J Korean Neurosurg Soc.
2022 Jul;65(4):539-548. 10.3340/jkns.2021.0168.
Full-Endoscopic versus Minimally Invasive Lumbar Interbody Fusion for Lumbar Degenerative Diseases : A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Neurosurgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- KMID: 2531623
- DOI: http://doi.org/10.3340/jkns.2021.0168
Abstract
Objective
: Although full-endoscopic lumbar interbody fusion (Endo-LIF) has been tried as the latest alternative technique to minimally invasive transforaminal lumbar interobody fusion (MIS-TLIF) since mid-2010, the evidence is still lacking. We compared the clinical outcome and safety of Endo-LIF to MIS-TLIF for lumbar degenerative disease.
Methods
: We systematically searched electronic databases, including PubMed, EMBASE, and Cochrane Library to find literature comparing Endo-LIF to MIS-TLIF. The results retrieved were last updated on December 11, 2020. The perioperative outcome included the operation time, blood loss, complication, and hospital stay. The clinical outcomes included Visual analog scale (VAS) of low back pain and leg pain and Oswestry disability index (ODI), and the radiological outcome included pseudoarthosis rate with 12-month minimum follow-up.
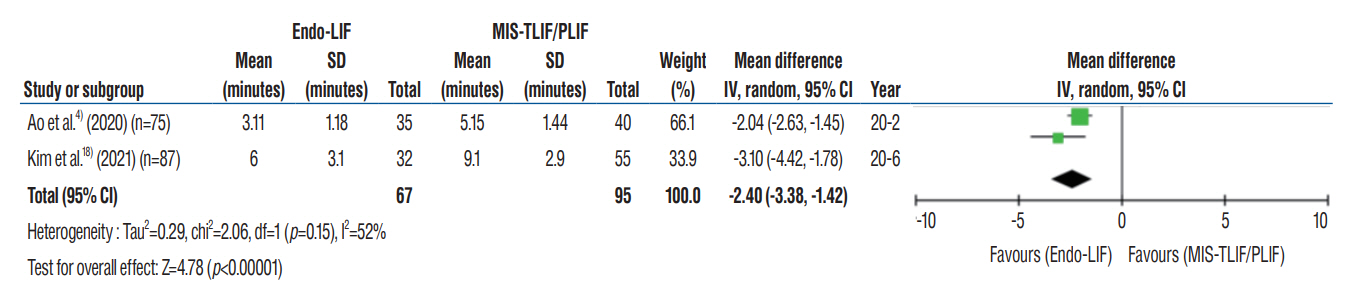
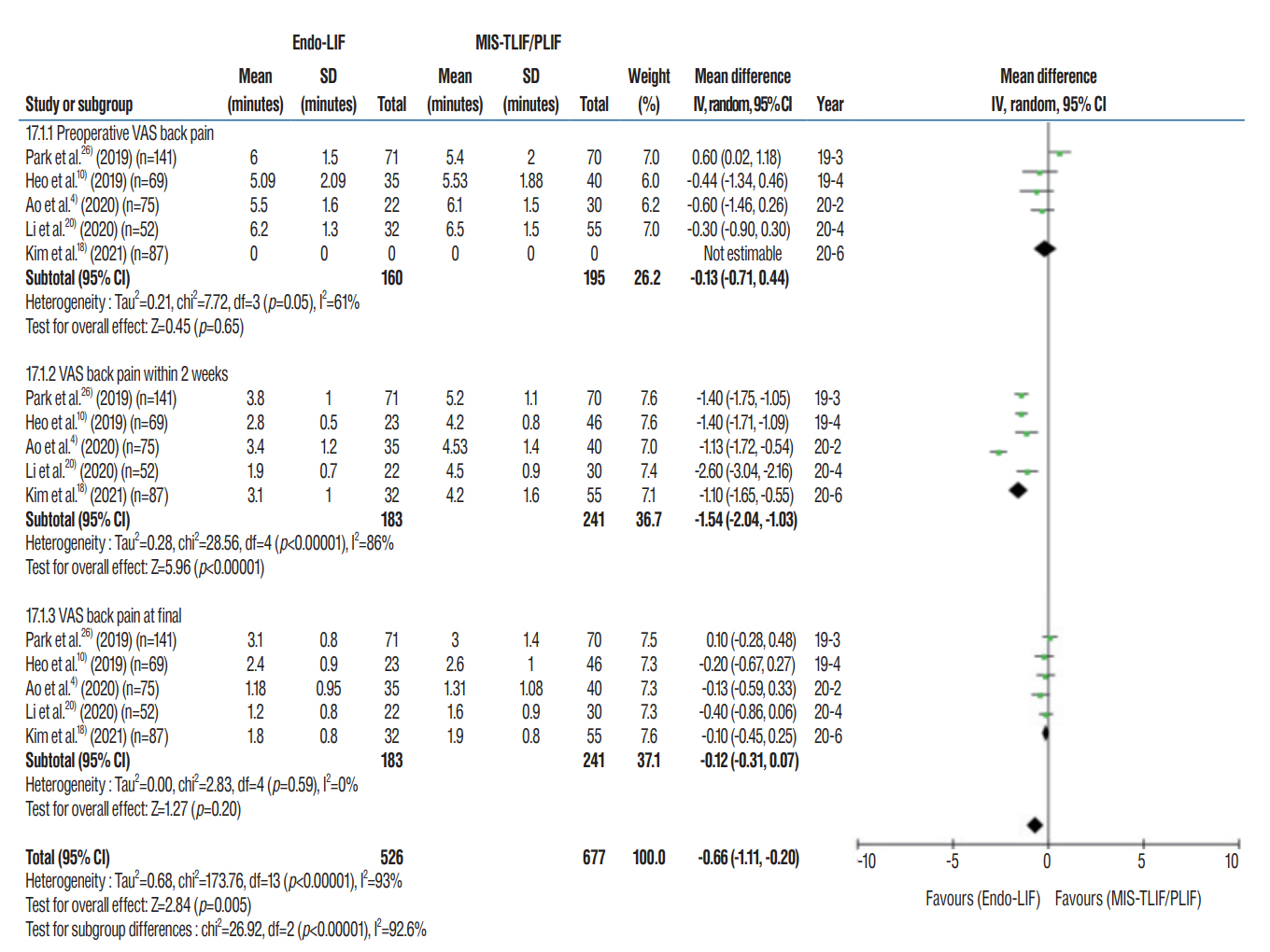
Results
: Four retrospective observational studies and one prospective observational study comprising 423 patients (183 Endo-LIF and 241 MIS-TLIF) were included, and the pooled data analysis revealed low heterogeneity between studies in our review. Baseline characteristics including age and sex were not different between the two groups. Operation time was significantly longer in Endo- LIF (mean difference [MD], 23.220 minutes; 95% confidence interval [CI], 10.669–35.771; p=0.001). However, Endo-LIF resulted in less perioperative blood loss (MD, -144.710 mL; 95% CI, 247.941–41.478; p=0.023). Although VAS back pain at final (MD, -0.120; p=0.586), leg pain within 2 weeks (MD, 0.005; p=0.293), VAS leg pain at final (MD, 0.099; p=0.099), ODI at final (MD, 0.141; p=0.093) were not different, VAS back pain within 2 weeks was more favorable in the Endo-LIF (MD, -1.538; 95% CI, -2.044 to -1.032; p<0.001). On the other hand, no statistically significant group difference in complication rate (relative risk [RR], 0.709; p=0.774), hospital stay (MD, -2.399; p=0.151), and pseudoarthrosis rate (RR, 1.284; p=0.736) were found.
Conclusion
: Relative to MIS-TLIF, immediate outcomes were favorable in Endo-LIF in terms of blood loss and immediate VAS back pain, although complication rate, mid-term clinical outcomes, and fusion rate were not different. However, the challenges for Endo-LIF include longer operation time which means a difficult learning curve and limited surgical indication which means patient selection bias. Larger-scale, well-designed study with long-term follow-up and randomized controlled trials are needed to confirm and update the results of this systematic review.
Keyword
Figure
Reference
-
References
1. Ahn Y. A historical review of endoscopic spinal discectomy. World Neurosurg. 145:591–596. 2021.
Article2. Ahn Y, Lee S, Son S, Kim H, Kim JE. Learning curve for transforaminal percutaneous endoscopic lumbar discectomy: a systematic review. World Neurosurg. 143:471–479. 2020.
Article3. Ahn Y, Youn MS, Heo DH. Endoscopic transforaminal lumbar interbody fusion: a comprehensive review. Expert Rev Med Devices. 16:373–380. 2019.
Article4. Ao S, Zheng W, Wu J, Tang Y, Zhang C, Zhou Y, et al. Comparison of preliminary clinical outcomes between percutaneous endoscopic and minimally invasive transforaminal lumbar interbody fusion for lumbar degenerative diseases in a tertiary hospital: is percutaneous endoscopic procedure superior to MIS-TLIF? A prospective cohort study. Int J Surg. 76:136–143. 2020.
Article5. Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg. 49:499–517. 2002.6. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 64:383–394. 2011.
Article7. Harms J, Rolinger H. A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author's transl). Z Orthop Ihre Grenzgeb. 120:343–347. 1982.8. Hayashino Y, Noguchi Y, Fukui T. Systematic evaluation and comparison of statistical tests for publication bias. J Epidemiol. 15:235–243. 2005.
Article9. Heo DH, Lee DC, Kim HS, Park CK, Chung H. Clinical results and complications of endoscopic lumbar interbody fusion for lumbar degenerative disease: a meta-analysis. World Neurosurg. 145:396–404. 2021.
Article10. Heo DH, Park CK. Clinical results of percutaneous biportal endoscopic lumbar interbody fusion with application of enhanced recovery after surgery. Neurosurg Focus. 46:E18. 2019.
Article11. Heo DH, Son SK, Eum JH, Park CK. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus. 43:E8. 2017.
Article12. Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane Handbook for Systematic Reviews of Interventions. Version 6. Available at : https://training.cochrane.org/handbook/archive/v6.13. Jin M, Zhang J, Shao H, Liu J, Huang Y. Percutaneous transforaminal endoscopic lumbar interbody fusion for degenerative lumbar diseases: a consecutive case series with mean 2-year follow-up. Pain Physician. 23:165–174. 2020.14. Kamson S, Lu D, Sampson PD, Zhang Y. Full-endoscopic lumbar fusion outcomes in patients with minimal deformities: a retrospective study of data collected between 2011 and 2015. Pain Physician. 22:75–88. 2019.15. Karikari IO, Isaacs RE. Minimally invasive transforaminal lumbar interbody fusion: a review of techniques and outcomes. Spine (Phila Pa 1976). 35(26 Suppl):S294–S301. 2010.16. Kim HS, Wu PH, Lee YJ, Kim DH, Jang IT. Technical considerations of uniportal endoscopic posterolateral lumbar interbody fusion: a review of its early clinical results in application in adult degenerative scoliosis. World Neurosurg. 145:682–692. 2021.
Article17. Kim JE, Choi DJ. Biportal endoscopic transforaminal lumbar interbody fusion with arthroscopy. Clin Orthop Surg. 10:248–252. 2018.
Article18. Kim JE, Yoo HS, Choi DJ, Park EJ, Jee SM. Comparison of minimal invasive versus biportal endoscopic transforaminal lumbar interbody fusion for single-level lumbar disease. Clin Spine Surg. 34:E64–E71. 2021.
Article19. Kolcun JPG, Brusko GD, Basil GW, Epstein R, Wang MY. Endoscopic transforaminal lumbar interbody fusion without general anesthesia: operative and clinical outcomes in 100 consecutive patients with a minimum 1-year follow-up. Neurosurg Focus. 46:E14. 2019.
Article20. Li Y, Dai Y, Wang B, Li L, Li P, Xu J, et al. Full-endoscopic posterior lumbar interbody fusion via an interlaminar approach versus minimally invasive transforaminal lumbar interbody fusion: a preliminary retrospective study. World Neurosurg. 144:e475–e482. 2020.
Article21. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 151:W65–W94. 2009.
Article22. Lin PM. A technical modification of Cloward's posterior lumbar interbody fusion. Neurosurgery. 1:118–124. 1977.
Article23. Miller LE, Bhattacharyya S, Pracyk J. Minimally invasive versus open transforaminal lumbar interbody fusion for single-level degenerative disease: a systematic review and meta-analysis of randomized controlled trials. World Neurosurg. 133:358–365.e4. 2020.
Article24. Nagahama K, Ito M, Abe Y, Murota E, Hiratsuka S, Takahata M. Early clinical results of percutaneous endoscopic transforaminal lumbar interbody fusion: a new modified technique for treating degenerative lumbar spondylolisthesis. Spine Surg Relat Res. 3:327–334. 2018.
Article25. Nakamura S, Taguchi M. Full percutaneous lumbar interbody fusion: technical note. J Neurol Surg A Cent Eur Neurosurg. 78:601–606. 2017.
Article26. Park MK, Park SA, Son SK, Park WW, Choi SH. Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev. 42:753–761. 2019.
Article27. Resnick DK, Choudhri TF, Dailey AT, Groff MW, Khoo L, Matz PG, et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 1: introduction and methodology. J Neurosurg Spine. 2:637–638. 2005.
Article28. Resnick DK, Choudhri TF, Dailey AT, Groff MW, Khoo L, Matz PG, et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 11: interbody techniques for lumbar fusion. J Neurosurg Spine. 2:692–699. 2005.
Article29. Son S, Ahn Y, Lee SG, Kim WK. Learning curve of percutaneous endoscopic interlaminar lumbar discectomy versus open lumbar microdiscectomy at the L5-S1 level. PLoS One. 15:e0236296. 2020.
Article30. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 25:603–605. 2010.
Article31. Wagner R, Haefner M. Uniportal endoscopic lumbar interbody fusion. Neurospine. 17(Suppl 1):S120–S128. 2020.
Article32. Wu J, Liu H, Ao S, Zheng W, Li C, Li H, et al. Percutaneous endoscopic lumbar interbody fusion: technical note and preliminary clinical experience with 2-year follow-up. Biomed Res Int. 2018:5806037. 2018.
Article33. Wu PH, Kim HS, Jang IT. A narrative review of development of full-endoscopic lumbar spine surgery. Neurospine. 17(Suppl 1):S20–S33. 2020.
Article34. Wu PH, Kim HS, Lee YJ, Kim DH, Lee JH, Jeon JB, et al. Uniportal full endoscopic posterolateral transforaminal lumbar interbody fusion with endoscopic disc drilling preparation technique for symptomatic foraminal stenosis secondary to severe collapsed disc space: a clinical and computer tomographic study with technical note. Brain Sci. 10:373. 2020.
Article35. Wu W, Yang S, Diao W, Wang D, Guo Y, Yan M, et al. Analysis of clinical efficacy of endo-LIF in the treatment of single-segment lumbar degenerative diseases. J Clin Neurosci. 71:51–57. 2020.
Article36. Yang J, Liu C, Hai Y, Yin P, Zhou L, Zhang Y, et al. Percutaneous endoscopic transforaminal lumbar interbody fusion for the treatment of lumbar spinal stenosis: preliminary report of seven cases with 12-month follow-up. Biomed Res Int. 2019:3091459. 2019.
Article37. Youn MS, Shin JK, Goh TS, Lee JS. Full endoscopic lumbar interbody fusion (FELIF): technical note. Eur Spine J. 27:1949–1955. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum to “Full-Endoscopic versus Minimally Invasive Lumbar Interbody Fusion for Lumbar Degenerative Diseases : A Systematic Review and Meta-Analysis” by Son et al. (J Korean Neurosurg Soc 65 : 539-548, 2022)
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Minimally Invasive Strategy for Uniportal Full-Endoscopic Transforaminal Lumbar Interbody Fusion Using a Large Cage Utilized in Oblique Lumbar Interbody Fusion
- Biportal Endoscopic Transforaminal Interbody Fusion for Lumbar Adjacent Segment Disease: An Illustrative Case and Literature Review
- A Review of Fully Endoscopic Lumbar Interbody Fusion