Korean J Transplant.
2022 Jun;36(2):136-142. 10.4285/kjt.22.0004.
The outcomes of marginal donor hearts compared with ideal donors: a single-center experience in Iran
- Affiliations
-
- 1Department of Cardiovascular Surgery, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran
- 2Organ Procurement Unit, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran
- 3Iranian Tissue Bank and Research Center, Tehran University of Medical Sciences, Tehran, Iran
- 4Cardiac Primary Prevention Research Center (CPPRC), Cardiovascular Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran
- 5Department of Cardiology, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran
- 6Department of Cardiology, Ziaeian Hospital, School of Medicine, International Campus, Tehran University of Medical Sciences, Tehran, Iran
- KMID: 2531137
- DOI: http://doi.org/10.4285/kjt.22.0004
Abstract
- Background
Heart transplantation has been considered the gold-standard treatment for patients with end-stage heart failure. This study assessed the survival outcomes of marginal donor hearts compared with ideal donor hearts in Iran.
Methods
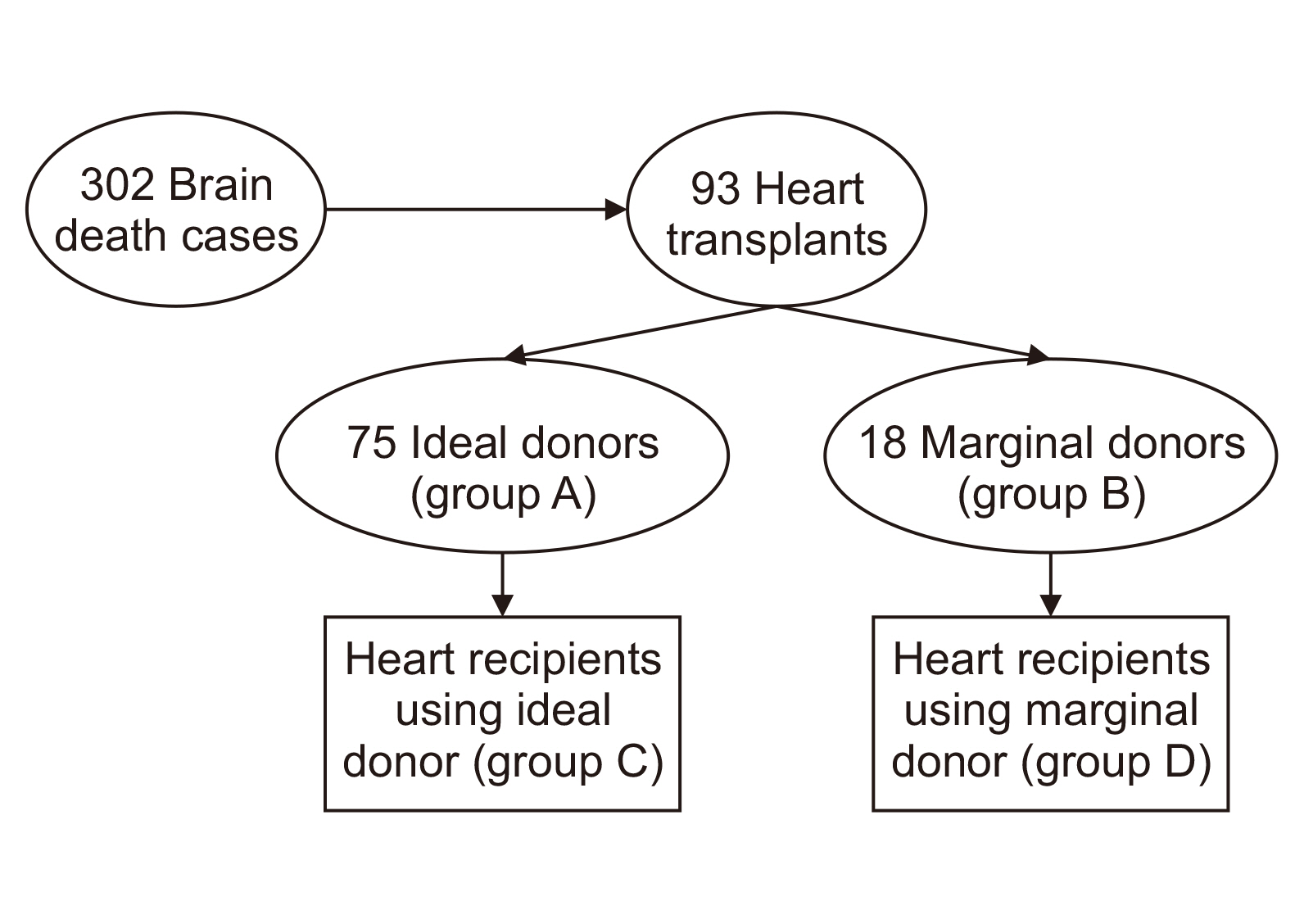
This retrospective study is based on the follow-up data of heart donors and recipients in the Sina Hospital Organ Procurement Unit. Among the 93 participants, 75 were categorized as ideal donors (group A) and 18 as marginal donors (group B). Group C included heart recipients who received a standard organ, and group D included heart recipients who received a marginal one. To analyze differences in patient character-istics among the groups, posttransplant heart survival was assessed in all groups. All data were obtained from the hospital records.
Results
The mean age of the donors was 26.27±11.44 years (median age, 28 years). The marginal age showed a significant association with donor age. The age of recipients had a significant effect on survival days in the ideal group. Most patients survived for at least 1 year, with a median of 645 days in recipients from marginal donors and 689 days in re-cipients from ideal donors.
Conclusions
Considering the lack of organ availability in Iran, it may be possible to use marginal donors for marginal recipients, therefore reducing the number of people on the waitlist. We also recommend establishing a national marginal donor system specifically for Iranian patients to extend the donor pool.
Figure
Reference
-
1. Kilic A, Emani S, Sai-Sudhakar CB, Higgins RS, Whitson BA. 2014; Donor selection in heart transplantation. J Thorac Dis. 6:1097–104. DOI: 10.3978/j.issn.2072-1439.2014.03.23. PMID: 25132976. PMCID: PMC4133543.2. Grady KL, Jalowiec A, White-Williams C. 1999; Predictors of quality of life in patients at one year after heart transplantation. J Heart Lung Transplant. 18:202–10. DOI: 10.1016/S1053-2498(98)00048-5. PMID: 10328145.3. Grady KL, Naftel DC, White-Williams C, Bellg AJ, Young JB, Pelegrin D, et al. 2005; Predictors of quality of life at 5 to 6 years after heart transplantation. J Heart Lung Transplant. 24:1431–9. DOI: 10.1016/j.healun.2004.08.012. PMID: 16143267.4. Lund LH, Edwards LB, Kucheryavaya AY, Benden C, Christie JD, Dipchand AI, et al. 2014; The registry of the International Society for Heart and Lung Transplantation: thirty-first official adult heart transplant report--2014; focus theme: retransplantation. J Heart Lung Transplant. 33:996–1008. DOI: 10.1016/j.healun.2014.08.003. PMID: 25242124.5. Cook JA, Shah KB, Quader MA, Cooke RH, Kasirajan V, Rao KK, et al. 2015; The total artificial heart. J Thorac Dis. 7:2172–80. DOI: 10.21037/jtd.2017.02.66. PMID: 26793338. PMCID: PMC4703693.6. Kron IL, Tribble CG, Kern JA, Daniel TM, Rose CE, Truwit JD, et al. 1993; Successful transplantation of marginally acceptable thoracic organs. Ann Surg. 217:518–22. DOI: 10.1097/00000658-199305010-00012. PMID: 8489314. PMCID: PMC1242835.7. Mandegar MH, Bagheri J, Chitsaz S, Jebelli M, Javidi D, Sarzaeem MR, et al. 2009; Heart transplantation in Iran; a comprehensive single-center review of 15-year performance. Arch Iran Med. 12:111–5. PMID: 19249878.8. Ministry of Health. 2021. 2021 Organ donation statistics Tehran [Internet]. Tehran: Ministry of Health;cited 2022 Apr 1. Available from: medcare.health.gov.ir/hospman/dtsd/default.aspx.9. Ioannidis JP. 2018; Diagnosis and treatment of hypertension in the 2017 ACC/AHA guidelines and in the real world. JAMA. 319:115–6. DOI: 10.1001/jama.2017.19672. PMID: 29242891.10. Sharma AK, Metzger DL, Rodd CJ. 2018; Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics guidelines. JAMA Pediatr. 172:557–65. DOI: 10.1001/jamapediatrics.2018.0223. PMID: 29710187. PMCID: PMC6137536.11. Sanchis-Gomar F, Perez-Quilis C, Leischik R, Lucia A. 2016; Epidemiology of coronary heart disease and acute coronary syndrome. Ann Transl Med. 4:256. DOI: 10.21037/atm.2016.06.33. PMID: 27500157. PMCID: PMC4958723.12. Forni A, Luciani GB, Chiominto B, Pizzuti M, Mazzucco A, Faggian G. 2011; Results with expanded donor acceptance criteria in heart transplantation. Transplant Proc. 43:953–9. DOI: 10.1016/j.transproceed.2011.01.117. PMID: 21620025.13. Ministry of Health. 2021. Heart transplant guideline. 2021 Organ donation statistics Tehran [Internet]. Ministry of Health;Tehran: cited 2022 Apr 1. Available from: medcare.health.gov.ir/hospman/dtsd/default.aspx.14. Zaroff JG, Rosengard BR, Armstrong WF, Babcock WD, D'Alessandro A, Dec GW, et al. 2002; Consensus conference report: maximizing use of organs recovered from the cadaver donor: cardiac recommendations, March 28-29, 2001, Crystal City, Va. Circulation. 106:836–41. DOI: 10.1161/01.CIR.0000025587.40373.75. PMID: 12176957.15. Bombardini T, Gherardi S, Arpesella G, Maccherini M, Serra W, Magnani G, et al. 2011; Favorable short-term outcome of transplanted hearts selected from marginal donors by pharmacological stress echocardiography. J Am Soc Echocardiogr. 24:353–62. DOI: 10.1016/j.echo.2010.11.014. PMID: 21440213.16. Kobashigawa J, Khush K, Colvin M, Acker M, Van Bakel A, Eisen H, et al. 2017; Report from the American Society of Transplantation conference on donor heart selection in adult cardiac transplantation in the United States. Am J Transplant. 17:2559–66. DOI: 10.1111/ajt.14354. PMID: 28510318.17. Khush KK. 2018; Donor selection in the modern era. Ann Cardiothorac Surg. 7:126–34. DOI: 10.21037/acs.2017.09.09. PMID: 29492390. PMCID: PMC5827134.18. Lipshutz GS, Hiatt J, Ghobrial RM, Farmer DG, Martinez MM, Yersiz H, et al. 2007; Outcome of liver transplantation in septuagenarians: a single-center experience. Arch Surg. 142:775–81. DOI: 10.1001/archsurg.142.8.775. PMID: 17709732.19. Loebe M, Potapov EV, Hummel M, Weng Y, Bocksch W, Hetzer R. 2000; Medium-term results of heart transplantation using older donor organs. J Heart Lung Transplant. 19:957–63. DOI: 10.1016/S1053-2498(00)00178-9. PMID: 11044690.20. Drinkwater DC, Laks H, Blitz A, Kobashigawa J, Sabad A, Moriguchi J, et al. 1996; Outcomes of patients undergoing transplantation with older donor hearts. J Heart Lung Transplant. 15:684–91. PMID: 8820784.21. McCarthy JF, McCarthy PM, Massad MG, Cook DJ, Smedira NG, Kasirajan V, et al. 1998; Risk factors for death after heart transplantation: does a single-center experience correlate with multicenter registries? Ann Thorac Surg. 65:1574–8. DOI: 10.1016/S0003-4975(98)00138-6. PMID: 9647061.22. Mizraji R, Pérez S, Alvarez I. 2004; Brain death: epidemiology and quality control of solid organ donor generation. Transplant Proc. 36:1641–4. DOI: 10.1016/j.transproceed.2004.06.066. PMID: 15350439.23. Lima B, Rajagopal K, Petersen RP, Shah AS, Soule B, Felker GM, et al. 2006; Marginal cardiac allografts do not have increased primary graft dysfunction in alternate list transplantation. Circulation. 114(1 Suppl):I27–32. DOI: 10.1161/CIRCULATIONAHA.105.000737.24. Morgan JA, John R, Weinberg AD, Kherani AR, Colletti NJ, Vigilance DW, et al. 2003; Prolonged donor ischemic time does not adversely affect long-term survival in adult patients undergoing cardiac transplantation. J Thorac Cardiovasc Surg. 126:1624–33. DOI: 10.1016/S0022-5223(03)01026-2.25. Blanche C, Kamlot A, Blanche DA, Kearney B, Magliato KE, Czer LS, et al. 2002; Heart transplantation with donors fifty years of age and older. J Thorac Cardiovasc Surg. 123:810–5. DOI: 10.1067/mtc.2002.120009. PMID: 11986611.26. Reed RM, Netzer G, Hunsicker L, Mitchell BD, Rajagopal K, Scharf S, et al. 2014; Cardiac size and sex-matching in heart transplantation: size matters in matters of sex and the heart. JACC Heart Fail. 2:73–83. DOI: 10.1016/j.jchf.2013.09.005. PMID: 24611131. PMCID: PMC3941995.27. Ayesta A, Urrútia G, Madrid E, Vernooij RW, Vicent L, Martínez-Sellés M. 2019; Sex-mismatch influence on survival after heart transplantation: a systematic review and meta-analysis of observational studies. Clin Transplant. 33:e13737. DOI: 10.1111/ctr.13737. PMID: 31630456.28. Antelmi I, de Paula RS, Shinzato AR, Peres CA, Mansur AJ, Grupi CJ. 2004; Influence of age, gender, body mass index, and functional capacity on heart rate variability in a cohort of subjects without heart disease. Am J Cardiol. 93:381–5. DOI: 10.1016/j.amjcard.2003.09.065. PMID: 14759400.29. Wang Y, Cai J, Sun Y, Zhang J, Xie F, Alshirbini MH, et al. 2018; Extended donor criteria in heart transplantation: a retrospective study from a single Chinese institution. J Thorac Dis. 10:2153–65. DOI: 10.21037/jtd.2018.03.149. PMID: 29850119. PMCID: PMC5949496.30. Felker GM, Milano CA, Yager JE, Hernandez AF, Blue L, Higginbotham MB, et al. 2005; Outcomes with an alternate list strategy for heart transplantation. J Heart Lung Transplant. 24:1781–6. DOI: 10.1016/j.healun.2005.03.014. PMID: 16297782.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The clinical outcomes of marginal donor hearts: a single center experience
- Evaluating heart transplantation outcomes from marginal donors
- The Clinical Outcomes of Marginal Donor Hearts: A Single Center Experience
- A Single Center Experience for a Feasibility of Totally Laparoscopic Living Donor Right Hepatectomy
- A Preliminary Study to Revise the Marginal Donor Criteria of KONOS in Deceased Donor Kidney Transplantation