J Korean Assoc Oral Maxillofac Surg.
2022 Apr;48(2):79-84. 10.5125/jkaoms.2022.48.2.79.
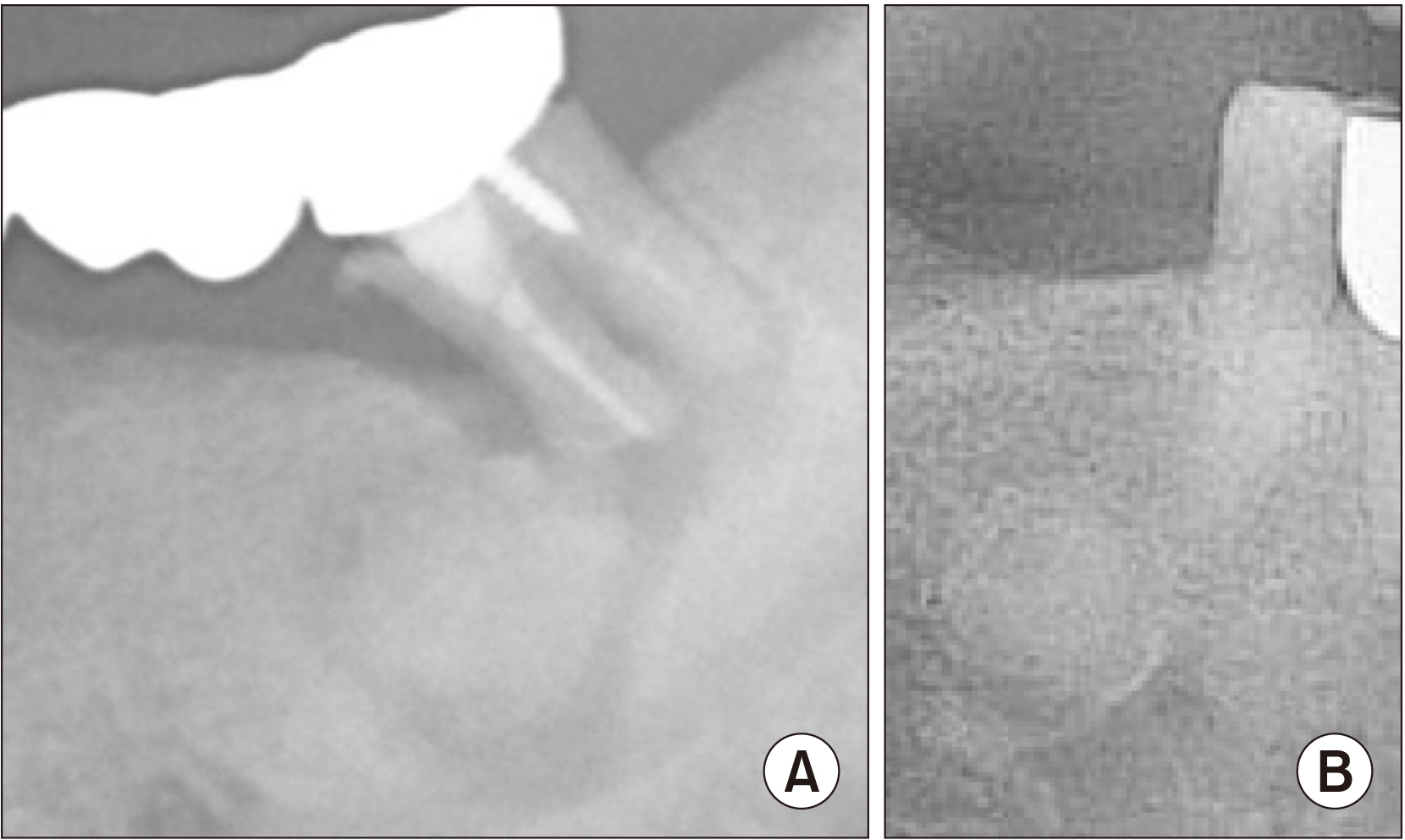
Cemento-osseous dysplasia: clinical presentation and symptoms
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Pusan National University, Yangsan, Korea
- KMID: 2529920
- DOI: http://doi.org/10.5125/jkaoms.2022.48.2.79
Abstract
Objectives
The purpose of this study was to evaluate risk factors and symptoms in cemento-osseous dysplasia (COD) patients.
Materials and Methods
In this study, 62 patients who were diagnosed histologically with COD were investigated from 2010 to 2020 at the author’s institution. We compared clinical and radiological characteristics of symptomatic and asymptomatic patients. The factors were sex, age, lesion size, site, radiologic stage of lesion, apical involvement, sign of infection, and history of tooth extraction. Statistical analysis was performed using Fisher’s exact test and the chi-square test.
Results
COD was more prevalent in female patients. With the exception of three cases, all were focal COD. The majority of patients presented with symptoms when the lesion was smaller than 1.5 cm in size. Symptoms were observed when the apex of the tooth was included in the lesion or there was a local infection around the lesion. The history of tooth extraction and previous endodontic treatment were evaluated, and history was not a significant predictor for the onset of symptoms.
Conclusion
In this study, risk factors associated with symptomatic patients were size of lesion, apical involvement, and local infection.
Keyword
Figure
Reference
-
References
1. Alsufyani NA, Lam EW. 2011; Osseous (cemento-osseous) dysplasia of the jaws: clinical and radiographic analysis. J Can Dent Assoc. 77:b70. PMID: 21683027.2. Mainville GN, Turgeon DP, Kauzman A. 2017; Diagnosis and management of benign fibro-osseous lesions of the jaws: a current review for the dental clinician. Oral Dis. 23:440–50. https://doi.org/10.1111/odi.12531. DOI: 10.1111/odi.12531. PMID: 27387498.
Article3. MacDonald DS. 2021; Classification and nomenclature of fibro-osseous lesions. Oral Surg Oral Med Oral Pathol Oral Radiol. 131:385–9. https://doi.org/10.1016/j.oooo.2020.12.004. DOI: 10.1016/j.oooo.2020.12.004. PMID: 33518490.
Article4. de Noronha Santos Netto J, Machado Cerri J, Miranda AM, Pires FR. 2013; Benign fibro-osseous lesions: clinicopathologic features from 143 cases diagnosed in an oral diagnosis setting. Oral Surg Oral Med Oral Pathol Oral Radiol. 115:e56–65. https://doi.org/10.1016/j.oooo.2012.05.022. DOI: 10.1016/j.oooo.2012.05.022. PMID: 22981804.
Article5. Kim NK, Kim HS, Kim J, Nam W, Cha IH, Kim HJ. 2011; Florid cemento-osseous dysplasia: a report of two cases. J Korean Assoc Oral Maxillofac Surg. 37:515–9. https://doi.org/10.5125/jkaoms.2011.37.6.515. DOI: 10.5125/jkaoms.2011.37.6.515. PMID: 34210933.
Article6. Nelson BL, Phillips BJ. 2019; Benign fibro-osseous lesions of the head and neck. Head Neck Pathol. 13:466–75. https://doi.org/10.1007/s12105-018-0992-5. DOI: 10.1007/s12105-018-0992-5. PMID: 30887390. PMCID: PMC6684826.
Article7. Brody A, Zalatnai A, Csomo K, Belik A, Dobo-Nagy C. 2019; Difficulties in the diagnosis of periapical translucencies and in the classification of cemento-osseous dysplasia. BMC Oral Health. 19:139. https://doi.org/10.1186/s12903-019-0843-0. DOI: 10.1186/s12903-019-0843-0. PMID: 31291935. PMCID: PMC6617922.
Article8. Kato CN, Barra SG, Pereira MJ, Gomes LT, Amaral TM, Abreu LG, et al. 2020; Mandibular radiomorphometric parameters of women with cemento-osseous dysplasia. Dentomaxillofac Radiol. 49:20190359. https://doi.org/10.1259/dmfr.20190359. DOI: 10.1259/dmfr.20190359. PMID: 31846355. PMCID: PMC7213529.
Article9. Mufeed A, Mangalath U, George A, Hafiz A. 2015; Infected florid osseous dysplasia: clinical and imaging follow-up. BMJ Case Rep. 2015:bcr2014209099. https://doi.org/10.1136/bcr-2014-209099. DOI: 10.1136/bcr-2014-209099. PMID: 25754168. PMCID: PMC4368933.
Article10. Olgac V, Sinanoglu A, Selvi F, Soluk-Tekkesin M. 2021; A clinicopathologic analysis of 135 cases of cemento-osseous dysplasia: to operate or not to operate? J Stomatol Oral Maxillofac Surg. 122:278–82. https://doi.org/10.1016/j.jormas.2020.06.002. DOI: 10.1016/j.jormas.2020.06.002. PMID: 32565263.
Article11. Kawai T, Hiranuma H, Kishino M, Jikko A, Sakuda M. 1999; Cemento-osseous dysplasia of the jaws in 54 Japanese patients: a radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 87:107–14. https://doi.org/10.1016/s1079-2104(99)70303-3. DOI: 10.1016/S1079-2104(99)70303-3. PMID: 9927089.
Article12. Cavalcanti PHP, Nascimento EHL, Pontual MLDA, Pontual ADA, Marcelos PGCL, Perez DEDC, et al. 2018; Cemento-osseous dysplasias: imaging features based on cone beam computed tomography scans. Braz Dent J. 29:99–104. https://doi.org/10.1590/0103-6440201801621. DOI: 10.1590/0103-6440201801621. PMID: 29267533.
Article13. Gumru B, Akkitap MP, Deveci S, Idman E. 2021; A retrospective cone beam computed tomography analysis of cemento-osseous dysplasia. J Dent Sci. 16:1154–61. https://doi.org/10.1016/j.jds.2021.03.009. DOI: 10.1016/j.jds.2021.03.009. PMID: 34484583. PMCID: PMC8403794.
Article14. Shibata N, Inamoto K, Naitoh M, Ariji E. 2021; Clinical assessment of cemento-osseous dysplasia based on three-dimensional diagnostic imaging: a case report. Aust Endod J. 47:105–12. https://doi.org/10.1111/aej.12488. DOI: 10.1111/aej.12488. PMID: 33523556.
Article15. Su L, Weathers DR, Waldron CA. 1997; Distinguishing features of focal cemento-osseous dysplasia and cemento-ossifying fibromas. II. A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 84:540–9. https://doi.org/10.1016/s1079-2104(97)90271-7. DOI: 10.1016/S1079-2104(97)90271-7. PMID: 9394387.
Article16. Ravikumar SS, Vasupradha G, Menaka TR, Sankar SP. 2020; Focal cemento-osseous dysplasia. J Oral Maxillofac Pathol. 24(Suppl 1):S19–22. https://doi.org/10.4103/jomfp.JOMFP_209_19. DOI: 10.4103/jomfp.JOMFP_209_19. PMID: 32189898. PMCID: PMC7069129.
Article17. Min CK, Koh KJ, Kim KA. 2018; Recurrent symptomatic cemento-osseous dysplasia: a case report. Imaging Sci Dent. 48:131–7. https://doi.org/10.5624/isd.2018.48.2.131. DOI: 10.5624/isd.2018.48.2.131. PMID: 29963485. PMCID: PMC6015922.
Article18. Kato CNAO, de Arruda JAA, Mendes PA, Neiva IM, Abreu LG, Moreno A, et al. 2020; Infected cemento-osseous dysplasia: analysis of 66 cases and literature review. Head Neck Pathol. 14:173–82. https://doi.org/10.1007/s12105-019-01037-x. DOI: 10.1007/s12105-019-01037-x. PMID: 31011984. PMCID: PMC7021850.
Article19. Günhan Ö, Kahraman D, Yalçın ÜK. 2021; The possible pathogenesis of cemento-osseous dysplasia: a case series and discussion. Adv Oral Maxillofac Surg. 3:100105. https://doi.org/10.1016/j.adoms.2021.100105. DOI: 10.1016/j.adoms.2021.100105.
Article20. Ray JM, Triplett RG. 2011; What is the role of biofilms in severe head and neck infections? Oral Maxillofac Surg Clin North Am. 23:497–505. https://doi.org/10.1016/j.coms.2011.07.002. DOI: 10.1016/j.coms.2011.07.002. PMID: 21982601.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 3 Types of Cemento-Osseous Dysplasia: Case Reports
- Cemento-Osseous Dysplasia Largely Occurring in the Mandible: Case Report
- Florid cemento-osseous dysplasia: a report of two cases
- Recurrent symptomatic cemento-osseous dysplasia: A case report
- CBCT findings of periapical cemento-osseous dysplasia: A case report