Anat Cell Biol.
2022 Jun;55(2):247-250. 10.5115/acb.22.004.
Three ipsilateral paracondylar processes with other skull base variations: case report
- Affiliations
-
- 1Department of Neurosurgery, Tulane University School of Medicine, New Orleans, LA, USA
- 2Department of Anatomical Dissection and Donation, Chair of Anatomy and Histology, Medical University of Lodz, Lodz, Poland
- 3Department of Orthopedics and Traumatology, University Hospital Queen Giovanna-ISUL, Medical University of Sofia, Sofia, Bulgaria
- 4Department of Neurology, Tulane University School of Medicine, New Orleans, LA, USA
- 5Department of Anatomical Sciences, St. George’s University, St. George’s, Grenada
- 6University of Queensland, Brisbane, Australia
- 7Department of Structural and Cellular Biology, Tulane University School of Medicine, New Orleans, LA, USA
- 8Department of Neurosurgery and Ochsner Neuroscience Institute, Ochsner Health System, New Orleans, LA, USA
- KMID: 2531211
- DOI: http://doi.org/10.5115/acb.22.004
Abstract
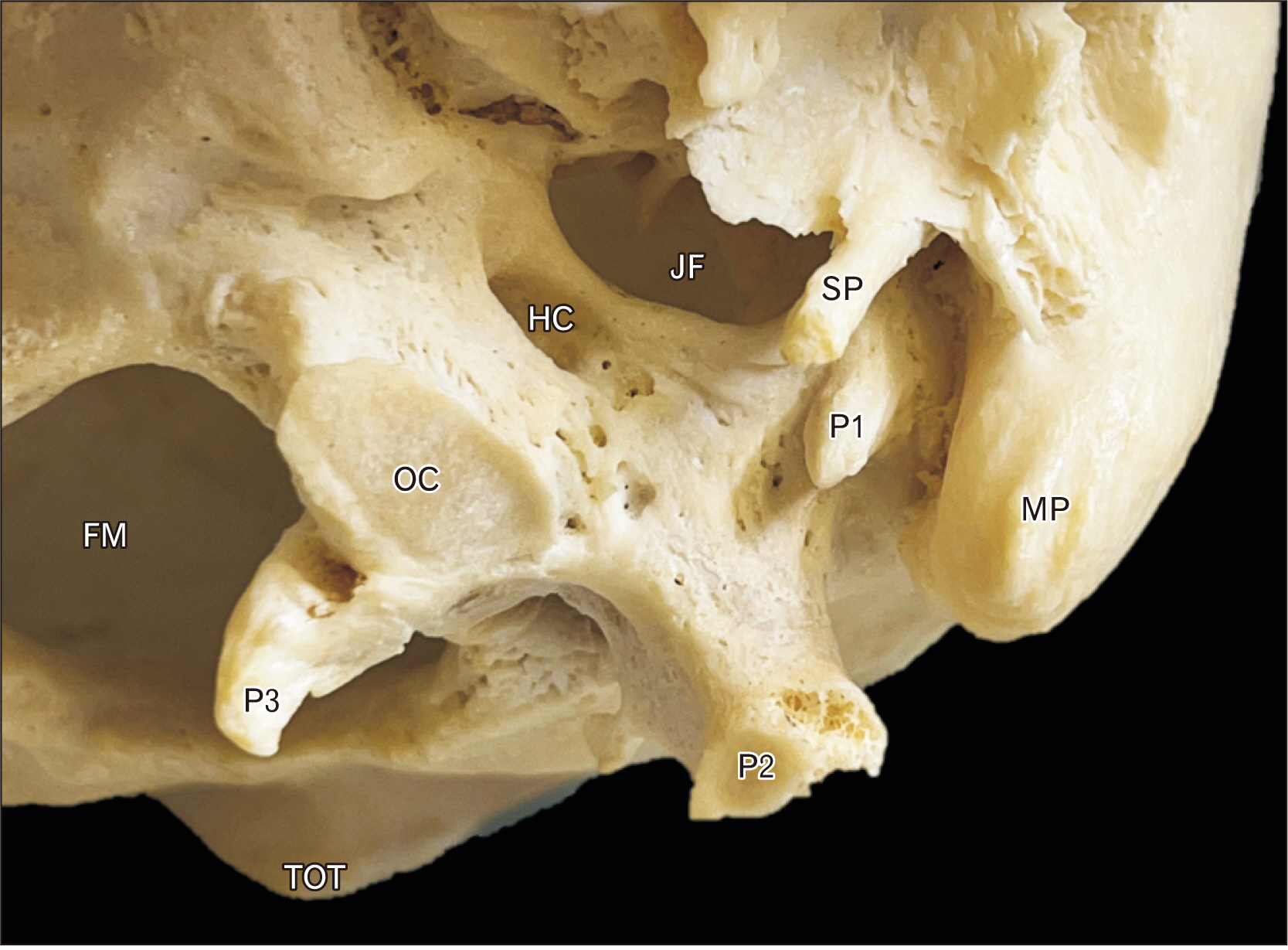
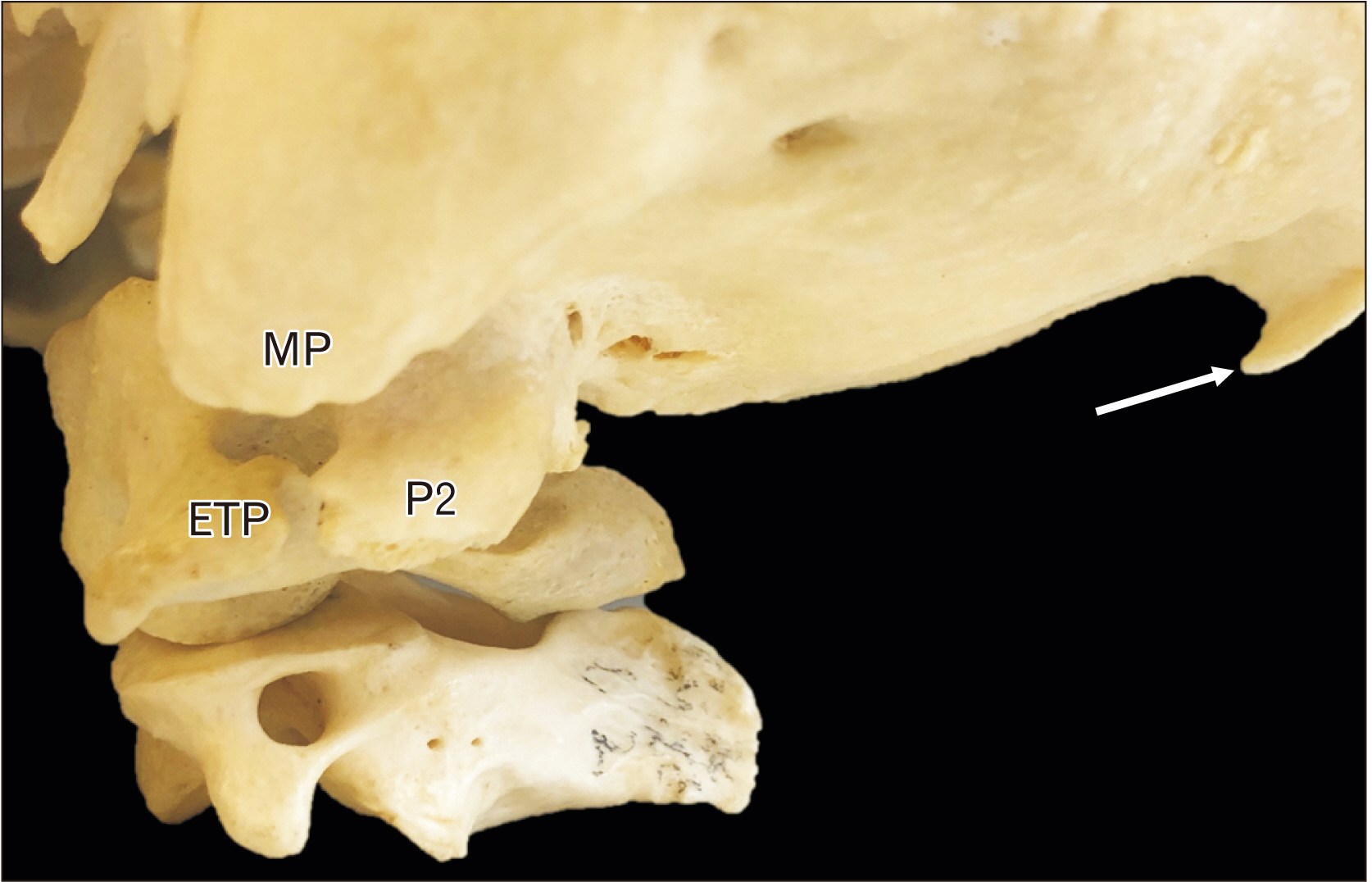
- Variations of the skull base can affect surgical approaches and must be considered when viewing and interpreting radiological imaging. Here, we report a unique collection of bony anatomical variations found on a single adult skull. Three bony excrescences from the occipital bone were identified in the paracondylar region. The smallest of these processes was 7 mm long and was just medial to the mastoid process of the temporal bone and posterior to the styloid process. One bony process was attached to the occipital condyle and was 12 mm in length. The longest of these processes was 17 mm long and arose from the jugular process of the occipital bone. Paracondylar processes can be symptomatic. Knowledge of the bony variations at the skull base is important to those who operate in this region or review and interpret radiological imaging.
Keyword
Figure
Reference
-
References
1. Nolet PS, Friedman L, Brubaker D. 1999; Paracondylar process: a rare cause of craniovertebral fusion - a case report. J Can Chiropr Assoc. 43:229–35.2. Schumacher M, Yilmaz E, Iwanaga J, Oskouian R, Tubbs RS. 2018; Paramastoid process: literature review of its anatomy and clinical implications. World Neurosurg. 117:261–3. DOI: 10.1016/j.wneu.2018.06.056. PMID: 29929028.
Article3. McCall T, Coppens J, Couldwell W, Dailey A. 2010; Symptomatic occipitocervical paracondylar process. J Neurosurg Spine. 12:9–12. DOI: 10.3171/2009.7.SPINE09345. PMID: 20043756.
Article4. Keskil S, Gözil R, Calgüner E. 2003; Common surgical pitfalls in the skull. Surg Neurol. 59:228–31. discussion 231DOI: 10.1016/S0090-3019(02)01038-8. PMID: 12681561.
Article5. Hauser G, De Stefano GF. 1989. Epigenetic variants of the human skull. Schweizerbart;Stuttgart:6. Iwanaga J, Singh V, Ohtsuka A, Hwang Y, Kim HJ, Moryś J, Ravi KS, Ribatti D, Trainor PA, Sañudo JR, Apaydin N, Şengül G, Albertine KH, Walocha JA, Loukas M, Duparc F, Paulsen F, Del Sol M, Adds P, Hegazy A, Tubbs RS. 2021; Acknowledging the use of human cadaveric tissues in research papers: recommendations from anatomical journal editors. Clin Anat. 34:2–4. DOI: 10.1002/ca.23671. PMID: 32808702.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Iatrogenic Skull Base Defect Accompanied by Brain Injury After Endoscopic Sinus Surgery: A Report of Two Cases
- Solitary Plasmacytoma of the Skull Base: Case Report
- Cervicogenic Headache from Skull Base Osteomyelitis : A case report
- Two Cases of Skull Base Osteomyelitis after Mastoidectomy
- A Case of Extracranial Chondroma of the Skull Base