Healthc Inform Res.
2022 Apr;28(2):160-169. 10.4258/hir.2022.28.2.160.
Lockdowns, Community Mobility Patterns, and COVID-19: A Retrospective Analysis of Data from 16 Countries
- Affiliations
-
- 1Department of Community Medicine & Family Medicine, All India Institute of Medical Sciences, Gorakhpur, India
- 2Department of Community Medicine and School of Public Health, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- 3Institute of Statistical Research & Training, University of Dhaka, Dhaka, Bangladesh
- 4Department of Community Medicine, Vardhman Mahavir Medical College & Safdarjung Hospital, New Delhi, India
- KMID: 2529798
- DOI: http://doi.org/10.4258/hir.2022.28.2.160
Abstract
Objectives
During the coronavirus disease 2019 (COVID-19) pandemic, countries around the world framed specific laws and imposed varying degrees of lockdowns to ensure the maintenance of physical distancing. Understanding changes in temporal and spatial mobility patterns may provide insights into the dynamics of this infectious disease. Therefore, we assessed the efficacy of lockdown measures in 16 countries worldwide by analyzing the relationship between community mobility patterns and the doubling time of COVID-19.
Methods
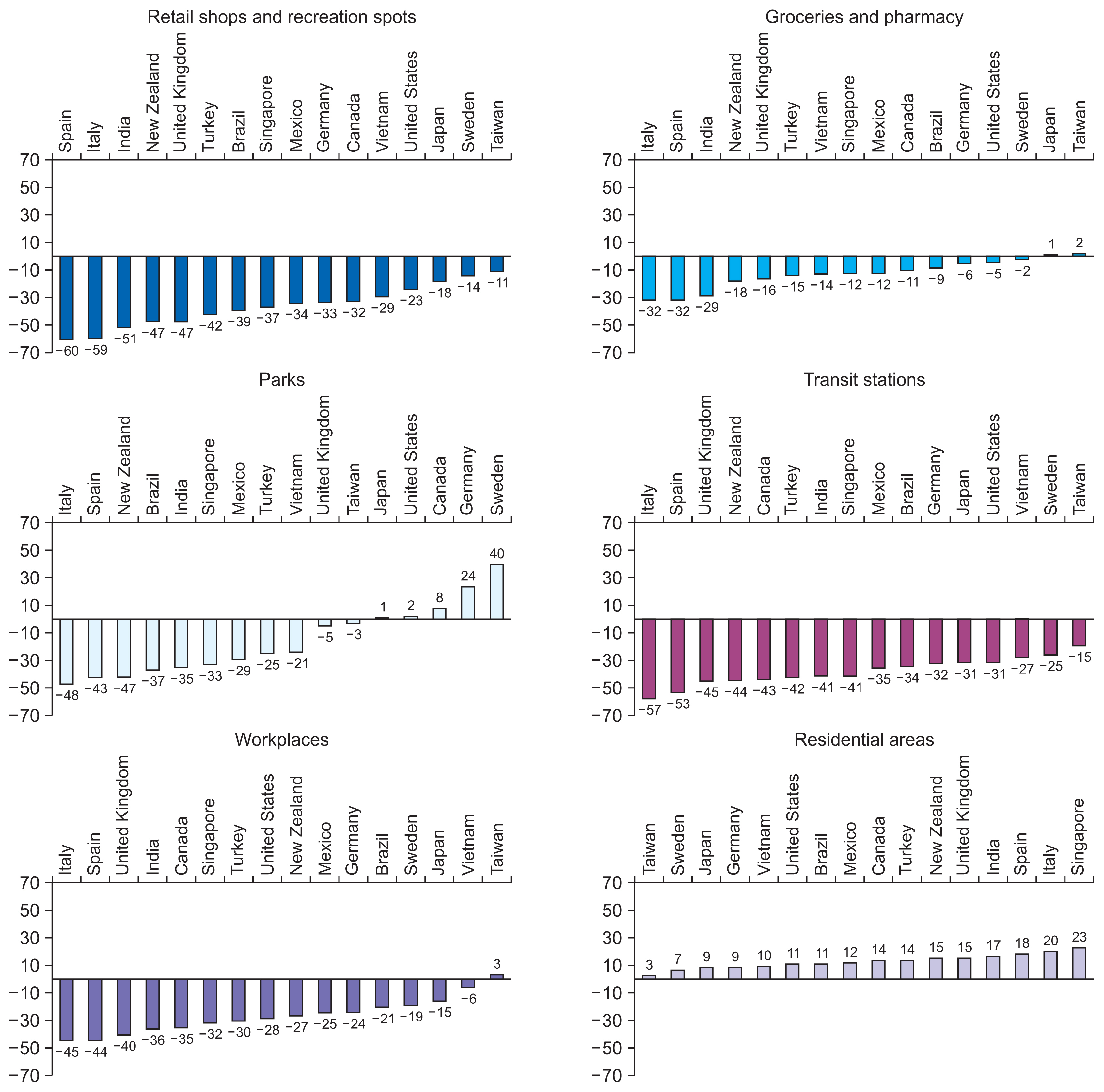
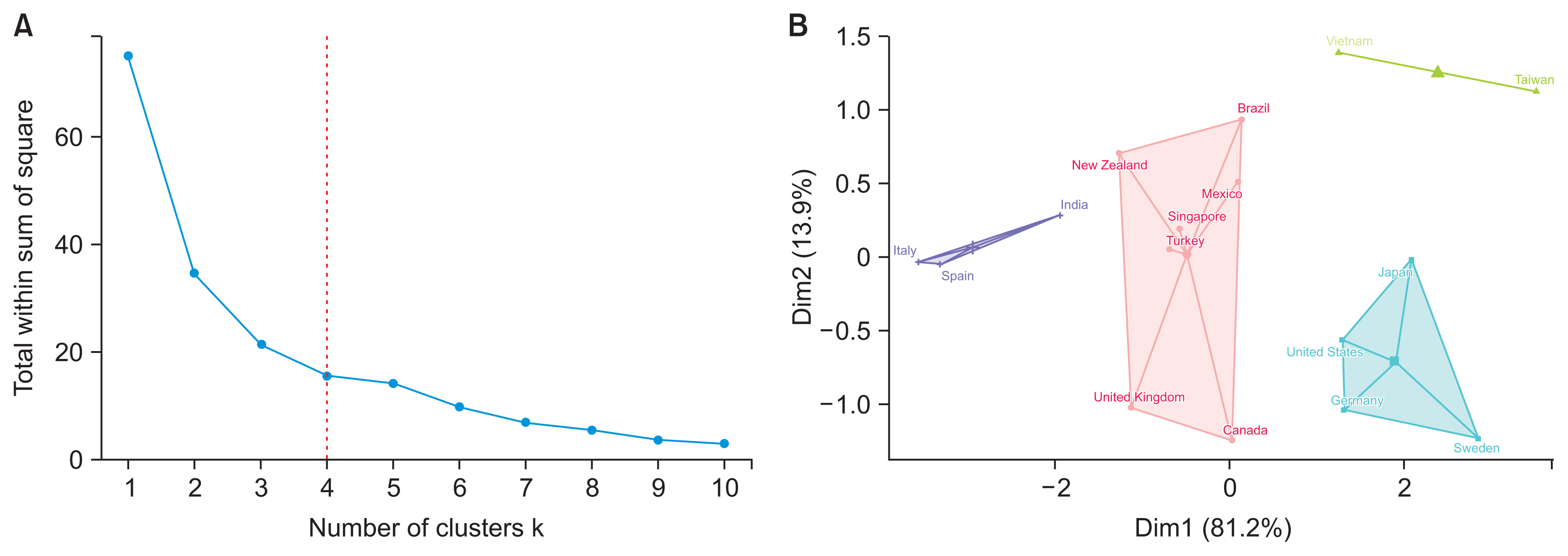
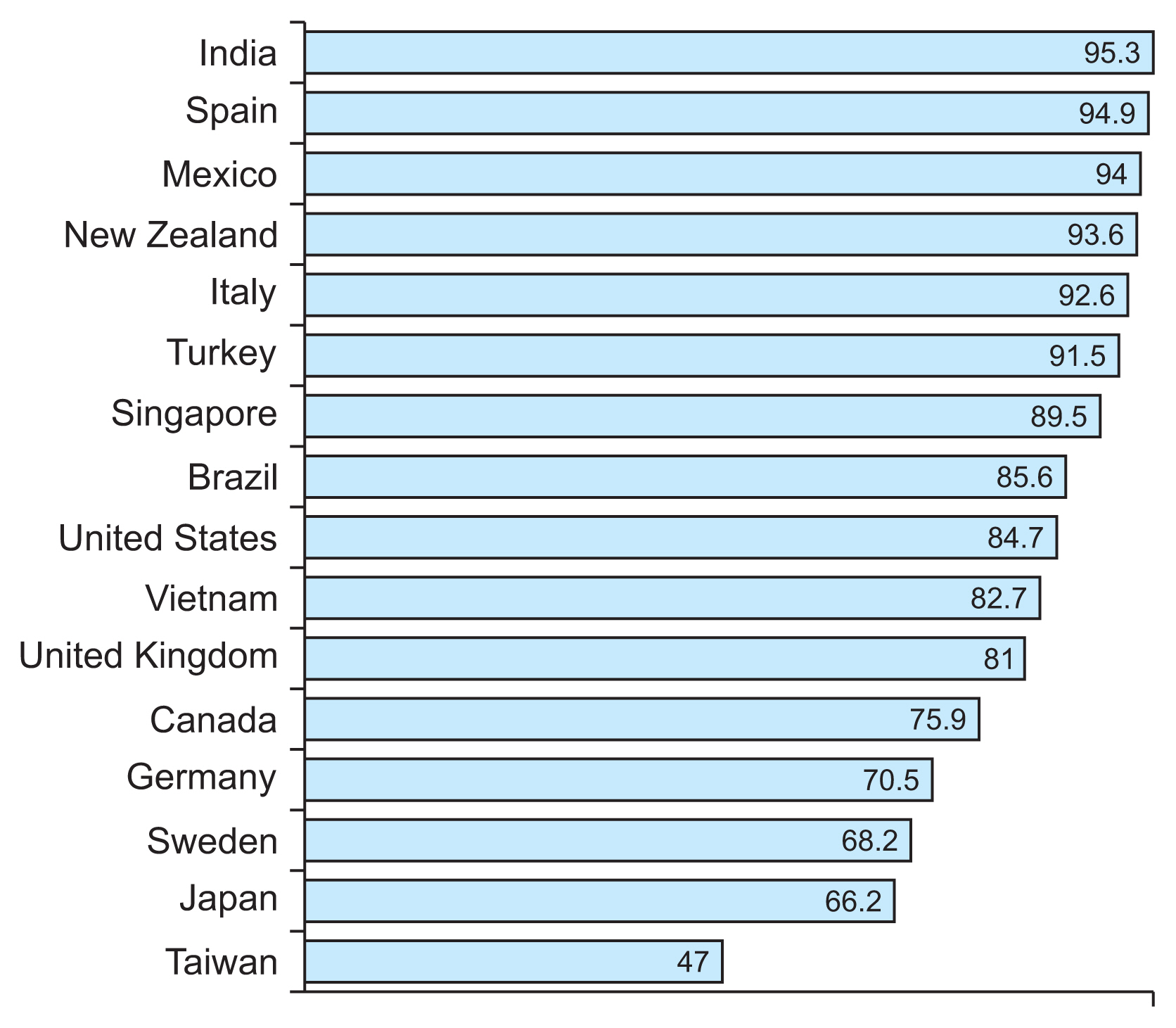
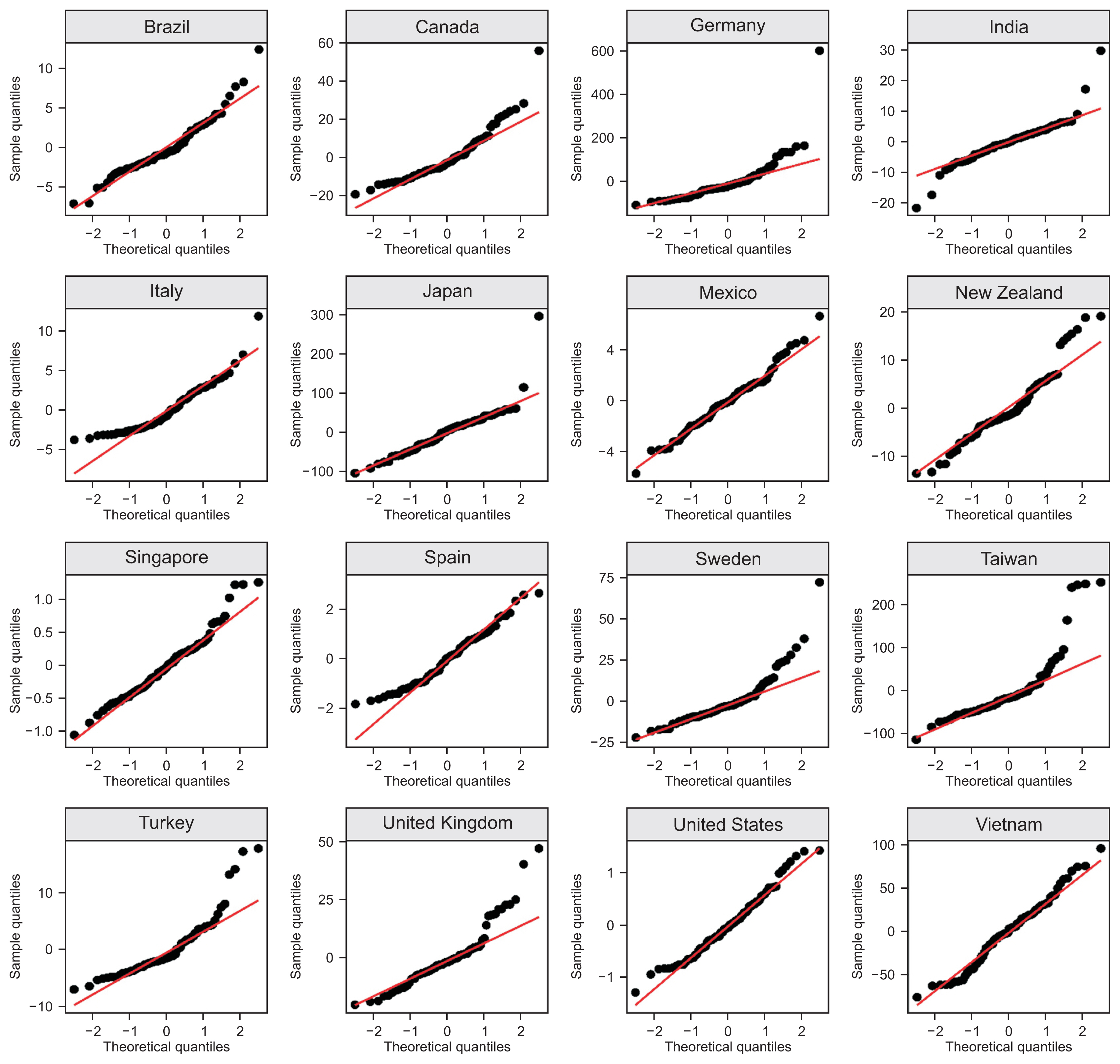
We performed a retrospective record-based analysis of population-level data on the doubling time for COVID-19 and community mobility. The doubling time for COVID-19 was calculated based on the laboratory-confirmed cases reported daily over the study period (from February 15 to May 2, 2020). Principal component analysis (PCA) of six mobility pattern-related variables was conducted. To explain the magnitude of the effect of mobility on the doubling time, a finite linear distributed lag model was fitted. The k-means clustering approach was employed to identify countries with similar patterns in the significant co-efficient of the mobility index, with the optimal number of clusters derived using Elbow’s method.
Results
The countries analyzed had reduced mobility in commercial and social places. Reduced mobility had a significant and favorable association with the doubling time of COVID-19—specifically, the greater the mobility reduction, the longer the time taken for the COVID-19 cases to double.
Conclusions
COVID-19 lockdowns achieved the immediate objective of mobility reduction in countries with a high burden of cases.
Keyword
Figure
Reference
-
References
1. World Health Organization. Coronavirus disease (COVID-19) technical guidance: Infection prevention and control/WASH [Internet]. Geneva, Switzerland: World Health Organization;2020. [cited at 2022 Apr 20]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control/ .2. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schunemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020; 395(10242):1973–87.
Article3. Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020; 585(7825):410–3.
Article4. Dore B. Covid-19: collateral damage of lockdown in India. BMJ. 2020; 369:m1711.
Article5. Lo KL, Zhang M, Chen Y, Mi JJ. Forecasting the trend of COVID-19 considering the impacts of public health interventions: an application of FGM and buffer level. J Healthc Inform Res. 2021; 5(4):497–528.
Article6. Chatterjee K, Chatterjee K, Kumar A, Shankar S. Healthcare impact of COVID-19 epidemic in India: a stochastic mathematical model. Med J Armed Forces India. 2020; 76(2):147–55.
Article7. Ngonghala CN, Iboi E, Eikenberry S, Scotch M, MacIntyre CR, Bonds MH, et al. Mathematical assessment of the impact of non-pharmaceutical interventions on curtailing the 2019 novel coronavirus. Math Biosci. 2020; 325:108364.
Article8. Google. COVID-19 community mobility report [Internet]. Mountain View (CA): Google;c2022. [cited at 2022 Apr 20]. Available from: https://www.google.com/covid19/mobility/ .9. Sun J, Kwek K, Li M, Shen H. Effects of social mobility and stringency measures on the COVID-19 outcomes: evidence from the United States. Front Public Health. 2021; 9:779501.
Article10. Periyasamy AG, Venkatesh U. Population mobility, lockdowns, and COVID-19 control: an analysis based on google location data and doubling time from India. Healthc Inform Res. 2021; 27(4):325–34.
Article11. Lu N, Cheng KW, Qamar N, Huang KC, Johnson JA. Weathering COVID-19 storm: successful control measures of five Asian countries. Am J Infect Control. 2020; 48(7):851–2.
Article12. Yang X. Does city lockdown prevent the spread of COVID-19?: new evidence from the synthetic control method. Glob Health Res Policy. 2021; 6(1):20.
Article13. Muniz-Rodriguez K, Chowell G, Cheung CH, Jia D, Lai PY, Lee Y, et al. Doubling time of the COVID-19 epidemic by province, China. Emerg Infect Dis. 2020; 26(8):1912–4.
Article14. Galvani AP, Lei X, Jewell NP. Severe acute respiratory syndrome: temporal stability and geographic variation in case-fatality rates and doubling times. Emerg Infect Dis. 2003; 9(8):991–4.
Article15. Wallinga J, Lipsitch M. How generation intervals shape the relationship between growth rates and reproductive numbers. Proc Biol Sci. 2007; 274(1609):599–604.
Article16. Blavatnik School of Government, University of Oxford. COVID-19 government response tracker [Internet]. Oxford, UK: University of Oxford;c2022. [cited 2022 Apr 20]. Available from: https://www.bsg.ox.ac.uk/research/research-projects/covid-19-government-response-tracker .17. Wold S, Esbensen K, Geladi P. Principal component analysis. Chemom Intell Lab Syst. 1987; 2(1–3):37–52.
Article18. Nelder JA, Wedderburn RW. Generalized linear models. J R Stat Soc Ser A. 1972; 135(3):370–84.
Article19. Bholowalia P, Kumar A. EBK-means: a clustering technique based on elbow method and k-means in WSN. Int J Comput Appl. 2014; 105(9):17–24.20. Tobias A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci Total Environ. 2020; 725:138539.21. Adiga A, Wang L, Sadilek A, Tendulkar A, Venkatramanan S, Vullikanti A, et al. Interplay of global multiscale human mobility, social distancing, government interventions, and COVID-19 dynamics. medRxiv [Preprint]. 2020. Jun. 5. [Epub]. https://doi.org/10.1101/2020.06.05.20123760 .
Article22. Rebecca Lai KK, Collins K. Which country has flattened the curve for the coronavirus? [Internet]. New York (NY): New York Times;2020. [cited at 2022 Apr 20]. Available from: https://www.nytimes.com/interactive/2020/03/19/world/coronavirus-flatten-the-curve-countries.html .23. Yeh S. The best global responses to COVID-19 pandemic, 1 year later [Internet]. New York (NY): Time USA LLC;2020. [cited at 2022 Apr 20]. Available from: https://time.com/5851633/best-global-responses-covid-19/ .24. Rocha R. What countries did right and wrong in responding to the pandemic [Internet]. Toronto, Canada: CBC News;2020. [cited at 2022 Apr 20]. Available from: https://www.cbc.ca/news/canada/covid-19-coronavirus-pandemic-countries-response-1.5617898 .25. Carrasco-Escobar G, Castro MC, Barboza JL, Ruiz-Cabrejos J, Llanos-Cuentas A, Vinetz JM, et al. Use of open mobile mapping tool to assess human mobility traceability in rural offline populations with contrasting malaria dynamics. PeerJ. 2019; 7:e6298.
Article26. Wesolowski A, Buckee CO, Engø-Monsen K, Metcalf CJE. Connecting mobility to infectious diseases: the promise and limits of mobile phone data. J Infect Dis. 2016; 214(suppl_4):S414–20.
Article27. Badr HS, Du H, Marshall M, Dong E, Squire MM, Gardner LM. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect Dis. 2020; 20(11):1247–54.
Article28. Voko Z, Pitter JG. The effect of social distance measures on COVID-19 epidemics in Europe: an interrupted time series analysis. Geroscience. 2020; 42(4):1075–82.
Article29. Delen D, Eryarsoy E, Davazdahemami B. No place like home: cross-national data analysis of the efficacy of social distancing during the COVID-19 pandemic. JMIR Public Health Surveill. 2020; 6(2):e19862.
Article30. Espinoza B, Castillo-Chavez C, Perrings C. Mobility restrictions for the control of epidemics: when do they work? PLoS One. 2020; 15(7):e0235731.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Population Mobility, Lockdowns, and COVID-19 Control: An Analysis Based on Google Location Data and Doubling Time from India
- In-depth Correlation Analysis of SARS-CoV-2 Effective Reproduction Number and Mobility Patterns: Three Groups of Countries
- Impact of Government Healthcare Policy Changes on Consumption and Human Movements During COVID-19: An Interrupted Time Series Analysis in Korea
- A Scoping Review on the Expected Role of Community Pharmacists in the Era of COVID-19 Pandemic Crisis Across OECD Countries
- Predisposing, Enabling, and Reinforcing Factors of COVID-19 Prevention Behavior in Indonesia: A Mixed-methods Study