Intest Res.
2022 Apr;20(2):192-202. 10.5217/ir.2020.00150.
Perspectives of East Asian patients and physicians on complementary and alternative medicine use for inflammatory bowel disease: results of a cross-sectional, multinational study
- Affiliations
-
- 1Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- 6Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 7Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 8Department of Internal Medicine, Keio University School of Medicine, Tokyo, Japan
- 9Inflammatory Bowel Disease Center, Fukuoka University Chikushi Hospital, Chikushino, Japan
- 10Endoscopic Unit, Tokyo Medical and Dental University Hospital, Tokyo, Japan
- 11Department of Internal Medicine, Peking Union Medical College Hospital, Beijing, China
- 12Gastroenterology Department, Sir Run Run Shaw Hospital, Zhejiang University College of Medicine, Zhejiang, China
- KMID: 2529565
- DOI: http://doi.org/10.5217/ir.2020.00150
Abstract
- Background/Aims
Complementary and alternative medicine (CAM) is prevalent in East Asia. However, information on CAM in East Asian patients with inflammatory bowel disease (IBD) is scarce. We aimed to profile the prevalence and pattern of CAM use among East Asian IBD patients and to identify factors associated with CAM use. We also compared physicians’ perspectives on CAM.
Methods
Patients with IBD from China, Japan, and South Korea were invited to complete questionnaires on CAM use. Patient demographic and clinical data were collected. Logistic regression analysis was applied for predictors of CAM use. Physicians from each country were asked about their opinion on CAM services or products.
Results
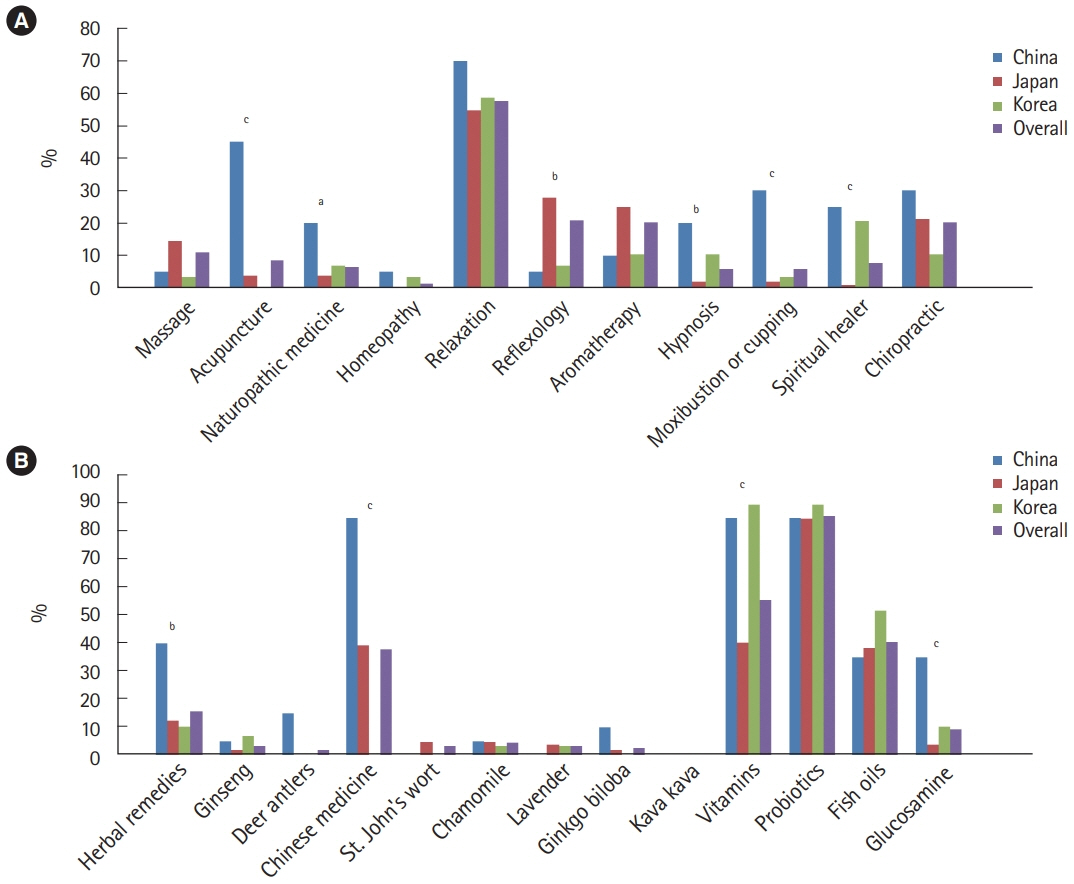
Overall, 905 patients with IBD participated in this study (China 232, Japan 255, and South Korea 418). Approximately 8.6% of patients with IBD used CAM services for their disease, while 29.7% of patients sought at least 1 kind of CAM product. Current active disease and Chinese or South Korean nationality over Japanese were independent predictors of CAM use. Chinese doctors were more likely to consider CAM helpful for patients with IBD than were Japanese and South Korean doctors.
Conclusions
In 8.6% and 29.7% of East Asian patients with IBD used CAM services and products, respectively, which does not differ from the prevalence in their Western counterparts. There is a significant gap regarding CAM usage among different Asian countries, not only from the patients’ perspective but also from the physicians’ point of view.
Figure
Reference
-
1. Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017; 152:313–321.
Article2. Toruner M, Loftus EV Jr, Harmsen WS, et al. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology. 2008; 134:929–936.
Article3. Lichtenstein GR, Rutgeerts P, Sandborn WJ, et al. A pooled analysis of infections, malignancy, and mortality in infliximaband immunomodulator-treated adult patients with inflammatory bowel disease. Am J Gastroenterol. 2012; 107:1051–1063.
Article4. Papamichael K, Gils A, Rutgeerts P, et al. Role for therapeutic drug monitoring during induction therapy with TNF antagonists in IBD: evolution in the definition and management of primary nonresponse. Inflamm Bowel Dis. 2015; 21:182–197.
Article5. Cheifetz AS, Gianotti R, Luber R, Gibson PR. Complementary and alternative medicines used by patients with inflammatory bowel diseases. Gastroenterology. 2017; 152:415–429.
Article6. Hilsden RJ, Verhoef MJ, Best A, Pocobelli G. Complementary and alternative medicine use by Canadian patients with inflammatory bowel disease: results from a national survey. Am J Gastroenterol. 2003; 98:1563–1568.
Article7. Li FX, Verhoef MJ, Best A, Otley A, Hilsden RJ. Why patients with inflammatory bowel disease use or do not use complementary and alternative medicine: a Canadian national survey. Can J Gastroenterol. 2005; 19:567–573.
Article8. Nguyen GC, Croitoru K, Silverberg MS, Steinhart AH, Weizman AV. Use of complementary and alternative medicine for inflammatory bowel disease is associated with worse adherence to conventional therapy: the COMPLIANT Study. Inflamm Bowel Dis. 2016; 22:1412–1417.
Article9. Rawsthorne P, Clara I, Graff LA, et al. The Manitoba Inflammatory Bowel Disease Cohort Study: a prospective longitudinal evaluation of the use of complementary and alternative medicine services and products. Gut. 2012; 61:521–527.
Article10. Gallinger ZR, Nguyen GC. Practices and attitudes toward complementary and alternative medicine in inflammatory bowel disease: a survey of gastroenterologists. J Complement Integr Med. 2014; 11:297–303.
Article11. Hung A, Kang N, Bollom A, Wolf JL, Lembo A. Complementary and alternative medicine use is prevalent among patients with gastrointestinal diseases. Dig Dis Sci. 2015; 60:1883–1888.
Article12. Mannel M. Drug interactions with St John’s wort: mechanisms and clinical implications. Drug Saf. 2004; 27:773–797.13. Cheung F. TCM: made in China. Nature. 2011; 480:S82–S83.
Article14. Harris PE, Cooper KL, Relton C, Thomas KJ. Prevalence of complementary and alternative medicine (CAM) use by the general population: a systematic review and update. Int J Clin Pract. 2012; 66:924–939.
Article15. Jowett SL, Seal CJ, Phillips E, Gregory W, Barton JR, Welfare MR. Defining relapse of ulcerative colitis using a symptombased activity index. Scand J Gastroenterol. 2003; 38:164–171.
Article16. Best WR. Predicting the Crohn’s disease activity index from the Harvey-Bradshaw index. Inflamm Bowel Dis. 2006; 12:304–310.
Article17. Bensoussan M, Jovenin N, Garcia B, et al. Complementary and alternative medicine use by patients with inflammatory bowel disease: results from a postal survey. Gastroenterol Clin Biol. 2006; 30:14–23.
Article18. Weizman AV, Ahn E, Thanabalan R, et al. Characterisation of complementary and alternative medicine use and its impact on medication adherence in inflammatory bowel disease. Aliment Pharmacol Ther. 2012; 35:342–349.
Article19. Portela F, Dias CC, Caldeira P, et al. The who-when-why triangle of CAM use among Portuguese IBD patients. Dig Liver Dis. 2017; 49:388–396.20. Abitbol V, Lahmek P, Buisson A, et al. Impact of complementary and alternative medicine on the quality of life in inflammatory bowel disease: results from a French national survey. Eur J Gastroenterol Hepatol. 2014; 26:288–294.
Article21. Joos S, Rosemann T, Szecsenyi J, Hahn EG, Willich SN, Brinkhaus B. Use of complementary and alternative medicine in Germany: a survey of patients with inflammatory bowel disease. BMC Complement Altern Med. 2006; 6:19.22. Langhorst J, Anthonisen IB, Steder-Neukamm U, et al. Patterns of complementary and alternative medicine (CAM) use in patients with inflammatory bowel disease: perceived stress is a potential indicator for CAM use. Complement Ther Med. 2007; 15:30–37.
Article23. Park DI, Cha JM, Kim HS, et al. Predictive factors of complementary and alternative medicine use for patients with inflammatory bowel disease in Korea. Complement Ther Med. 2014; 22:87–93.
Article24. Lee SH, Chang K, Seo KS, et al. Changes in prevalence and perception of complementary and alternative medicine use in Korean inflammatory bowel disease patients: results of an 8-year follow-up survey. Intest Res. 2020; 18:192–199.
Article25. Leong RW, Lawrance IC, Ching JY, et al. Knowledge, quality of life, and use of complementary and alternative medicine and therapies in inflammatory bowel disease: a comparison of Chinese and Caucasian patients. Dig Dis Sci. 2004; 49:1672–1676.
Article26. Stadlbauer V, Fickert P, Lackner C, et al. Hepatotoxicity of NONI juice: report of two cases. World J Gastroenterol. 2005; 11:4758–4760.
Article27. Pittler MH, Ernst E. Systematic review: hepatotoxic events associated with herbal medicinal products. Aliment Pharmacol Ther. 2003; 18:451–471.
Article28. Park HL, Lee HS, Shin BC, et al. Traditional medicine in china, Korea, and Japan: a brief introduction and comparison. Evid Based Complement Alternat Med. 2012; 2012:429103.
Article29. Torres J, Ellul P, Langhorst J, et al. European Crohn’s and Colitis Organisation topical review on complementary medicine and psychotherapy in inflammatory bowel disease. J Crohns Colitis. 2019; 13:673–685e.
Article30. Langhorst J, Wulfert H, Lauche R, et al. Systematic review of complementary and alternative medicine treatments in inflammatory bowel diseases. J Crohns Colitis. 2015; 9:86–106.
Article31. Norton C, Czuber-Dochan W, Artom M, Sweeney L, Hart A. Systematic review: interventions for abdominal pain management in inflammatory bowel disease. Aliment Pharmacol Ther. 2017; 46:115–125.
Article32. Koning M, Ailabouni R, Gearry RB, Frampton CM, Barclay ML. Use and predictors of oral complementary and alternative medicine by patients with inflammatory bowel disease: a population-based, case-control study. Inflamm Bowel Dis. 2013; 19:767–778.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
- Patterns of Complementary and Alternative Medicine Therapies in Patients with Chronic Fatigue or Pain
- Asian Physician's Perspectives on Biosimilars in Inflammatory Bowel Disease: Are We Ready to Use?
- Diagnosis of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization for Crohn's and Colitis (AOCC) meeting in Seoul
- Vaccination in patients with inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting