Ann Hepatobiliary Pancreat Surg.
2022 May;26(2):204-209. 10.14701/ahbps.21-146.
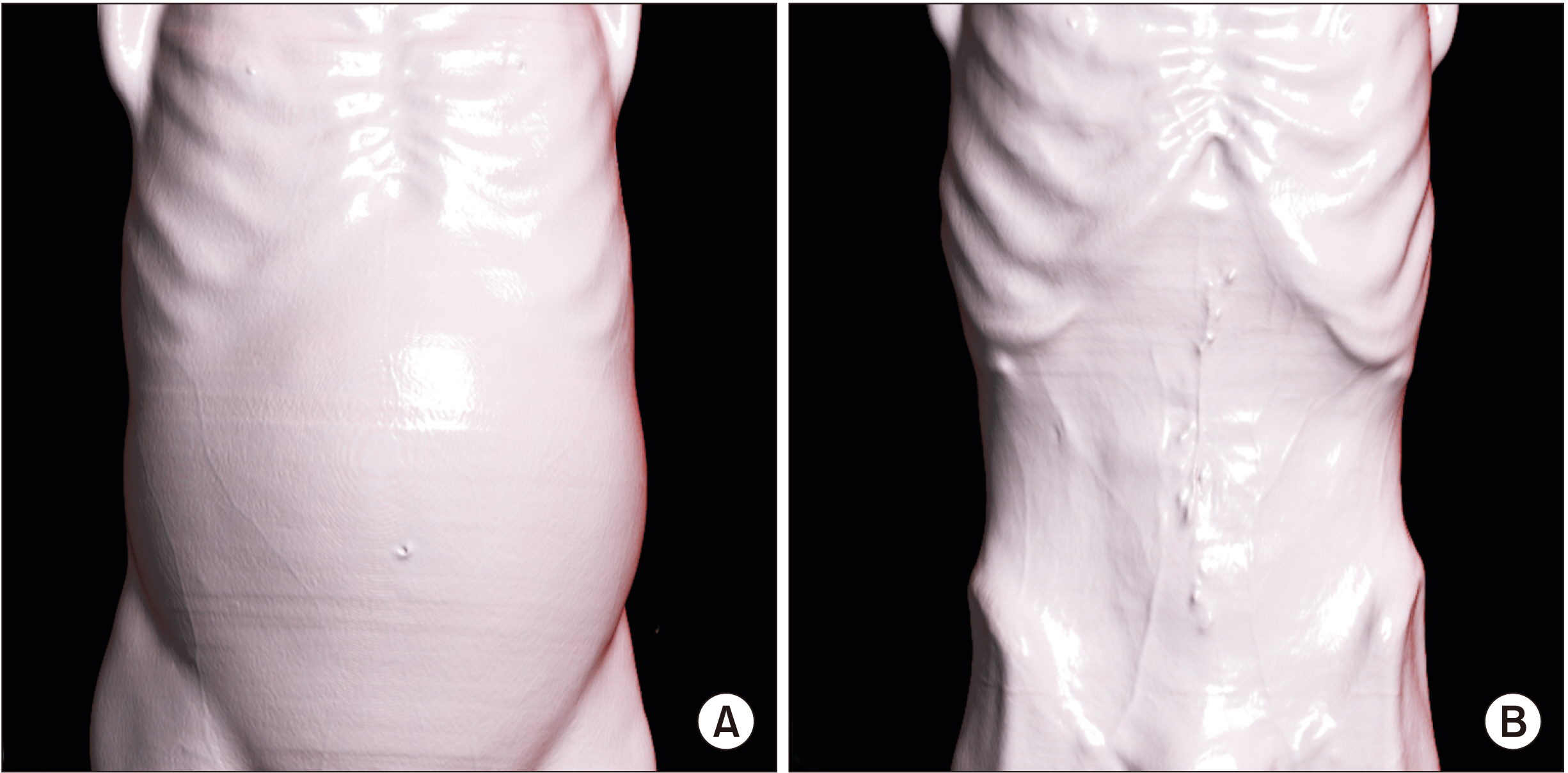
Successful use of a mesocaval shunt to treat refractory ascites in a chronic pancreatitis induced portal vein thrombosis
- Affiliations
-
- 1Division of Hepatopancreatobiliary Surgery, Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
- 2Department of Cardiovascular and Thoracic Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
- KMID: 2530101
- DOI: http://doi.org/10.14701/ahbps.21-146
Abstract
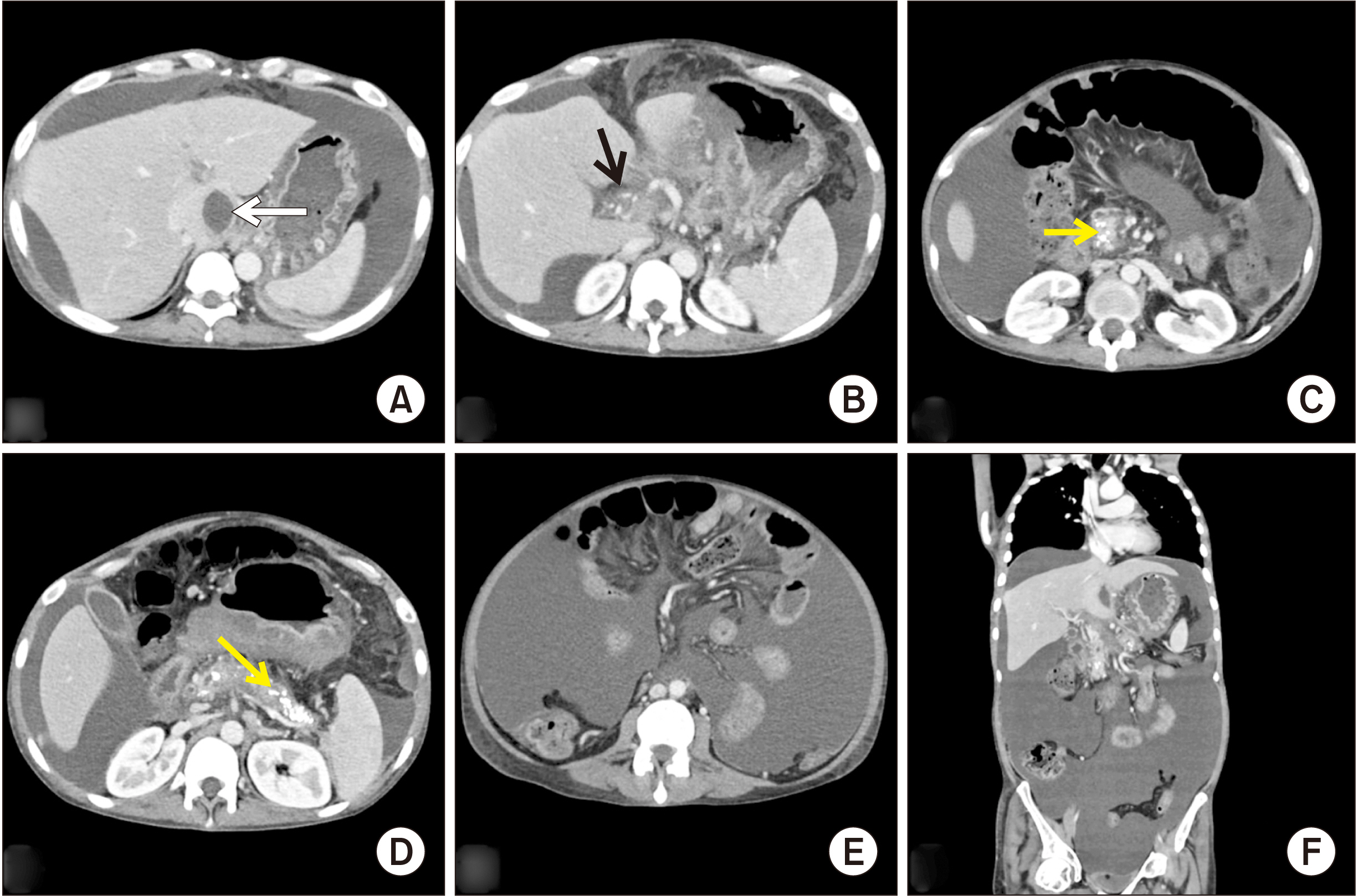
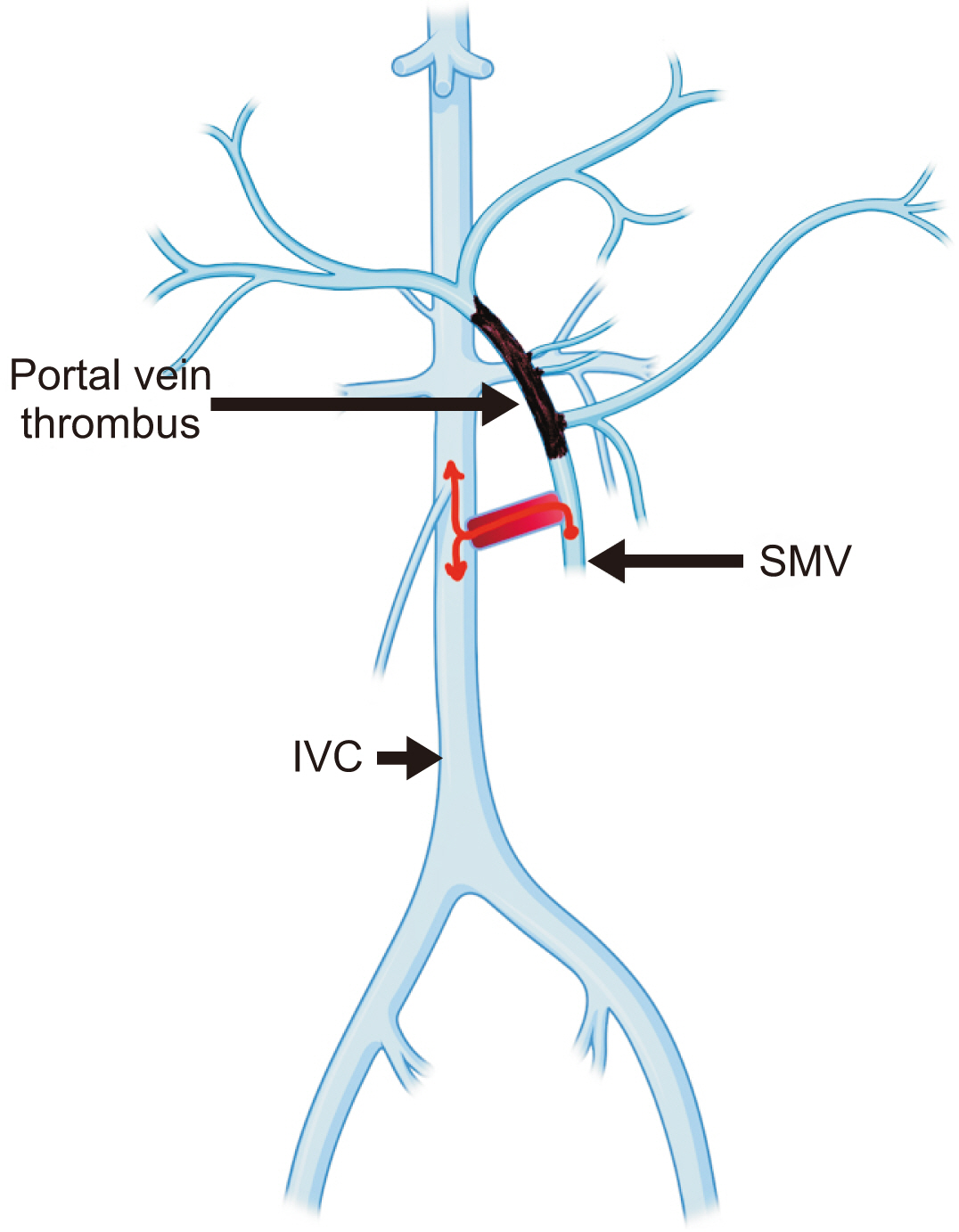
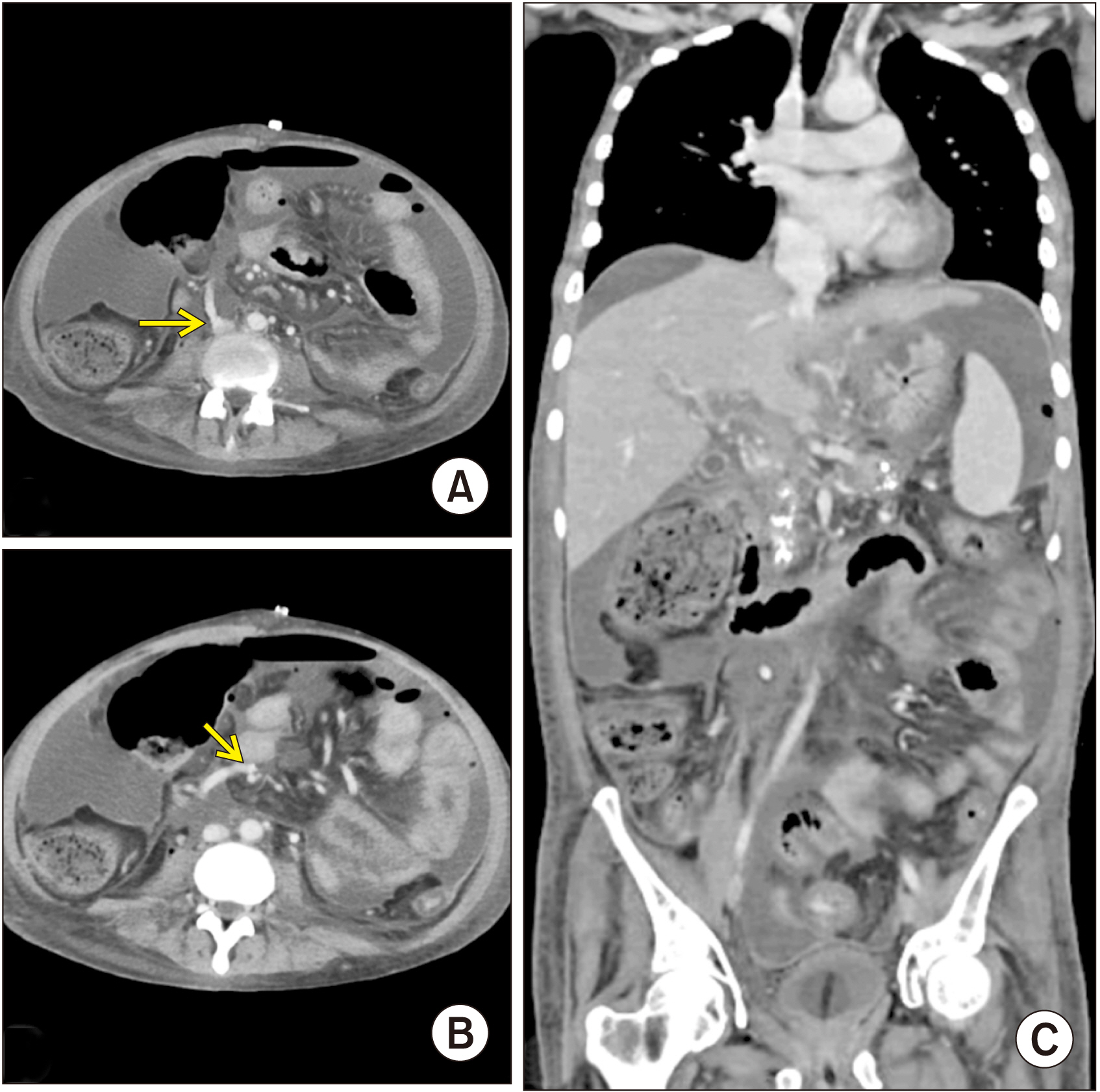
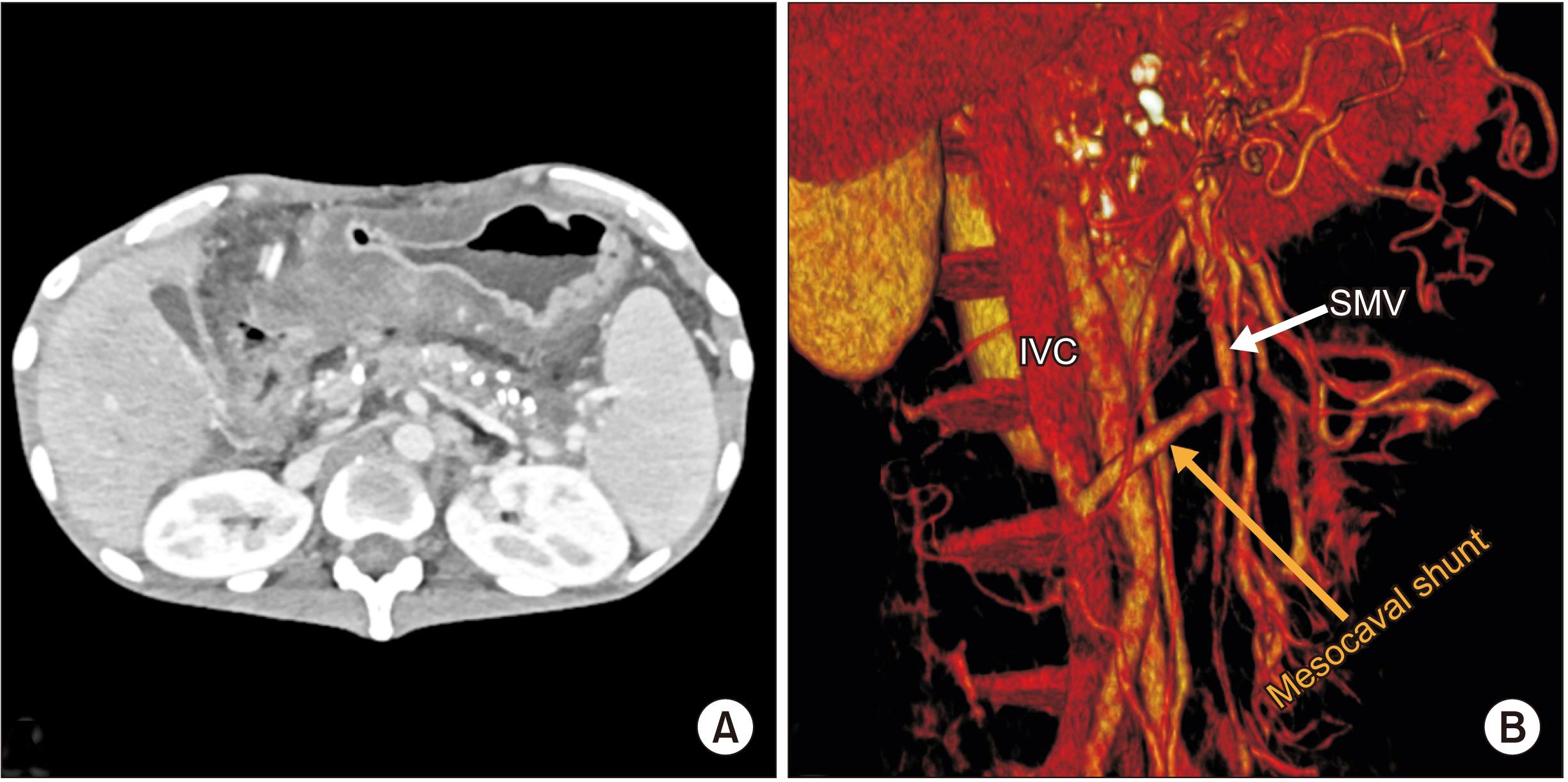
- The state of intense peripancreatic inf lammation in chronic pancreatitis can give rise to various vascular complications such as venous thrombosis and arterial pseudoaneurysms. Due to its intimate location with the pancreas, spleno-mesenteric-portal axis suffers the greatest blunt of thrombotic complications. Treatment modalities for such cases of chronic portal vein thrombosis have always been controversial and challenging. Medical management with anticoagulants is both risky and unsatisfactory due to presence of varices, hypersplenism, and persistence of the inf lammatory pathology. Although endovascular techniques have been tried in various case reports, there are definite anatomical challenges in cases of long segment porto-mesenteric thrombosis with massive ascites. Surgical shunts have been historically described for cirrhotic and non-cirrhotic portal hypertensive patients. However, its use in patients with refractory ascites due to chronic pancreatitis induced portal vein thrombosis has not been reported in the medical literature. Here, we present a case of an extensive portal vein thrombosis with massive refractory ascites in a patient with alcohol-induced chronic pancreatitis successfully treated with a surgical mesocaval shunt using an interposition small diameter graft.
Keyword
Figure
Reference
-
1. Etemad B, Whitcomb DC. 2001; Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterology. 120:682–707. DOI: 10.1053/gast.2001.22586. PMID: 11179244.
Article2. Anand A, Gunjan D, Agarwal S, Kaushal K, Sharma S, Gopi S, et al. 2020; Vascular complications of chronic pancreatitis: a tertiary center experience. Pancreatology. 20:1085–1091. DOI: 10.1016/j.pan.2020.07.005. PMID: 32800648.
Article3. Bernades P, Baetz A, Lévy P, Belghiti J, Menu Y, Fékété F. 1992; Splenic and portal venous obstruction in chronic pancreatitis. A prospective longitudinal study of a medical-surgical series of 266 patients. Dig Dis Sci. 37:340–346. DOI: 10.1007/BF01307725. PMID: 1735356.4. Chawla Y, Duseja A, Dhiman RK. 2009; Review article: the modern management of portal vein thrombosis. Aliment Pharmacol Ther. 30:881–894. DOI: 10.1111/j.1365-2036.2009.04116.x. PMID: 19678814.
Article5. Webster GJ, Burroughs AK, Riordan SM. 2005; Review article: portal vein thrombosis -- new insights into aetiology and management. Aliment Pharmacol Ther. 21:1–9. DOI: 10.1111/j.1365-2036.2004.02301.x. PMID: 15644039.
Article6. Stein M, Link DP. 1999; Symptomatic spleno-mesenteric-portal venous thrombosis: recanalization and reconstruction with endovascular stents. J Vasc Interv Radiol. 10:363–371. DOI: 10.1016/S1051-0443(99)70044-8. PMID: 10102204.
Article7. Plessier A, Darwish-Murad S, Hernandez-Guerra M, Consigny Y, Fabris F, Trebicka J, et al. 2010; Acute portal vein thrombosis unrelated to cirrhosis: a prospective multicenter follow-up study. Hepatology. 51:210–218. DOI: 10.1002/hep.23259. PMID: 19821530.
Article8. Loffredo L, Pastori D, Farcomeni A, Violi F. 2017; Effects of anticoagulants in patients with cirrhosis and portal vein thrombosis: a systematic review and meta-analysis. Gastroenterology. 153:480–487.e1. DOI: 10.1053/j.gastro.2017.04.042. PMID: 28479379.
Article9. Orr DW, Harrison PM, Devlin J, Karani JB, Kane PA, Heaton ND, et al. 2007; Chronic mesenteric venous thrombosis: evaluation and determinants of survival during long-term follow-up. Clin Gastroenterol Hepatol. 5:80–86. DOI: 10.1016/j.cgh.2006.09.030. PMID: 17142105.
Article10. Han G, Qi X, He C, Yin Z, Wang J, Xia J, et al. 2011; Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J Hepatol. 54:78–88. DOI: 10.1016/j.jhep.2010.06.029. PMID: 20932597.
Article11. Moriarty JM, Kokabi N, Kee ST. 2012; Transvenous creation of a mesocaval shunt: report of use in the management of extrahepatic portal vein occlusion. J Vasc Interv Radiol. 23:565–567. DOI: 10.1016/j.jvir.2011.09.023. PMID: 22464719.
Article12. Santy P, Marion P. 1953; [Technics of portacaval derivations]. Sem Hop. 29:2758–2767. French. PMID: 13113234.13. Clatworthy HW, Wall T, Watman RN. 1955; A new type of portal-to-systemic venous shunt for portal hypertension. AMA Arch Surg. 71:588–599. DOI: 10.1001/archsurg.1955.01270160114014.
Article14. Drapanas T. 1972; Interposition mesocaval shunt for treatment of portal hypertension. Ann Surg. 176:435–448. DOI: 10.1097/00000658-197210000-00001. PMID: 4263236. PMCID: PMC1355426.
Article15. Cameron JL, Zuidema GD, Smith GW, Harrington DP, Maddrey WC. 1979; Mesocaval shunts for the control of bleeding esophageal varices. Surgery. 85:257–262. DOI: 10.1016/s0022-3468(79)80179-7. PMID: 311525.16. Mangla V, Pal S, Sahni P. 2016; Surgery for non-cirrhotic portal hypertension: current status. Trop Gastroenterol. 37:152–155. DOI: 10.7869/tg.348.
Article17. Bommana V, Shah P, Kometa M, Narwal R, Sharma P. 2010; A case of isolated duodenal varices secondary to chronic pancreatitis with review of literature. Gastroenterology Res. 3:281–286. DOI: 10.4021/gr249w. PMID: 27942309. PMCID: PMC5139857.
Article18. Moore WS. 2018. Vascular and endovascular surgery e-book: a comprehensive review. 9th ed. Elsevier;Philadelphia: DOI: 10.7869/tg.348.19. Drapanas T, LoCicero J 3rd, Dowling JB. 1975; Hemodynamics of the interposition mesocaval shunt. Ann Surg. 181:523–533. DOI: 10.1097/00000658-197505000-00004. PMID: 124159. PMCID: PMC1345527.
Article20. Mercado MA, Orozco H, Guillén-Navarro E, Acosta E, López-Martínez LM, Hinojosa C, et al. 2000; Small-diameter mesocaval shunts: a 10-year evaluation. J Gastrointest Surg. 4:453–457. DOI: 10.1016/S1091-255X(00)80085-2. PMID: 11077318.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mesocaval Shunt Creation for Jejunal Variceal Bleeding with Chronic Portal Vein Thrombosis
- Chylous ascites caused by acute pancreatitis with portal vein thrombosis
- Rescue therapy using transjugular intrahepatic portosystemic shunt for sudden-onset portal vein thrombosis-associated ascites after living donor liver transplantation
- Refractory Ascites with Intrahepatic Portal Thrombosis after Living Donor Liver Transplantation Successfully Treated by Splenic Artery Embolization and Apixaban (Case Report)
- Portal flow augmentation using meso-reno-portal anastomosis during liver transplantation with severe portal vein thrombosis