Clin Endosc.
2022 May;55(3):372-380. 10.5946/ce.2021.152.
Epidemiology of early esophageal adenocarcinoma
- Affiliations
-
- 1Department of Medicine, Division of Digestive Diseases, Emory University, Atlanta, GA, USA
- 2Department of Medicine, Division of Gastroenterology, Duke University, Durham, NC, USA
- 3Department of Medicine, Division of Gastroenterology, Hepatology, and Nutrition, Vanderbilt University, Nashville, TN, USA
- 4Department of Biostatistics and Bioinformatics, Rollins School of Public Health, Emory University, Atlanta, GA, USA
- 5Department of Surgery, Division of Cardiothoracic Surgery, Emory University, Atlanta, GA, USA
- 6Emory Winship Cancer Institute, Department of Hematology and Medical Oncology, Emory University, Atlanta, GA, USA
- KMID: 2529959
- DOI: http://doi.org/10.5946/ce.2021.152
Abstract
- Background/Aims
Endoscopic resection has become the preferred treatment approach for select early esophageal adenocarcinoma (EAC); however, the epidemiology of early stage disease has not been well defined.
Methods
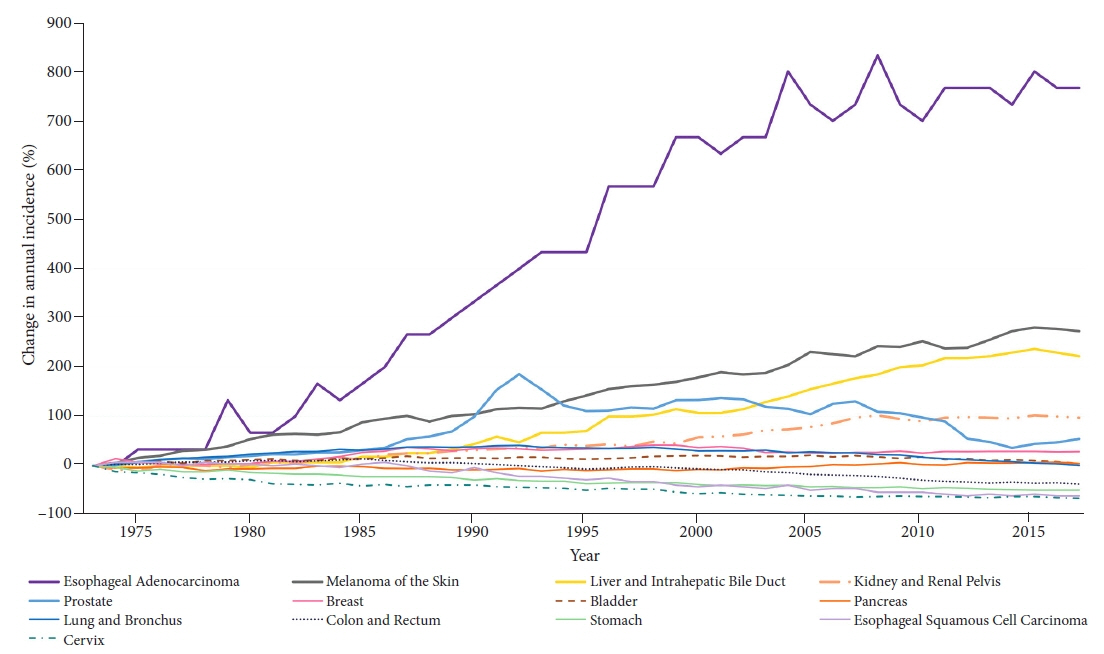
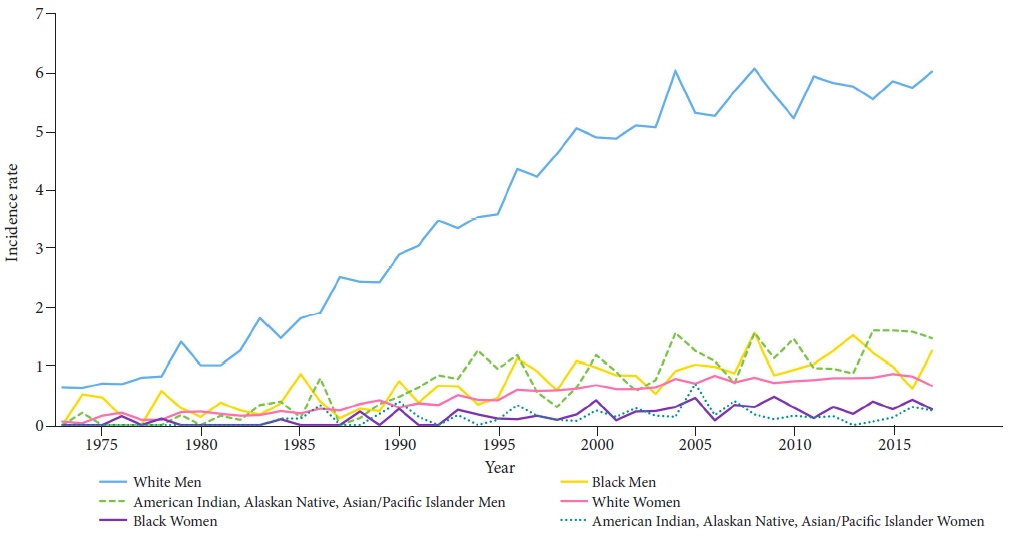
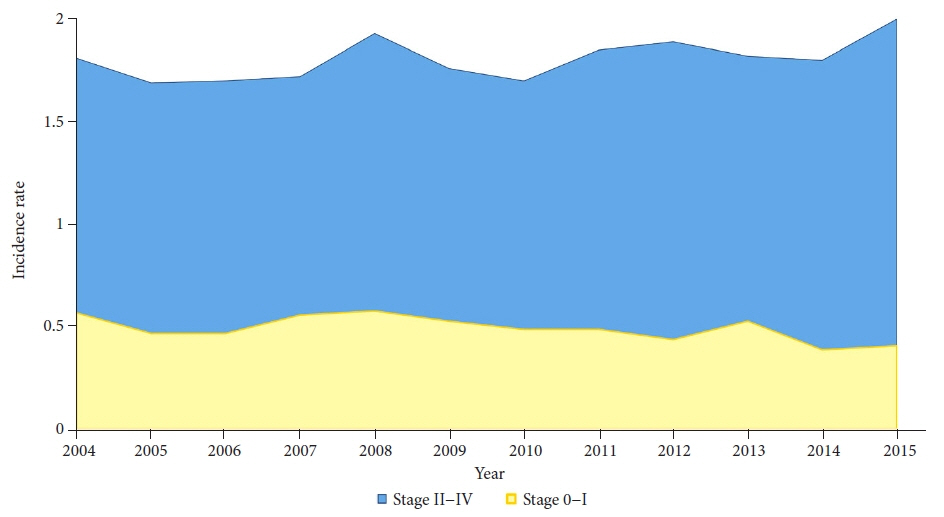
Surveillance Epidemiology and End Results (SEER) data were analyzed to determine age-adjusted incidence rates among major epithelial carcinomas, including EAC, from 1973 to 2017. The percent change in incidence over time was compared according to tumor subtype. Early T-stage, node-negative EAC without metastasis was examined from 2004 to 2017 when precise T-stage data were available.
Results
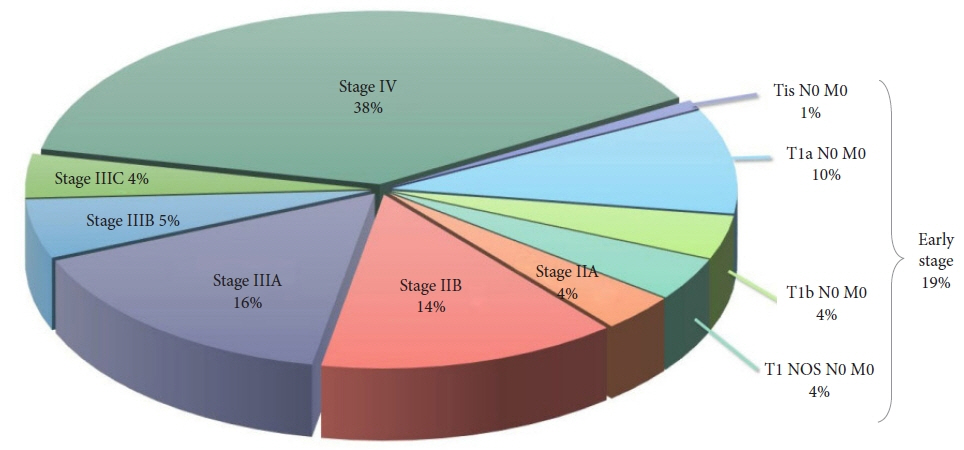
The percent change in annual incidence from 1973 to 2017 was 767% for EAC. Joinpoint analysis showed that the average annual percent change in EAC from 1973 to 2017 was 5.11% (95% confidence interval, 4.66%–5.56%). The annual percent change appeared to plateau between 2004 and 2017; however, early EAC decreased from 2010 to 2017, with an annual percent change of -5.78%.
Conclusions
There has been a 7-fold increase in the incidence of EAC, which was significantly greater than that of the other major epithelial malignancies examined. More recently, the incidence of early EAC has been decreasing. Approximately one in five patients has node negative, potentially resectable early stage disease.
Figure
Reference
-
1. American Cancer Society. Key statistics for esophageal cancer [Internet]. Kennesaw (GA): American Cancer Society;2021. [cited 2021 Dec 7]. Available from: https://www.cancer.org/cancer/esophagus-cancer/about/key-statistics.html.2. Lagergren J, Lagergren P. Recent developments in esophageal adenocarcinoma. CA Cancer J Clin. 2013; 63:232–248.3. Pohl H, Welch HG. The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst. 2005; 97:142–146.4. Hur C, Miller M, Kong CY, et al. Trends in esophageal adenocarcinoma incidence and mortality. Cancer. 2013; 119:1149–1158.5. Dubecz A, Gall I, Solymosi N, et al. Temporal trends in long-term survival and cure rates in esophageal cancer: a SEER database analysis. J Thorac Oncol. 2012; 7:443–447.6. Barnes JA, Willingham FF. Endoscopic management of early esophageal cancer. J Clin Gastroenterol. 2015; 49:638–646.7. National Institutes of Health. SEER*Stat software (version 8.3.9.2) [Internet]. Bethesda (MD): National Institutes of Health;2021. [cited 2021 Dec 7]. Available from: https://seer.cancer.gov/seerstat/index.html.8. Greene FL, Balch CM, Fleming ID, et al. AJCC cancer staging handbook: TNM classification of malignant tumors. 6th ed. New York (NY): Springer;2002.9. Edge S, Byrd DR, Compton CC, et al. AJCC cancer staging handbook: from the AJCC cancer staging manual. 7th ed. New York (NY): Springer;2010.10. National Institutes of Health. Joinpoint regression program [Internet]. Bethesda (MD): National Institutes of Health;[cited 2021 Dec 7]. Available from: https://surveillance.cancer.gov/joinpoint/.11. Murphy CC, Sandler RS, Sanoff HK, et al. Decrease in incidence of colorectal cancer among individuals 50 years or older after recommendations for population-based screening. Clin Gastroenterol Hepatol. 2017; 15:903–909.e6.12. Govindan R, Page N, Morgensztern D, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol. 2006; 24:4539–4544.13. Banks E, Canfell K. Recent declines in breast cancer incidence: mounting evidence that reduced use of menopausal hormones is largely responsible. Breast Cancer Res. 2010; 12:103.14. He H, Chen N, Hou Y, et al. Trends in the incidence and survival of patients with esophageal cancer: a SEER database analysis. Thorac Cancer. 2020; 11:1121–1128.15. Haiyu Z, Xiaofeng P, Xiangqiong M, et al. Incidence and survival changes in patients with esophageal adenocarcinoma during 1984-2013. Biomed Res Int. 2019; 2019:7431850.16. Then EO, Lopez M, Saleem S, et al. Esophageal cancer: an updated surveillance epidemiology and end results database analysis. World J Oncol. 2020; 11:55–64.17. Pech O, Behrens A, May A, et al. Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett’s oesophagus. Gut. 2008; 57:1200–1206.18. Peters FP, Kara MA, Rosmolen WD, et al. Endoscopic treatment of high-grade dysplasia and early stage cancer in Barrett’s esophagus. Gastrointest Endosc. 2005; 61:506–514.19. Larghi A, Lightdale CJ, Ross AS, et al. Long-term follow-up of complete Barrett’s eradication endoscopic mucosal resection (CBE-EMR) for the treatment of high grade dysplasia and intramucosal carcinoma. Endoscopy. 2007; 39:1086–1091.20. Ell C, May A, Pech O, et al. Curative endoscopic resection of early esophageal adenocarcinomas (Barrett’s cancer). Gastrointest Endosc. 2007; 65:3–10.21. May A, Gossner L, Pech O, et al. Intraepithelial high-grade neoplasia and early adenocarcinoma in short-segment Barrett’s esophagus (SSBE): curative treatment using local endoscopic treatment techniques. Endoscopy. 2002; 34:604–610.22. Seewald S, Akaraviputh T, Seitz U, et al. Circumferential EMR and complete removal of Barrett’s epithelium: a new approach to management of Barrett’s esophagus containing high-grade intraepithelial neoplasia and intramucosal carcinoma. Gastrointest Endosc. 2003; 57:854–859.23. Manner H, Pech O, Heldmann Y, et al. Efficacy, safety, and long-term results of endoscopic treatment for early stage adenocarcinoma of the esophagus with low-risk sm1 invasion. Clin Gastroenterol Hepatol. 2013; 11:630–635.24. Pech O, May A, Manner H, et al. Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus. Gastroenterology. 2014; 146:652–660.e1.25. Gamboa AM, Kim S, Force SD, et al. Treatment allocation in patients with early-stage esophageal adenocarcinoma: prevalence and predictors of lymph node involvement. Cancer. 2016; 122:2150–2157.26. Ajani JA, D’Amico TA, Almhanna K, et al. Esophageal and esophagogastric junction cancers, version 1.2015. J Natl Compr Canc Netw. 2015; 13:194–227.27. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020; 70:7–30.28. De Pergola G, Silvestris F. Obesity as a major risk factor for cancer. J Obes. 2013; 2013:291546.29. Nieman KM, Romero IL, Van Houten B, et al. Adipose tissue and adipocytes support tumorigenesis and metastasis. Biochim Biophys Acta. 2013; 1831:1533–1541.30. Chang P, Friedenberg F. Obesity and GERD. Gastroenterol Clin North Am. 2014; 43:161–173.31. Ness-Jensen E, Hveem K, El-Serag H, et al. Lifestyle intervention in gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2016; 14:175–182.e1-e3.32. Schlottmann F, Dreifuss NH, Patti MG. Obesity and esophageal cancer: GERD, Barrett´s esophagus, and molecular carcinogenic pathways. Expert Rev Gastroenterol Hepatol. 2020; 14:425–433.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Single Center's 30 Years' Experience of Esophageal Adenocarcinoma
- Epidemiology of and Risk Factors for Esophageal Cancer in Korea
- Diagnosis of Adenocarcinoima of the Esophageal Junction
- A Case of Primary Esophageal Adenocarcinoma Originated from Ectopic Gastric Mucosa in the Upper Esophagus
- Surgical Treatment of Esophageal Adenocarcinoma in Barrett's Esophagus: A case report