Clin Endosc.
2022 May;55(3):426-433. 10.5946/ce.2021.239.
Increased ERCP volume improves cholangiogram interpretation: a new performance measure for ERCP training?
- Affiliations
-
- 1Department of Medicine, University of Miami, Miami, FL, USA
- 2Division of Digestive Health and Liver Diseases, Department of Medicine, University of Miami, Miami, FL, USA
- 3Department of Interventional Radiology, University Hospital Southampton NHS Foundation Trust, Southampton, UK
- 4Department of Gastroenterology, Sherwood Forest Hospitals NHS Foundation Trust, Sutton in Ashfield, UK
- 5Department of Gastroenterology, Liaquat National Hospital and Medical College, Karachi, Pakistan
- 6Interventional Endoscopy Unit, Surgical Unit 4, Dow University of Health Sciences, Karachi, Pakistan
- 7Southampton Interventional Endoscopy Unit, University Hospital Southampton NHS Foundation Trust, Southampton, UK
- KMID: 2529965
- DOI: http://doi.org/10.5946/ce.2021.239
Abstract
- Background/Aims
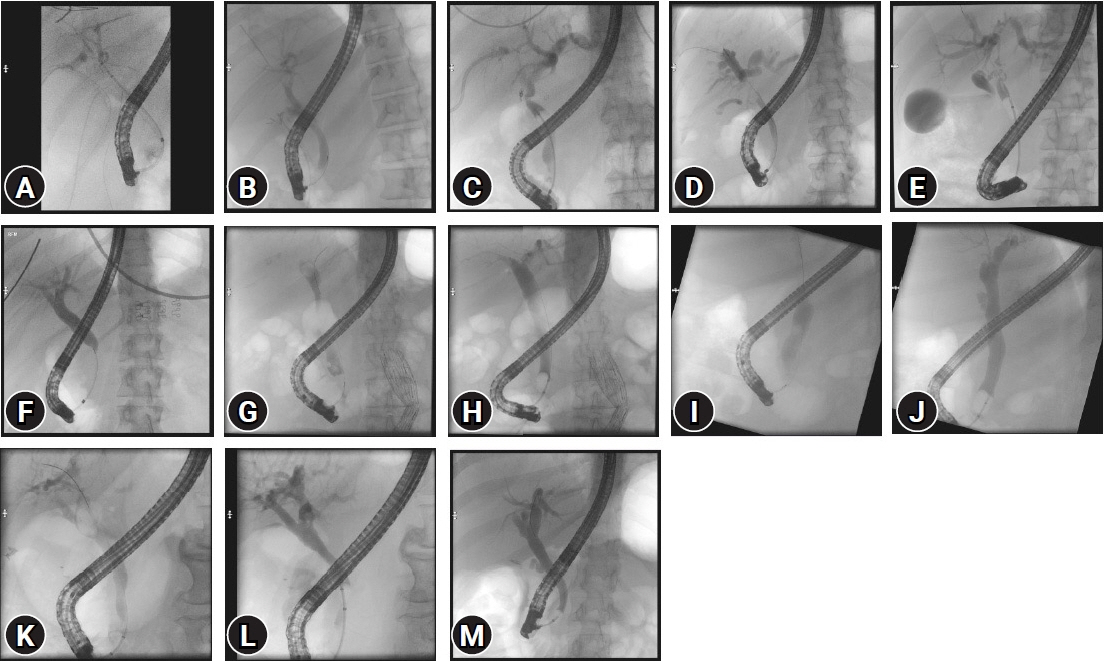
Cholangiogram interpretation is not used as a key performance indicator (KPI) of endoscopic retrograde cholangiopancreatography (ERCP) training, and national societies recommend different minimum numbers per annum to maintain competence. This study aimed to determine the relationship between correct ERCP cholangiogram interpretation and experience.
Methods
One hundred fifty ERCPists were surveyed to appropriately interpret ERCP cholangiographic findings. There were three groups of 50 participants each: “Trainees,” “Consultants group 1” (performed >75 ERCPs per year), and “Consultants group 2” (performed >100 ERCPs per year).
Results
Trainees was inferior to Consultants groups 1 and 2 in identifying all findings except choledocholithiasis outside the intrahepatic duct on the initial or completion/occlusion cholangiogram. Consultants group 1 was inferior to Consultants group 2 in identifying Strasberg type A bile leaks (odds ratio [OR], 0.86; 95% confidence interval [CI], 0.77–0.96), Strasberg type B (OR, 0.84; 95% CI, 0.74–0.95), and Bismuth type 2 hilar strictures (OR, 0.81; 95% CI, 0.69–0.95).
Conclusions
This investigation supports the notion that cholangiogram interpretation improves with increased annual ERCP case volumes. Thus, a higher annual volume of procedures performed may improve the ability to correctly interpret particularly difficult findings. Cholangiogram interpretation, in addition to bile duct cannulation, could be considered as another KPI of ERCP training.
Keyword
Figure
Reference
-
1. Costamagna G, Familiari P, Marchese M, et al. Endoscopic biliopancreatic investigations and therapy. Best Pract Res Clin Gastroenterol. 2008; 22:865–881.2. Kapral C, Mühlberger A, Wewalka F, et al. Quality assessment of endoscopic retrograde cholangiopancreatography: results of a running nationwide Austrian benchmarking project after 5 years of implementation. Eur J Gastroenterol Hepatol. 2012; 24:1447–1454.3. Elta GH, Jorgensen J, Coyle WJ. Training in interventional endoscopy: current and future state. Gastroenterology. 2015; 148:488–490.4. Wani S, Keswani RN, Han S, et al. Competence in endoscopic ultrasound and endoscopic retrograde cholangiopancreatography, from training through independent practice. Gastroenterology. 2018; 155:1483–1494.e7.5. Shahidi N, Ou G, Telford J, et al. When trainees reach competency in performing ERCP: a systematic review. Gastrointest Endosc. 2015; 81:1337–1342.6. Voiosu T, Bălănescu P, Voiosu A, et al. Measuring trainee competence in performing endoscopic retrograde cholangiopancreatography: a systematic review of the literature. United European Gastroenterol J. 2019; 7:239–249.7. Cappell MS, Friedel DM. Stricter national standards are required for credentialing of endoscopic-retrograde-cholangiopancreatography in the United States. World J Gastroenterol. 2019; 25:3468–3483.8. ASGE Training Committee, Jorgensen J, Kubiliun N, et al. Endoscopic retrograde cholangiopancreatography (ERCP): core curriculum. Gastrointest Endosc. 2016; 83:279–289.9. The British Society of Gastroenterology (BSG). ERCP: the way forward, a standards framework [Internet]. London: BSG;2013. [cited 2021 Dec 9]. Available from: https://www.bsg.org.uk/wp-content/uploads/2019/12/ERCP-%E2%80%93-The-Way-Forward-A-Standards-Framework-1.pdf.10. Adler DG, Lieb JG, Cohen J, et al. Quality indicators for ERCP. Gastrointest Endosc. 2015; 81:54–66.11. Domagk D, Oppong KW, Aabakken L, et al. Performance measures for ERCP and endoscopic ultrasound: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2018; 50:1116–1127.12. Sanjay P, Tagolao S, Dirkzwager I, et al. A survey of the accuracy of interpretation of intraoperative cholangiograms. HPB (Oxford). 2012; 14:673–676.13. Caglar E, Atasoy D, Tozlu M, et al. Experience of the endoscopists matters in endoscopic retrograde cholangiopancreatography in Billroth II gastrectomy patients. Clin Endosc. 2020; 53:82–89.14. Cotton PB. Are low-volume ERCPists a problem in the United States? A plea to examine and improve ERCP practice-NOW. Gastrointest Endosc. 2011; 74:161–166.15. Barkun AN, Rezieg M, Mehta SN, et al. Postcholecystectomy biliary leaks in the laparoscopic era: risk factors, presentation, and management. McGill Gallstone Treatment Group. Gastrointest Endosc. 1997; 45:277–282.16. Davids PH, Tanka AK, Rauws EA, et al. Benign biliary strictures. Surgery or endoscopy? Ann Surg. 1993; 217:237–243.17. Bergman JJ, van den Brink GR, Rauws EA, et al. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut. 1996; 38:141–147.18. Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998; 48:1–10.19. Tanner AR. ERCP: present practice in a single region. Suggested standards for monitoring performance. Eur J Gastroenterol Hepatol. 1996; 8:145–148.20. Masci E, Toti G, Mariani A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001; 96:417–423.21. Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007; 102:1781–1788.22. Chan CK, Pace RF. Misdiagnosis using endoscopic retrograde cholangiopancreatography in a patient with postcholecystectomy pain. Surg Endosc. 1987; 1:179–180.23. Trap R, Adamsen S, Hart-Hansen O, et al. Severe and fatal complications after diagnostic and therapeutic ERCP: a prospective series of claims to insurance covering public hospitals. Endoscopy. 1999; 31:125–130.24. Siau K, Webster G, Wright M, et al. Attitudes to radiation safety and cholangiogram interpretation in endoscopic retrograde cholangiopancreatography (ERCP): a UK survey. Frontline Gastroenterol. 2020; 12:550–556.25. Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998; 316:1236–1238.26. Nakagawa S. A farewell to Bonferroni: the problems of low statistical power and publication bias. Behavioral Ecology. 2004; 15:1044–1045.27. Desai R, Patel U, Doshi S, et al. A nationwide assessment of the “July Effect” and predictors of post-endoscopic retrograde cholangiopancreatography sepsis at urban teaching hospitals in the United States. Clin Endosc. 2019; 52:486–496.28. Lee TY, Nakai Y. Is the July effect real in patients undergoing endoscopic retrograde cholangiopancreatography? Clin Endosc. 2019; 52:399–400.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quality indicators in endoscopic retrograde cholangiopancreatography: a brief review of established guidelines
- Basic knowledge of endoscopic retrograde cholangiopancreatography
- Choledocal Cyst Diagnosed by Endoscopic Retrograde Cholangiopancreatography
- Why Should We Implement a System of Endoscopic Retrograde Cholangiopancreatography Certification?
- Basic Knowledge that Doctors Starting ERCP Should Know