Diabetes Metab J.
2022 May;46(3):486-498. 10.4093/dmj.2021.0095.
Sex Differences of Visceral Fat Area and Visceral-to-Subcutaneous Fat Ratio for the Risk of Incident Type 2 Diabetes Mellitus
- Affiliations
-
- 1Health Screening and Promotion Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, University of Ulsan College of Medicine, Seoul, Korea
- 3Asan Diabetes Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- KMID: 2530187
- DOI: http://doi.org/10.4093/dmj.2021.0095
Abstract
- Background
This study aimed to determine the optimal cut-off values of visceral fat area (VFA) and visceral-to-subcutaneous fat ratio (VSR) for predicting incident type 2 diabetes mellitus (T2DM).
Methods
A total of 10,882 individuals (6,835 men; 4,047 women) free of T2DM at baseline aged between 30 and 79 years who underwent abdominal computed tomography scan between 2012 and 2013 as a part of routine health check-ups were included and followed. VFA, subcutaneous fat area, and VSR on L3 vertebral level were measured at baseline.
Results
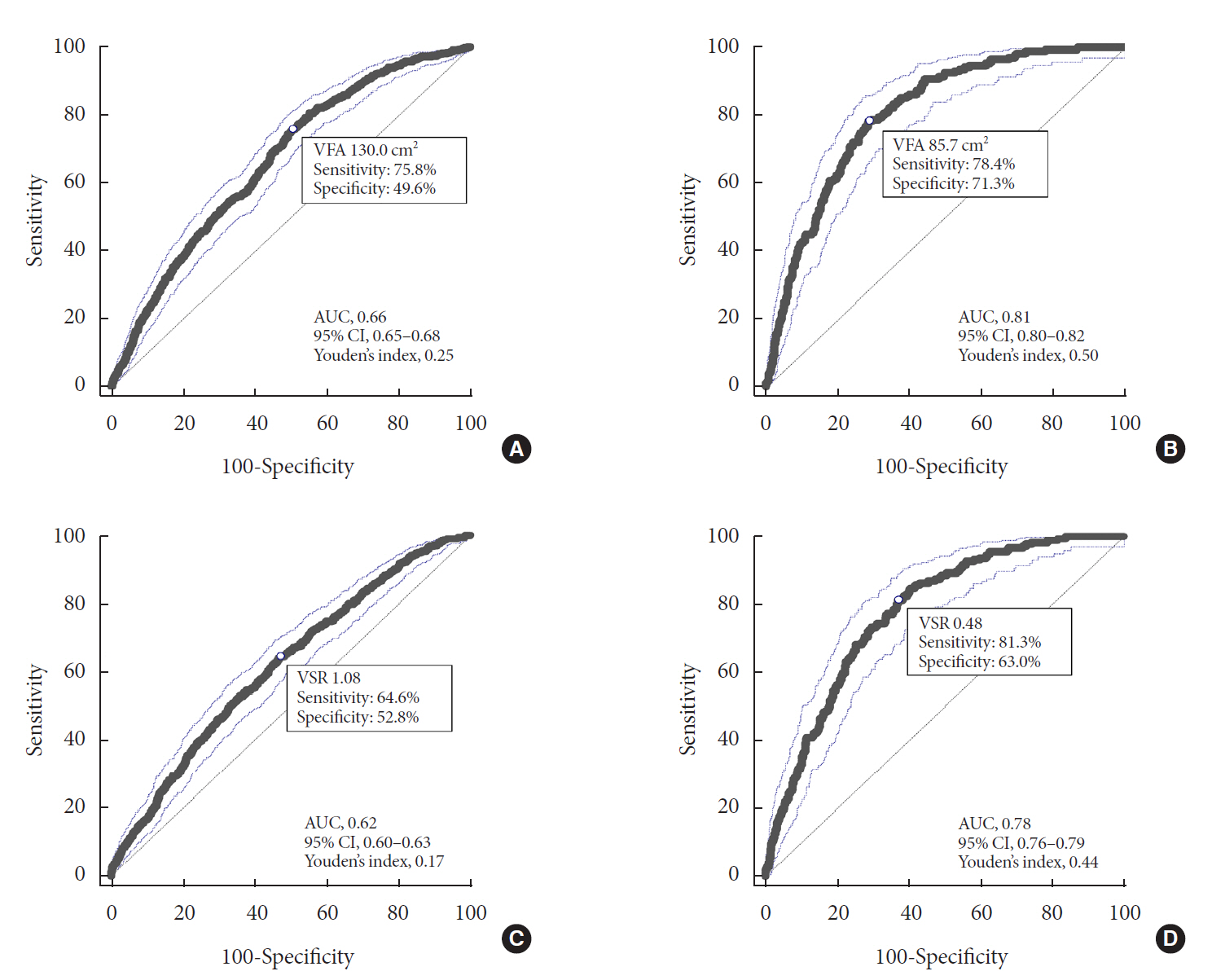
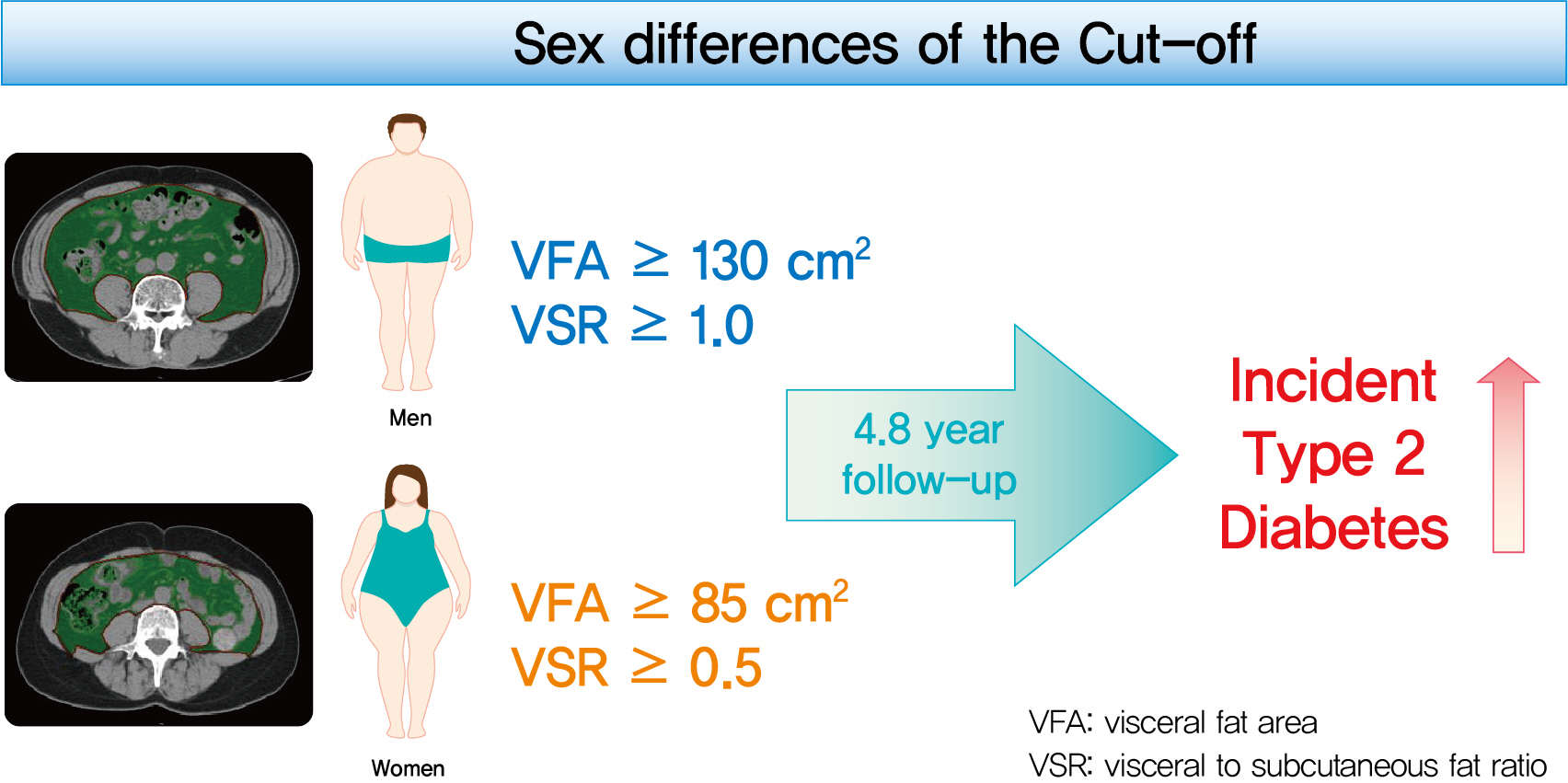
During a median follow-up of 4.8 years, 730 (8.1% for men; 4.3% for women) incident cases of T2DM were identified. Receiver operating characteristic curve analysis showed that the optimal cut-off values of VFA and VSR for predicting incident T2DM were 130.03 cm2 and 1.08 in men, respectively, and 85.7 cm2 and 0.48 in women, respectively. Regardless of sex, higher VFA and VSR were significantly associated with a higher risk of incident T2DM. Compared with the lowest quartiles of VFA and VSR, the highest quartiles had adjusted odds ratios of 2.62 (95% confidence interval [CI], 1.73 to 3.97) and 1.55 (95% CI, 1.14 to 2.11) in men, respectively, and 32.49 (95% CI, 7.42 to 142.02) and 11.07 (95% CI, 3.89 to 31.50) in women, respectively.
Conclusion
Higher VFA and VSR at baseline were independent risk factors for the development of T2DM. Sex-specific reference values for visceral fat obesity (VFA ≥130 cm2 or VSR ≥1.0 in men; VFA ≥85 cm2 or VSR ≥0.5 in women) are proposed for the prediction of incident T2DM.
Figure
Cited by 1 articles
-
Implication of Sex Differences in Visceral Fat for the Assessment of Incidence Risk of Type 2 Diabetes Mellitus
Sang Hyeon Ju, Hyon-Seung Yi
Diabetes Metab J. 2022;46(3):414-416. doi: 10.4093/dmj.2022.0089.
Reference
-
1. Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014; 103:137–49.
Article2. Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond). 2008; 32:1431–7.
Article3. Lebovitz HE, Banerji MA. Point: visceral adiposity is causally related to insulin resistance. Diabetes Care. 2005; 28:2322–5.
Article4. Wander PL, Boyko EJ, Leonetti DL, McNeely MJ, Kahn SE, Fujimoto WY. Change in visceral adiposity independently predicts a greater risk of developing type 2 diabetes over 10 years in Japanese Americans. Diabetes Care. 2013; 36:289–93.
Article5. Neeland IJ, Turer AT, Ayers CR, Powell-Wiley TM, Vega GL, Farzaneh-Far R, et al. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA. 2012; 308:1150–9.
Article6. Jung SH, Ha KH, Kim DJ. Visceral fat mass has stronger associations with diabetes and prediabetes than other anthropometric obesity indicators among Korean adults. Yonsei Med J. 2016; 57:674–80.
Article7. Brochu M, Starling RD, Tchernof A, Matthews DE, Garcia-Rubi E, Poehlman ET. Visceral adipose tissue is an independent correlate of glucose disposal in older obese postmenopausal women. J Clin Endocrinol Metab. 2000; 85:2378–84.
Article8. Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care. 2000; 23:465–71.
Article9. Lv X, Zhou W, Sun J, Lin R, Ding L, Xu M, et al. Visceral adiposity is significantly associated with type 2 diabetes in middle-aged and elderly Chinese women: a cross-sectional study. J Diabetes. 2017; 9:920–8.
Article10. Bays HE. Adiposopathy is “sick fat” a cardiovascular disease? J Am Coll Cardiol. 2011; 57:2461–73.11. Park HJ, Shin Y, Park J, Kim H, Lee IS, Seo DW, et al. Development and validation of a deep learning system for segmentation of abdominal muscle and fat on computed tomography. Korean J Radiol. 2020; 21:88–100.
Article12. Kim JA, Choi CJ, Yum KS. Cut-off values of visceral fat area and waist circumference: diagnostic criteria for abdominal obesity in a Korean population. J Korean Med Sci. 2006; 21:1048–53.
Article13. Han JH, Park HS, Kim SM, Lee SY, Kim DJ, Choi WH. Visceral adipose tissue as a predictor for metabolic risk factors in the Korean population. Diabet Med. 2008; 25:106–10.
Article14. Seo JA, Kim BG, Cho H, Kim HS, Park J, Baik SH, et al. The cutoff values of visceral fat area and waist circumference for identifying subjects at risk for metabolic syndrome in elderly Korean: Ansan Geriatric (AGE) cohort study. BMC Public Health. 2009; 9:443.
Article15. Kim HI, Kim JT, Yu SH, Kwak SH, Jang HC, Park KS, et al. Gender differences in diagnostic values of visceral fat area and waist circumference for predicting metabolic syndrome in Koreans. J Korean Med Sci. 2011; 26:906–13.
Article16. Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, et al. Optimal cut points of waist circumference (WC) and visceral fat area (VFA) predicting for metabolic syndrome (MetS) in elderly population in the Korean Longitudinal Study on Health and Aging (KLoSHA). Arch Gerontol Geriatr. 2012; 54:e29–34.
Article17. Lee A, Kim YJ, Oh SW, Lee CM, Choi HC, Joh HK, et al. Cutoff values for visceral fat area identifying Korean adults at risk for metabolic syndrome. Korean J Fam Med. 2018; 39:239–46.
Article18. Park DW, Park NH, Park JY, Kim SJ. Relationship between abdominal fat area measured by screening abdominal fat CT and metabolic syndrome in asymptomatic Korean individuals. J Korean Soc Radiol. 2017; 77:1–8.
Article19. Examination committee of criteria for ‘obesity disease’ in Japan; Japan Society for the Study of Obesity. New criteria for ‘obesity disease’ in Japan. Circ J. 2002; 66:987–92.20. Hiuge-Shimizu A, Kishida K, Funahashi T, Ishizaka Y, Oka R, Okada M, et al. Absolute value of visceral fat area measured on computed tomography scans and obesity-related cardiovascular risk factors in large-scale Japanese general population (the VACATION-J study). Ann Med. 2012; 44:82–92.
Article21. Nicklas BJ, Penninx BW, Ryan AS, Berman DM, Lynch NA, Dennis KE. Visceral adipose tissue cutoffs associated with metabolic risk factors for coronary heart disease in women. Diabetes Care. 2003; 26:1413–20.
Article22. Hayashi T, Boyko EJ, McNeely MJ, Leonetti DL, Kahn SE, Fujimoto WY. Minimum waist and visceral fat values for identifying Japanese Americans at risk for the metabolic syndrome. Diabetes Care. 2007; 30:120–7.
Article23. White UA, Tchoukalova YD. Sex dimorphism and depot differences in adipose tissue function. Biochim Biophys Acta. 2014; 1842:377–92.
Article24. Kim EH, Kim HK, Bae SJ, Lee MJ, Hwang JY, Choe J, et al. Gender differences of visceral fat area for predicting incident type 2 diabetes in Koreans. Diabetes Res Clin Pract. 2018; 146:93–100.
Article25. Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism. 1987; 36:54–9.
Article26. Oh YH, Moon JH, Kim HJ, Kong MH. Visceral-to-subcutaneous fat ratio as a predictor of the multiple metabolic risk factors for subjects with normal waist circumference in Korea. Diabetes Metab Syndr Obes. 2017; 10:505–11.
Article27. Kaess BM, Pedley A, Massaro JM, Murabito J, Hoffmann U, Fox CS. The ratio of visceral to subcutaneous fat, a metric of body fat distribution, is a unique correlate of cardiometabolic risk. Diabetologia. 2012; 55:2622–30.
Article28. Kim EH, Kim KW, Shin Y, Lee J, Ko Y, Kim YJ, et al. Reference data and T-scores of lumbar skeletal muscle area and its skeletal muscle indices measured by CT scan in a healthy Korean population. J Gerontol A Biol Sci Med Sci. 2021; 76:265–71.
Article29. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–45.
Article30. Kanaya AM, Harris T, Goodpaster BH, Tylavsky F, Cummings SR; Health, Aging, and Body Composition (ABC) Study. Adipocytokines attenuate the association between visceral adiposity and diabetes in older adults. Diabetes Care. 2004; 27:1375–80.
Article31. Hanley AJ, Wagenknecht LE, Norris JM, Bryer-Ash M, Chen YI, Anderson AM, et al. Insulin resistance, beta cell dysfunction and visceral adiposity as predictors of incident diabetes: the Insulin Resistance Atherosclerosis Study (IRAS) Family study. Diabetologia. 2009; 52:2079–86.
Article32. Karlsson T, Rask-Andersen M, Pan G, Hoglund J, Wadelius C, Ek WE, et al. Contribution of genetics to visceral adiposity and its relation to cardiovascular and metabolic disease. Nat Med. 2019; 25:1390–5.
Article33. Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr. 2007; 86:353–9.
Article34. Wajchenberg BL. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev. 2000; 21:697–738.
Article35. Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010; 11:11–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Insulin Resistance and Visceral Fat Obesity in Hyperlipidemia
- The Association of Visceral Fat Area with Anthropometric Variables and its Risk for Metabolic Syndrome
- Severity of Coronary Artery Disease and Visceral Fat Obesity
- Visceral Fat Accumulation in Coronary Artery Disease
- The Relationship between Visceral & Subcutaneous Fat and Small Dense Low Density Lipoprotein Cholesterol Concentration in Type 2 Diabetic Patients