand differences. Plast Reconstr Surg. 2015; 135:1067–75.
Article18. Rumsey N, Harcourt D. Body image and disfigurement: issues and interventions. Body Image. 2004; 1:83–97.
Article19. Bradbury E. Psychological issues for children and their parents. In : Buck-Gramcko D, editor. Congenital malformations of the hand and forearm. London: Churchill Livingstone;1998. p. 48–56.20. Eskandari MM, Oztuna V, Demirkan F. Late psychosocial effects of congenital hand anomaly. Hand Surg. 2004; 9:257–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Axial Polysyndactyly and Postaxial Polydactyly of The Hand in Korean: A Clinical Analysis of 24 Cases
- Analysis of Congenital Postaxial Polydactyly of the Foot Using Magnetic Resonance Imagings
- Case-control study of the treatment of postaxial polysyndactyly of the foot: Comparison of surgical results after removal of the fifth or sixth toe
- Nationwide Estimation for Incidence at Birth of Congenital Polydactyly and Syndactyly in Korean
- Treatment of Congenital toe Anomalies