Cancer Res Treat.
2022 Jul;54(3):709-718. 10.4143/crt.2021.834.
Effect of National Oral Health Screening Program on the Risk of Head and Neck Cancer: A Korean National Population-Based Study
- Affiliations
-
- 1Department of Radiation Oncology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 2Section of Dentistry Medicine, Department of Periodontology, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Family Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 5Department of Radiation Oncology, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2531317
- DOI: http://doi.org/10.4143/crt.2021.834
Abstract
- Purpose
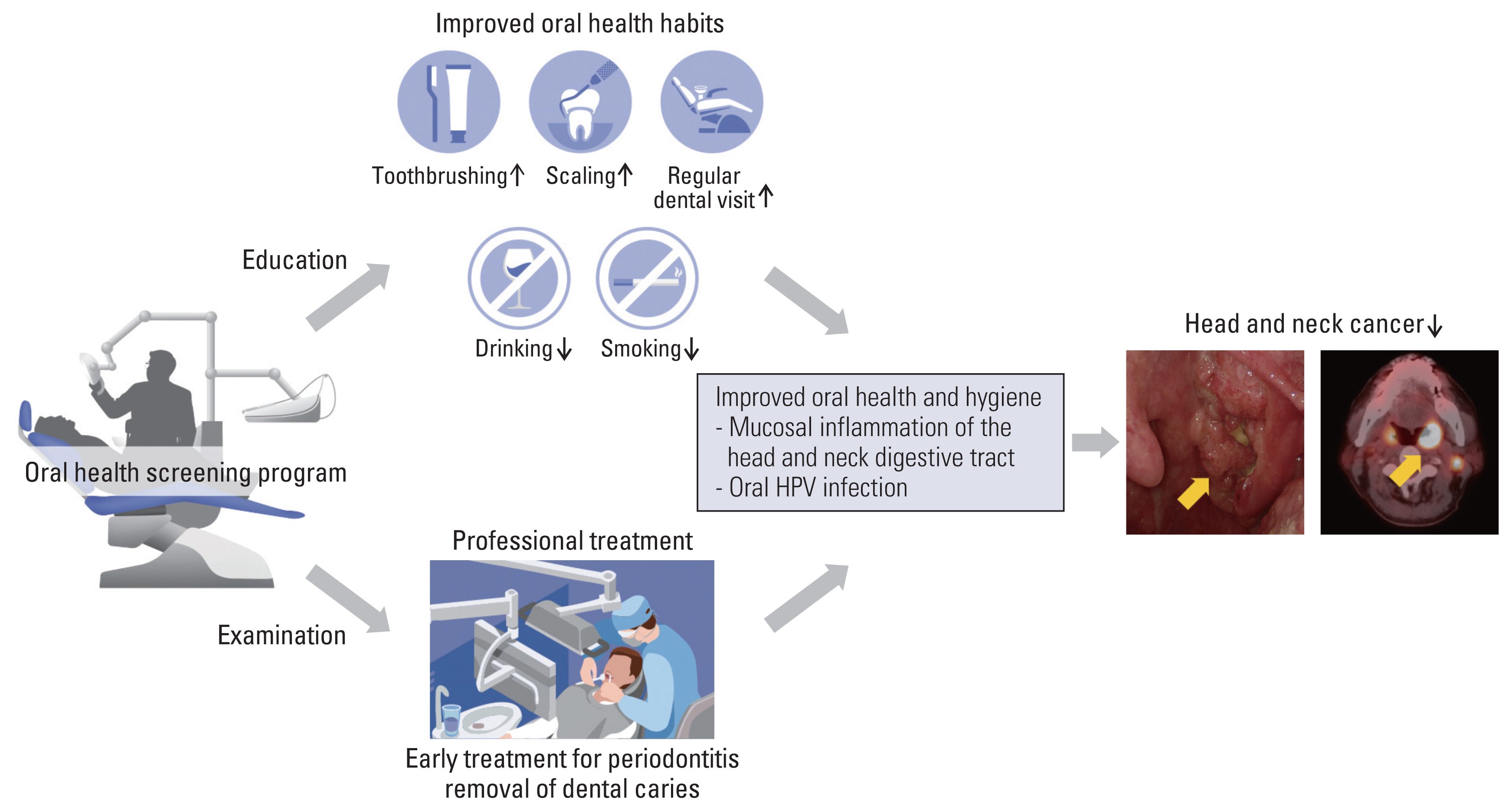
Poor oral health is associated with head and neck cancer (HNC). We evaluated whether a national oral health screening program (OHSP) could reduce the risk of HNC.
Materials and Methods
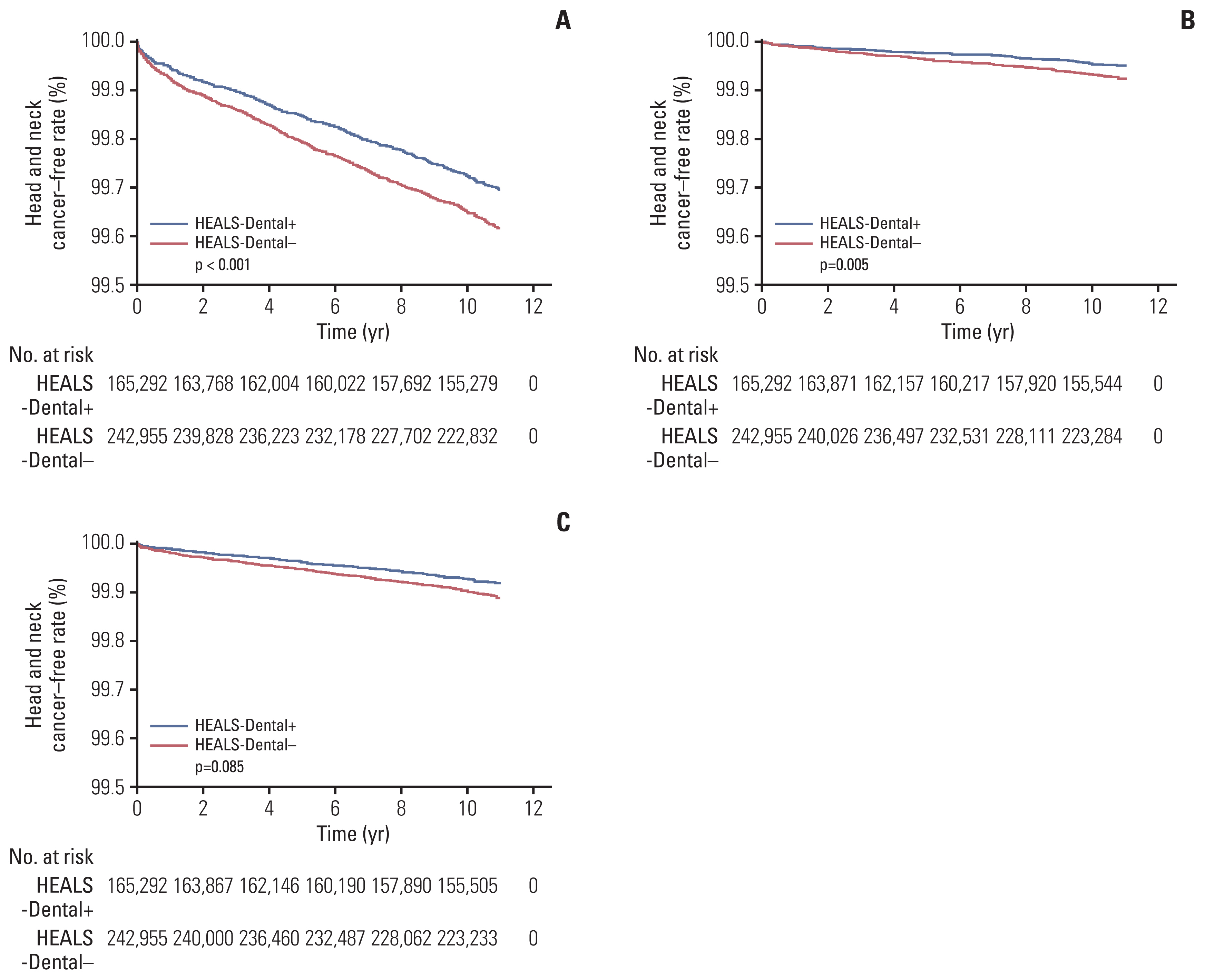
Data from 408,247 healthy individuals aged ≥ 40 years from the National Health Insurance System-National Health Screening program during 2003 and 2004 in Korea were analyzed. The risk of HNC was compared between subjects who underwent OHSP (HEALS-Dental+, n=165,292) and routine health check-ups only (HEALS-Dental‒, n=242,955). The impact of individual oral health-related factors on HNC risk was evaluated in HEALS-Dental+.
Results
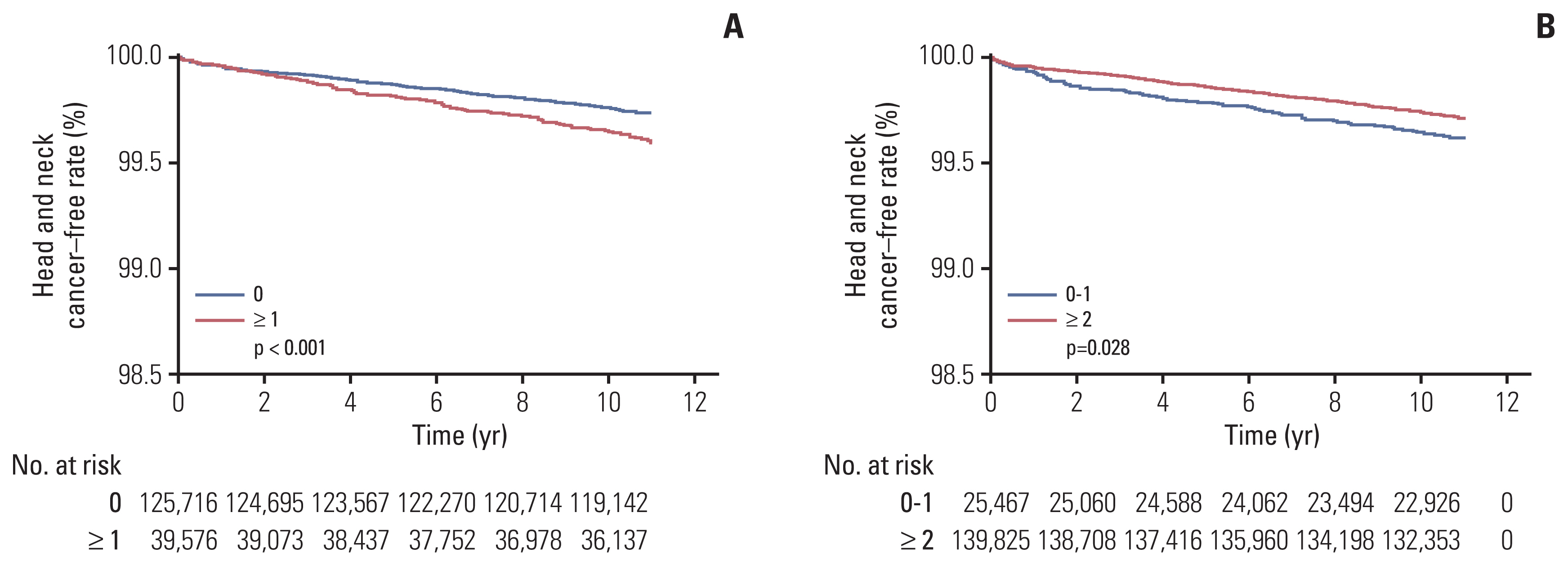
A total of 1,650 HNC cases were diagnosed. The 10-year HNC-free rate was 99.684% with a median follow-up of 11 years. The risk of all HNC (hazard ratio [HR], 1.16; 95% confidence interval [CI], 1.03 to 1.29; p=0.011) and oropharyngeal cancer (HR, 1.48; 95% CI, 1.13 to 1.94; p=0.005) was significantly higher in HEALS-Dental‒ than in HEALS-Dental+. In HEALS-Dental+, oral cavity cancer was marginally reduced (p=0.085), and missing teeth was a significant factor for HNC (HR, 1.24; 95% CI, 1.02 to 1.50; p=0.032). Toothbrushing was a significant factor in univariate analysis (p=0.028), but not in multivariate analysis (p=0.877).
Conclusion
The National OHSP significantly reduced the long-term HNC risk, particularly the incidence of oropharyngeal cancer. Routine OHSP should be considered at the population level.
Keyword
Figure
Reference
-
References
1. Hong S, Won YJ, Lee JJ, Jung KW, Kong HJ, Im JS, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2018. Cancer Res Treat. 2021; 53:301–15.
Article2. Bundgaard T, Wildt J, Frydenberg M, Elbrond O, Nielsen JE. Case-control study of squamous cell cancer of the oral cavity in Denmark. Cancer Causes Control. 1995; 6:57–67.
Article3. Lewin F, Norell SE, Johansson H, Gustavsson P, Wennerberg J, Biorklund A, et al. Smoking tobacco, oral snuff, and alcohol in the etiology of squamous cell carcinoma of the head and neck: a population-based case-referent study in Sweden. Cancer. 1998; 82:1367–75.
Article4. D’Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, et al. Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007; 356:1944–56.
Article5. Marshall JR, Graham S, Haughey BP, Shedd D, O’Shea R, Brasure J, et al. Smoking, alcohol, dentition and diet in the epidemiology of oral cancer. Eur J Cancer B Oral Oncol. 1992; 28B:9–15.
Article6. Rosenquist K, Wennerberg J, Schildt EB, Bladstrom A, Goran Hansson B, Andersson G. Oral status, oral infections and some lifestyle factors as risk factors for oral and oropharyngeal squamous cell carcinoma: a population-based case-control study in southern Sweden. Acta Otolaryngol. 2005; 125:1327–36.
Article7. Chang JS, Lo HI, Wong TY, Huang CC, Lee WT, Tsai ST, et al. Investigating the association between oral hygiene and head and neck cancer. Oral Oncol. 2013; 49:1010–7.
Article8. Hashim D, Sartori S, Brennan P, Curado MP, Wunsch-Filho V, Divaris K, et al. The role of oral hygiene in head and neck cancer: results from International Head and Neck Cancer Epidemiology (INHANCE) consortium. Ann Oncol. 2016; 27:1619–25.
Article9. Corbella S, Veronesi P, Galimberti V, Weinstein R, Del Fabbro M, Francetti L. Is periodontitis a risk indicator for cancer? A meta-analysis. PLoS One. 2018; 13:e0195683.
Article10. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7:e016640.
Article11. Cao X, Xu J. Insights into inflammasome and its research advances in cancer. Tumori. 2019; 105:456–64.
Article12. Heikkila P, But A, Sorsa T, Haukka J. Periodontitis and cancer mortality: register-based cohort study of 68,273 adults in 10-year follow-up. Int J Cancer. 2018; 142:2244–53.
Article13. Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011; 29:4294–301.
Article14. Kim SH, Koo BS, Kang S, Park K, Kim H, Lee KR, et al. HPV integration begins in the tonsillar crypt and leads to the alteration of p16, EGFR and c-myc during tumor formation. Int J Cancer. 2007; 120:1418–25.
Article15. Kim Y, Joo YH, Kim MS, Lee YS. Prevalence of high-risk human papillomavirus and its genotype distribution in head and neck squamous cell carcinomas. J Pathol Transl Med. 2020; 54:411–8.
Article16. Choi I, Lee D, Son KB, Bae S. Incidence, cost and gender differences of oropharyngeal and noncervical anogenital cancers in South Korea. BMC Public Health. 2020; 20:1035.
Article17. Tezal M, Sullivan Nasca M, Stoler DL, Melendy T, Hyland A, Smaldino PJ, et al. Chronic periodontitis-human papilloma-virus synergy in base of tongue cancers. Arch Otolaryngol Head Neck Surg. 2009; 135:391–6.
Article18. Wiener RC, Sambamoorthi U, Jurevic RJ. Association of periodontitis and human papillomavirus in oral rinse specimens: results from the National Health and Nutrition Survey 2009–2012. J Am Dent Assoc. 2015; 146:382–9.19. Sun CX, Bennett N, Tran P, Tang KD, Lim Y, Frazer I, et al. A pilot study into the association between oral health status and human papillomavirus-16 infection. Diagnostics (Basel). 2017; 7:11.
Article20. Mazul AL, Taylor JM, Divaris K, Weissler MC, Brennan P, Anantharaman D, et al. Oral health and human papilloma-virus-associated head and neck squamous cell carcinoma. Cancer. 2017; 123:71–80.
Article21. Lee K, Lee JS, Kim J, Lee H, Chang Y, Woo HG, et al. Oral health and gastrointestinal cancer: a nationwide cohort study. J Clin Periodontol. 2020; 47:796–808.
Article22. Park SY, Kim SH, Kang SH, Yoon CH, Lee HJ, Yun PY, et al. Improved oral hygiene care attenuates the cardiovascular risk of oral health disease: a population-based study from Korea. Eur Heart J. 2019; 40:1138–45.
Article23. Chang Y, Lee JS, Lee KJ, Woo HG, Song TJ. Improved oral hygiene is associated with decreased risk of new-onset diabetes: a nationwide population-based cohort study. Diabetologia. 2020; 63:924–33.
Article24. Chang Y, Woo HG, Park J, Lee JS, Song TJ. Improved oral hygiene care is associated with decreased risk of occurrence for atrial fibrillation and heart failure: a nationwide population-based cohort study. Eur J Prev Cardiol. 2020; 27:1835–45.
Article