J Stroke.
2022 May;24(2):296-299. 10.5853/jos.2021.04385.
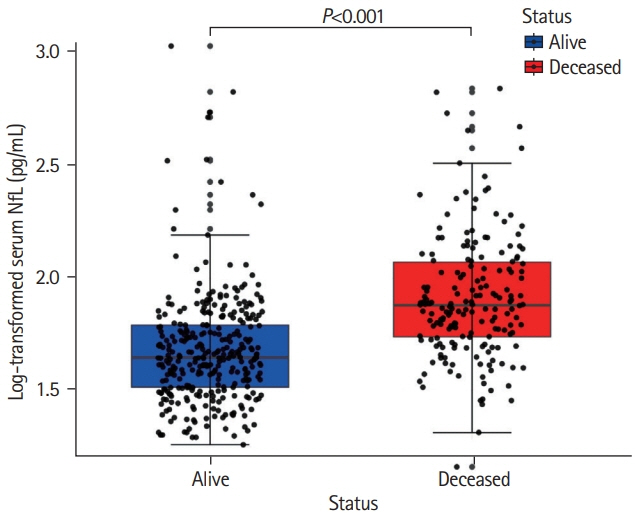
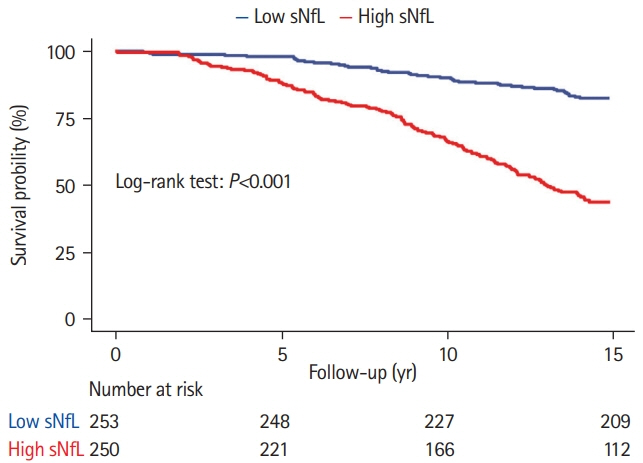
Increased Neurofilament Light Chain Is Associated with Increased Risk of Long-Term Mortality in Cerebral Small Vessel Disease
- Affiliations
-
- 1Department of Neurology, Donders Center for Medical Neurosciences, Radboud University Medical Center, Nijmegen, The Netherlands
- 2Stroke Center and Department of Neurology, University Hospital Basel, University of Basel, Basel, Switzerland
- 3University Center for Medicine of Aging, Felix Platter Hospital, Basel, Switzerland
- 4Stroke Center, Klinik Hirslanden, Zürich, Switzerland
- 5Medical Image Analysis Center (MIAC AG) and Quantitative Biomedical Imaging Group (qbig), Department of Biomedical Engineering, University of Basel, Basel, Switzerland
- 6Neurologic Clinic and Policlinic, Department of Medicine, Biomedicine and Clinical Research, University Hospital Basel, University of Basel, Switzerland
- KMID: 2530533
- DOI: http://doi.org/10.5853/jos.2021.04385
Figure
Reference
-
References
1. Ikram MA, Vernooij MW, Vrooman HA, Hofman A, Breteler MM. Brain tissue volumes and small vessel disease in relation to the risk of mortality. Neurobiol Aging. 2009; 30:450–456.
Article2. Bacioglu M, Maia LF, Preische O, Schelle J, Apel A, Kaeser SA, et al. Neurofilament light chain in blood and CSF as marker of disease progression in mouse models and in neurodegenerative diseases. Neuron. 2016; 91:56–66.
Article3. Peters N, van Leijsen E, Tuladhar AM, Barro C, Konieczny MJ, Ewers M, et al. Serum neurofilament light chain is associated with incident lacunes in progressive cerebral small vessel disease. J Stroke. 2020; 22:369–376.
Article4. Duering M, Konieczny MJ, Tiedt S, Baykara E, Tuladhar AM, Leijsen EV, et al. Serum neurofilament light chain levels are related to small vessel disease burden. J Stroke. 2018; 20:228–238.
Article5. Van Norden AG, de Laat KF, Gons RA, van Uden IW, van Dijk EJ, van Oudheusden LJ, et al. Causes and consequences of cerebral small vessel disease. The RUN DMC study: a prospective cohort study. Study rationale and protocol. BMC Neurol. 2011; 11:29.
Article6. Baranzini SE, Wang J, Gibson RA, Galwey N, Naegelin Y, Barkhof F, et al. Genome-wide association analysis of susceptibility and clinical phenotype in multiple sclerosis. Hum Mol Genet. 2009; 18:767–778.
Article7. Khalil M, Pirpamer L, Hofer E, Voortman MM, Barro C, Leppert D, et al. Serum neurofilament light levels in normal aging and their association with morphologic brain changes. Nat Commun. 2020; 11:812.
Article8. Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013; 12:822–838.
Article9. Egle M, Loubiere L, Maceski A, Kuhle J, Peters N, Markus HS. Neurofilament light chain predicts future dementia risk in cerebral small vessel disease. J Neurol Neurosurg Psychiatry. 2021; 92:582–589.
Article10. Gattringer T, Pinter D, Enzinger C, Seifert-Held T, Kneihsl M, Fandler S, et al. Serum neurofilament light is sensitive to active cerebral small vessel disease. Neurology. 2017; 89:2108–2114.
Article11. Qu Y, Tan CC, Shen XN, Li HQ, Cui M, Tan L, et al. Association of plasma neurofilament light with small vessel disease burden in nondemented elderly: a longitudinal study. Stroke. 2021; 52:896–904.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serum Neurofilament Light Chain Is Associated with Incident Lacunes in Progressive Cerebral Small Vessel Disease
- Cerebral Small Vessel Disease and Chronic Kidney Disease
- Vascular Overload Index Predicts Cerebral Small Vessel Disease in a Neurologically Healthy Population
- Prognostic Impact of Cerebral Small Vessel Disease on Stroke Outcome
- Relationship between Methylenetetrahydrofolate Reductase C677T Homozygous Mutation and Cerebral Small Vessel Disease Subtypes