Korean J Gastroenterol.
2022 Apr;79(4):177-181. 10.4166/kjg.2022.006.
A Huge Malignant Gastric Gastrointestinal Stromal Tumor in a Young Patient
- Affiliations
-
- 1Departments of Internal Medicine, Pathology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Departments of Pathology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 3Departments of Surgery, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2529368
- DOI: http://doi.org/10.4166/kjg.2022.006
Abstract
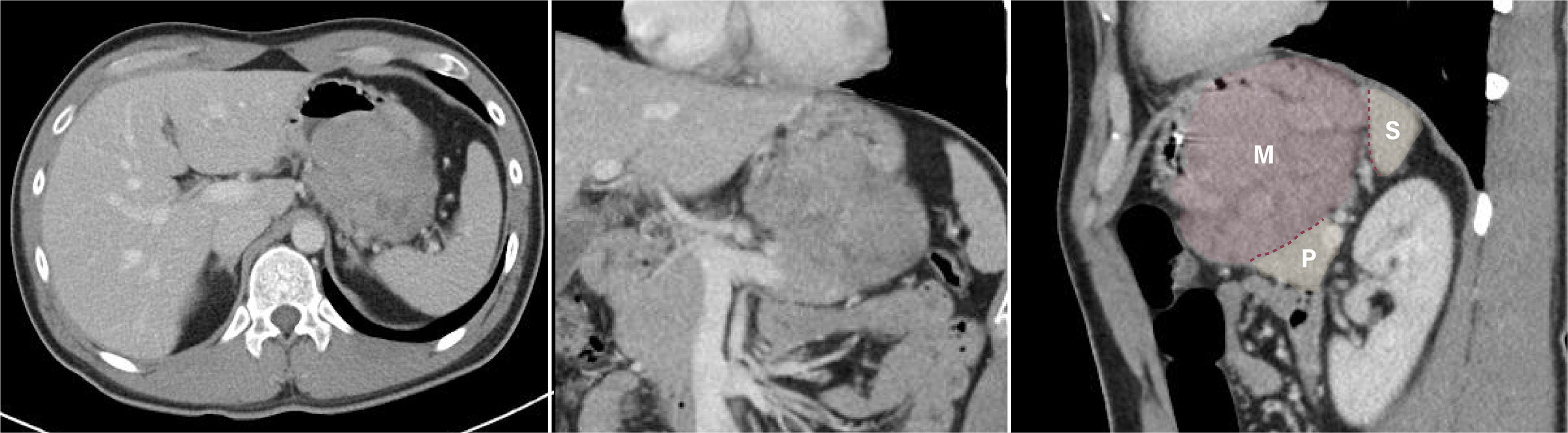
- Malignant gastrointestinal stromal tumors (GISTs) are rare neoplasms originating from the gastrointestinal tract that rarely occur in patients below 40 years of age. To our knowledge, there have been no previous reports of satellite and metastatic nodules in GIST. We present a case of a young patient with a huge malignant gastric GIST accompanied by spontaneous bleeding and satellite and metastatic nodules, successfully treated surgically, without preoperative chemotherapy administration. A 28-year-old man was admitted to Haeundae Paik Hospital with melena. A huge bulging gastric mass with ulceration and bleeding was observed on endoscopy. A subepithelial lesion on the stomach body, abutting the pancreatic body and tail, with regional lymph node enlargement was confirmed by EUS and CT. Radical total gastrectomy was performed, the invasion surrounding the pancreatic tail and spleen were surgically dissected, and enlarged lymph nodes around the celiac trunk and the common hepatic artery were removed. The pathology results showed a malignant GIST with two satellite nodules and a metastatic tumor nodule at the left paracardial lymph node site. After complete resection of the malignant GIST, adjuvant chemotherapy with imatinib was initiated. Follow-up CT and endoscopy performed 6 months after surgery confirmed no recurrence of the disease.
Keyword
Figure
Reference
-
1. Miettinen M, Lasota J. 2001; Gastrointestinal stromal tumors--definition, clinical, histological, immunohistochemical, and molecular g endothelial features and differential diagnosis. Virchows Arch. 438:1–12. DOI: 10.1007/s004280000338. PMID: 11213830.
Article2. Tran T, Davila JA, El-Serag HB. 2005; The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol. 100:162–168. DOI: 10.1111/j.1572-0241.2005.40709.x. PMID: 15654796.
Article3. Sorour MA, Kassem MI, Ghazal Ael-H, El-Riwini MT, Abu Nasr A. 2014; Gastrointestinal stromal tumors (GIST) related emergencies. Int J Surg. 12:269–280. DOI: 10.1016/j.ijsu.2014.02.004. PMID: 24530605.
Article4. Pih GY, Jeon SJ, Ahn JY, et al. 2020; Clinical outcomes of upper gastrointestinal bleeding in patients with gastric gastrointestinal stromal tumor. Surg Endosc. 34:696–706. DOI: 10.1007/s00464-019-06816-9. PMID: 31062158.
Article5. Agaimy A, Wünsch PH. 2009; Lymph node metastasis in gastrointestinal stromal tumours (GIST) occurs preferentially in young patients < or = 40 years: an overview based on our case material and the literature. Langenbecks Arch Surg. 394:375–381. DOI: 10.1007/s00423-008-0449-5. PMID: 19104826.
Article6. Kosmidis CS, Alexandrou V, Koimtzis GD, et al. 2020; Treatment of a gastrointestinal stromal tumor (GIST) Adherent to the spleen and the tail of the pancreas: a case report. Am J Case Rep. 21:e918278. DOI: 10.12659/AJCR.918278. PMID: 32231176. PMCID: PMC7161921.
Article7. Kong SH, Yang HK. 2013; Surgical treatment of gastric gastrointestinal stromal tumor. J Gastric Cancer. 13:3–18. DOI: 10.5230/jgc.2013.13.1.3. PMID: 23610714. PMCID: PMC3627804.
Article8. Canda AE, Ozsoy Y, Nalbant OA, Sagol O. 2008; Gastrointestinal stromal tumor of the stomach with lymph node metastasis. World J Surg Oncol. 6:97. DOI: 10.1186/1477-7819-6-97. PMID: 18775061. PMCID: PMC2553079.
Article9. Miettinen M, Lasota J. 2013; Gastrointestinal stromal tumors. Gastroenterol Clin North Am. 42:399–415. DOI: 10.1016/j.gtc.2013.01.001. PMID: 23639648. PMCID: PMC3644178.
Article10. Koo DH, Ryu MH, Kim KM, et al. 2016; Asian consensus guidelines for the diagnosis and management of gastrointestinal stromal tumor. Cancer Res Treat. 48:1155–1166. DOI: 10.4143/crt.2016.187. PMID: 27384163. PMCID: PMC5080813.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Advanced Gastric Carcinoma Mimicking a Malignant Gastrointestinal Stromal Tumor
- Malignant Transformation of Gastric Gastrointestinal Stromal Tumor in 44 Months Observational Period: A Case Report
- A case of huge Gastrointestinal stromal tumor masquerading as an ovarian malignancy
- Giant Gastrointestinal Stromal Tumor Accompanying Stomach Cancer
- Partial gastric outlet obstruction caused by a huge submucosal tumor originating in the heterotopic pancreas