Clin Endosc.
2022 May;55(3):319-331. 10.5946/ce.2022.094.
Quality indicators in esophagogastroduodenoscopy
- Affiliations
-
- 1Department of Internal Medicine, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Catholic Photomedicine Research Institute, The Catholic University of Korea, Seoul, Korea
- KMID: 2529951
- DOI: http://doi.org/10.5946/ce.2022.094
Abstract
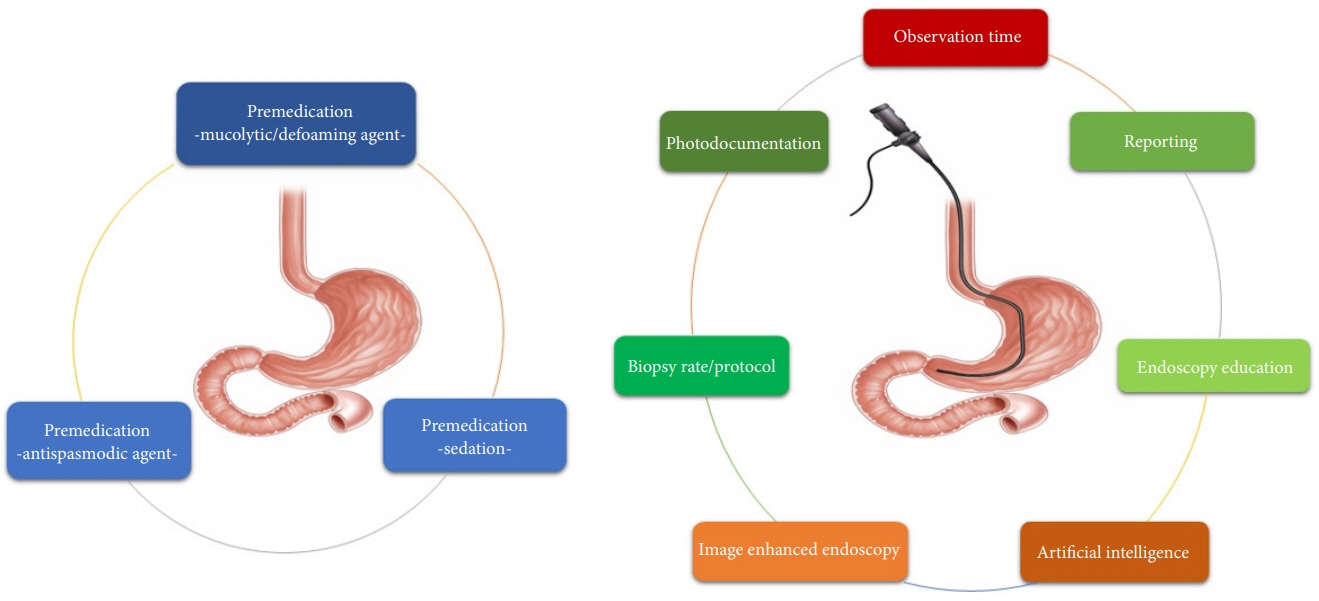
- Esophagogastroduodenoscopy (EGD) has been used to diagnose a wide variety of upper gastrointestinal diseases. In particular, EGD is used to screen high-risk subjects of gastric cancer. Quality control of EGD is important because the diagnostic rate is examiner-dependent. However, there is still no representative quality indicator that can be uniformly applied in EGD. There has been growing awareness of the importance of quality control in improving EGD performance. Therefore, we aimed to review the available and emerging quality indicators for diagnostic EGD.
Figure
Reference
-
1. Hamashima C, Ogoshi K, Narisawa R, et al. Impact of endoscopic screening on mortality reduction from gastric cancer. World J Gastroenterol. 2015; 21:2460–2466.2. Cohen J, Safdi MA, Deal SE, et al. Quality indicators for esophagogastroduodenoscopy. Am J Gastroenterol. 2006; 101:886–891.3. Park WG, Shaheen NJ, Cohen J, et al. Quality indicators for EGD. Gastrointest Endosc. 2015; 81:17–30.4. Park CH, Kim B, Chung H, et al. Endoscopic quality indicators for esophagogastroduodenoscopy in gastric cancer screening. Dig Dis Sci. 2015; 60:38–46.5. Beg S, Ragunath K, Wyman A, et al. Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut. 2017; 66:1886–1899.6. Min JK, Cha JM, Cho YK, et al. Revision of quality indicators for the endoscopy quality improvement program of the National Cancer Screening Program in Korea. Clin Endosc. 2018; 51:239–252.7. Chiu PWY, Uedo N, Singh R, et al. An Asian consensus on standards of diagnostic upper endoscopy for neoplasia. Gut. 2019; 68:186–197.8. Bisschops R, Areia M, Coron E, et al. Performance measures for upper gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2016; 48:843–864.9. Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010; 362:1795–1803.10. Keswani RN, Crockett SD, Calderwood AH. AGA clinical practice update on strategies to improve quality of screening and surveillance colonoscopy: expert review. Gastroenterology. 2021; 161:701–711.11. Barclay RL, Vicari JJ, Doughty AS, et al. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006; 355:2533–2541.12. Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2015; 81:31–53.13. Meining A, Riedl B, Stolte M. Features of gastritis predisposing to gastric adenoma and early gastric cancer. J Clin Pathol. 2002; 55:770–773.14. East JE, Vieth M, Rex DK. Serrated lesions in colorectal cancer screening: detection, resection, pathology and surveillance. Gut. 2015; 64:991–1000.15. Ren W, Yu J, Zhang ZM, et al. Missed diagnosis of early gastric cancer or high-grade intraepithelial neoplasia. World J Gastroenterol. 2013; 19:2092–2096.16. Chadwick G, Groene O, Hoare J, et al. A population-based, retrospective, cohort study of esophageal cancer missed at endoscopy. Endoscopy. 2014; 46:553–560.17. Pimenta-Melo AR, Monteiro-Soares M, Libânio D, et al. Missing rate for gastric cancer during upper gastrointestinal endoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2016; 28:1041–1049.18. Beck M, Bringeland EA, Qvigstad G, et al. Gastric cancers missed at upper endoscopy in Central Norway 2007 to 2016: a population-based study. Cancers (Basel). 2021; 13:5628.19. Uedo N, Gotoda T, Yoshinaga S, et al. Differences in routine esophagogastroduodenoscopy between Japanese and international facilities: a questionnaire survey. Dig Endosc. 2016; 28 Suppl 1:16–24.20. Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003; 58:76–79.21. Neale JR, James S, Callaghan J, et al. Premedication with N-acetylcysteine and simethicone improves mucosal visualization during gastroscopy: a randomized, controlled, endoscopist-blinded study. Eur J Gastroenterol Hepatol. 2013; 25:778–783.22. Lee GJ, Park SJ, Kim SJ, et al. Effectiveness of premedication with pronase for visualization of the mucosa during endoscopy: a randomized, controlled trial. Clin Endosc. 2012; 45:161–164.23. Liu X, Guan CT, Xue LY, et al. Effect of premedication on lesion detection rate and visualization of the mucosa during upper gastrointestinal endoscopy: a multicenter large sample randomized controlled double-blind study. Surg Endosc. 2018; 32:3548–3556.24. Chang WK, Yeh MK, Hsu HC, et al. Efficacy of simethicone and N-acetylcysteine as premedication in improving visibility during upper endoscopy. J Gastroenterol Hepatol. 2014; 29:769–774.25. Zhang Q, Chen ZY, Chen CD, et al. Training in early gastric cancer diagnosis improves the detection rate of early gastric cancer: an observational study in China. Medicine (Baltimore). 2015; 94:e384.26. Kim SY, Park JM, Cho HS, et al. Assessment of cimetropium bromide use for the detection of gastric neoplasms during esophagogastroduodenoscopy. JAMA Netw Open. 2022; 5:e223827.27. Omata F, Kumakura Y, Ishii N, et al. Noneffectiveness of scopolamine for facilitating detection of upper gastrointestinal neoplasia during screening esophagogastroduodenoscopy: propensity score-matched study. Endoscopy. 2020; 52:556–562.28. Cohen LB, Wecsler JS, Gaetano JN, et al. Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol. 2006; 101:967–974.29. McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008; 67:910–923.30. Bell GD, Quine A. Preparation, premedication, and surveillance. Endoscopy. 2006; 38:105–109.31. Fanti L, Testoni PA. Sedation and analgesia in gastrointestinal endoscopy: what’s new? World J Gastroenterol. 2010; 16:2451–2457.32. Zhou J, Li Z, Ji R, et al. Influence of sedation on the detection rate of early cancer and precancerous lesions during diagnostic upper gastrointestinal endoscopies: a multicenter retrospective study. Am J Gastroenterol. 2021; 116:1230–1237.33. Yao K. The endoscopic diagnosis of early gastric cancer. Ann Gastroenterol. 2013; 26:11–22.34. Lee JI, Kim JS, Kim BW, et al. Taking more gastroscopy images increases the detection rate of clinically significant gastric lesions: validation of a systematic screening protocol for the stomach. Korean J Helicobacter Up Gastrointest Res. 2020; 20:225–232.35. Park JM, Lim CH, Cho YK, et al. The effect of photo-documentation of the ampulla on neoplasm detection rate during esophagogastroduodenoscopy. Endoscopy. 2019; 51:115–124.36. Armstrong D, Bennett JR, Blum AL, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996; 111:85–92.37. Alvarez Herrero L, Curvers WL, van Vilsteren FG, et al. Validation of the Prague C&M classification of Barrett’s esophagus in clinical practice. Endoscopy. 2013; 45:876–882.38. Forrest JA, Finlayson ND, Shearman DJ. Endoscopy in gastrointestinal bleeding. Lancet. 1974; 2:394–397.39. Endoscopic Classification Review Group. Update on the Paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy. 2005; 37:570–578.40. Hirano I, Moy N, Heckman MG, et al. Endoscopic assessment of the oesophageal features of eosinophilic oesophagitis: validation of a novel classification and grading system. Gut. 2013; 62:489–495.41. Cheng HT, Cheng CL, Lin CH, et al. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol. 2008; 8:31.42. de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015; 63:743–752.43. Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008; 22:601–616.44. Spigelman AD, Williams CB, Talbot IC, et al. Upper gastrointestinal cancer in patients with familial adenomatous polyposis. Lancet. 1989; 2:783–785.45. Gupta N, Gaddam S, Wani SB, et al. Longer inspection time is associated with increased detection of high-grade dysplasia and esophageal adenocarcinoma in Barrett's esophagus. Gastrointest Endosc. 2012; 76:531–538.46. Teh JL, Tan JR, Lau LJ, et al. Longer examination time improves detection of gastric cancer during diagnostic upper gastrointestinal endoscopy. Clin Gastroenterol Hepatol. 2015; 13:480–487.47. Kawamura T, Wada H, Sakiyama N, et al. Examination time as a quality indicator of screening upper gastrointestinal endoscopy for asymptomatic examinees. Dig Endosc. 2017; 29:569–575.48. Park JM, Huo SM, Lee HH, et al. Longer observation time increases proportion of neoplasms detected by esophagogastroduodenoscopy. Gastroenterology. 2017; 153:460–469.49. Park JM, Kim SY, Shin GY, et al. Implementation effect of institutional policy of EGD observation time on neoplasm detection. Gastrointest Endosc. 2021; 93:1152–1159.50. Lee HH, Park JM, Lim CH, et al. The impact of pre-resection endoscopic examination time on the rate of synchronous gastric neoplasms missed during endoscopic treatment. Surg Endosc. 2017; 31:3952–3960.51. Choi Y, Choi HS, Jeon WK, et al. Optimal number of endoscopic biopsies in diagnosis of advanced gastric and colorectal cancer. J Korean Med Sci. 2012; 27:36–39.52. Hatfield AR, Slavin G, Segal AW, et al. Importance of the site of endoscopic gastric biopsy in ulcerating lesions of the stomach. Gut. 1975; 16:884–886.53. Pimentel-Nunes P, Libânio D, Marcos-Pinto R, et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019; 51:365–388.54. Januszewicz W, Wieszczy P, Bialek A, et al. Endoscopist biopsy rate as a quality indicator for outpatient gastroscopy: a multicenter cohort study with validation. Gastrointest Endosc. 2019; 89:1141–1149.55. Lee HS, Jeon SW. Barrett esophagus in Asia: same disease with different pattern. Clin Endosc. 2014; 47:15–22.56. Rex DK, Shaw M, Wong R. Prevalence of Barrett’s esophagus. Gastroenterology. 2006; 130:1373–1374.57. Levine DS. Management of dysplasia in the columnar-lined esophagus. Gastroenterol Clin North Am. 1997; 26:613–634.58. Dixon MF, Genta RM, Yardley JH, et al. Classification and grading of gastritis: the updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996; 20:1161–1181.59. Yue H, Shan L, Bin L. The significance of OLGA and OLGIM staging systems in the risk assessment of gastric cancer: a systematic review and meta-analysis. Gastric Cancer. 2018; 21:579–587.60. Yamazato T, Oyama T, Yoshida T, et al. Two years’ intensive training in endoscopic diagnosis facilitates detection of early gastric cancer. Intern Med. 2012; 51:1461–1465.61. Korean Society of Gastrointestinal Endoscopy. Quality Control E-learning [Internet]. Seoul: The Korean Society of Gastrointestinal Endoscopy;2020. [cited 2022 Mar 9]. Available from: https://www.gie.or.kr/disinfect/Elearning.php.62. National Cancer Center. National Cancer Screening Quality Improvement Online Education Program [Internet]. Goyang: National Cancer Center;2013. [cited 2022 Mar 9]. Available from: https://neweducation.ncc.re.kr/#.63. Lee W. Application of current image-enhanced endoscopy in gastric diseases. Clin Endosc. 2021; 54:477–487.64. Mabe K, Yao K, Nojima M, et al. An educational intervention to improve the endoscopist’s ability to correctly diagnose small gastric lesions using magnifying endoscopy with narrow-band imaging. Ann Gastroenterol. 2014; 27:149–155.65. Yang YJ, Bang CS. Application of artificial intelligence in gastroenterology. World J Gastroenterol. 2019; 25:1666–1683.66. Wu L, He X, Liu M, et al. Evaluation of the effects of an artificial intelligence system on endoscopy quality and preliminary testing of its performance in detecting early gastric cancer: a randomized controlled trial. Endoscopy. 2021; 53:1199–1207.67. Kuo CY, Chiu HM. Application of artificial intelligence in gastroenterology: potential role in clinical practice. J Gastroenterol Hepatol. 2021; 36:267–272.68. Bang CS, Lee JJ, Baik GH. Computer-aided diagnosis of esophageal cancer and neoplasms in endoscopic images: a systematic review and meta-analysis of diagnostic test accuracy. Gastrointest Endosc. 2021; 93:1006–1015.69. Choi SJ, Khan MA, Choi HS, et al. Development of artificial intelligence system for quality control of photo documentation in esophagogastroduodenoscopy. Surg Endosc. 2022; 36:57–65.70. Wu L, Zhang J, Zhou W, et al. Randomised controlled trial of WISENSE, a real-time quality improving system for monitoring blind spots during esophagogastroduodenoscopy. Gut. 2019; 68:2161–2169.71. Hirasawa T, Aoyama K, Tanimoto T, et al. Application of artificial intelligence using a convolutional neural network for detecting gastric cancer in endoscopic images. Gastric Cancer. 2018; 21:653–660.72. Menon S, Trudgill N. How commonly is upper gastrointestinal cancer missed at endoscopy? a meta-analysis. Endosc Int Open. 2014; 2:E46–E50.73. Yalamarthi S, Witherspoon P, McCole D, et al. Missed diagnoses in patients with upper gastrointestinal cancers. Endoscopy. 2004; 36:874–879.74. Chen D, Wu L, Li Y, et al. Comparing blind spots of unsedated ultrafine, sedated, and unsedated conventional gastroscopy with and without artificial intelligence: a prospective, single-blind, 3-parallel-group, randomized, single-center trial. Gastrointest Endosc. 2020; 91:332–339.75. Berzin TM, Parasa S, Wallace MB, et al. Position statement on priorities for artificial intelligence in GI endoscopy: a report by the ASGE Task Force. Gastrointest Endosc. 2020; 92:951–959.76. Sano T, Coit DG, Kim HH, et al. Proposal of a new stage grouping of gastric cancer for TNM classification: International Gastric Cancer Association staging project. Gastric Cancer. 2017; 20:217–225.77. Isomoto H, Shikuwa S, Yamaguchi N, et al. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009; 58:331–336.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Application of Nursing Service Quality Indicators in Nursing Homes
- Quality Indicators in Barrett's Esophagus: Time to Change the Status Quo
- Quality indicators in endoscopic retrograde cholangiopancreatography: a brief review of established guidelines
- Development of the Quality Indicators in Long Term Care Service
- Quality Indicators and Outcome Measures of Endoscopy in the National Cancer Screening Program