Cancer Res Treat.
2022 Apr;54(2):621-629. 10.4143/crt.2021.483.
A Prognostic Model to Facilitate Palliative Care Referral in Oncology Outpatients
- Affiliations
-
- 1Division of Hematology and Medical Oncology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Department of Palliative Medicine, Tohoku University School of Medicine, Sendai, Japan
- 3Hospice & Palliative Care Center, Department of Family Medicine, Dongguk University Ilsan Hospital, Goyang, Korea
- 4Department of Medicine, Dongguk University Medical School, Seoul, Korea
- 5Division of Medical Oncology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 6Division of Medical Oncology, Department of Internal Medicine, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea
- 7Department of Statistics, Dongguk University Medical School, Seoul, Korea
- KMID: 2528231
- DOI: http://doi.org/10.4143/crt.2021.483
Abstract
- Purpose
We aimed to develop a prognostic model to assist palliative care referral at least 3 months before death in advanced cancer patients treated at an outpatient medical oncology clinic.
Materials and Methods
In this prospective cohort study, a total of 200 patients were enrolled at a tertiary cancer center in South Korea. The major eligibility criterion was an expected survival of less than a year as estimated by their oncologists. We analyzed the influences of known prognostic factors along with chemotherapy status, mid-arm circumference, and triceps skinfold thickness on survival time.
Results
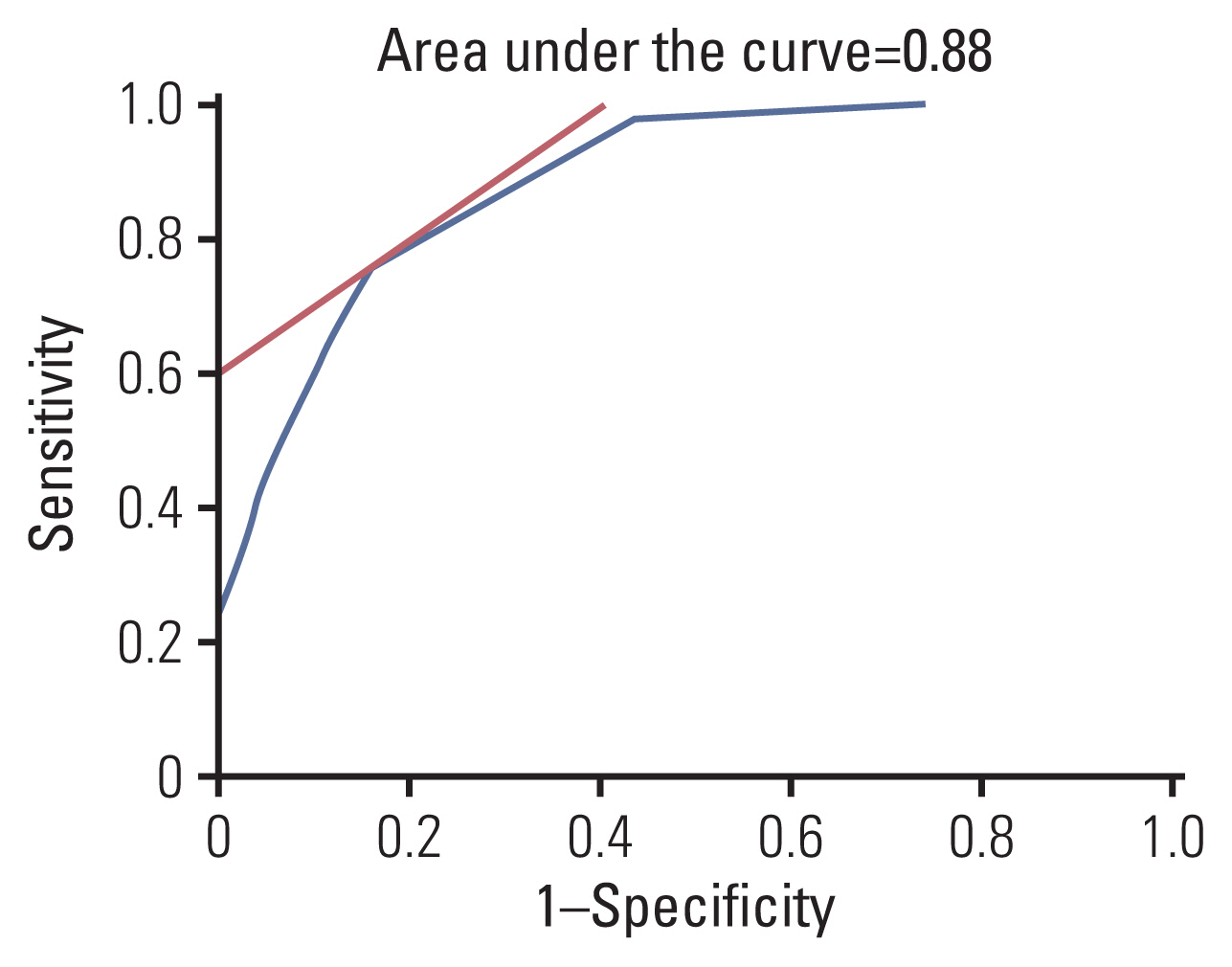
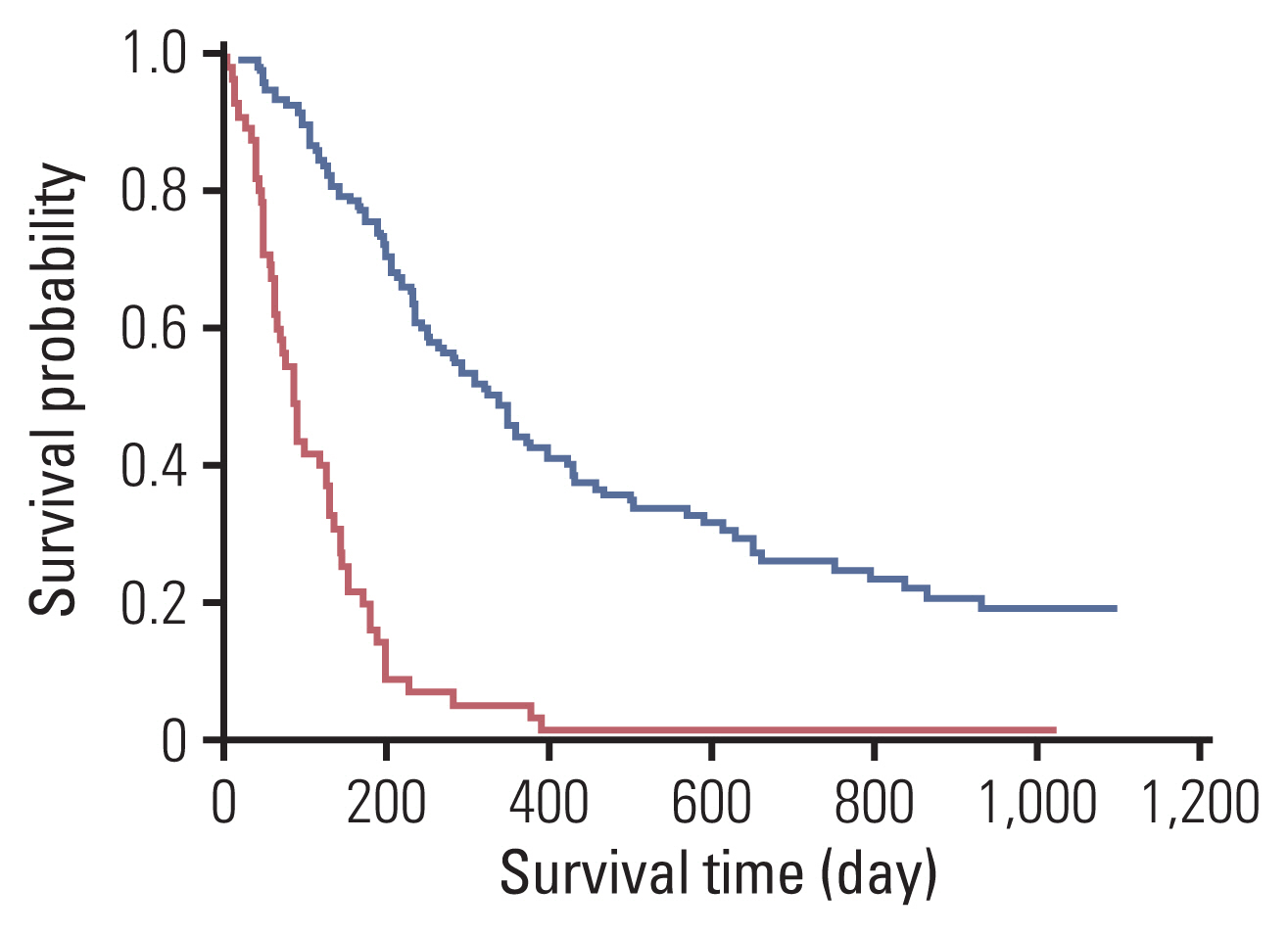
The mean age of the patients was 64.5 years, 36% were female, and the median survival time was 7.6 months. In the multivariate analysis, we found 6 significant factors related to poor survival: a poor Eastern Cooperative Oncology Group (ECOG) performance status (≥2), not undergoing chemotherapy, anorexia, a low lymphocyte level (<12%), a high lactate dehydrogenase (LDH) level (≥300 IU/L), and a low mid-arm circumference (<23 cm). We developed a prognostic model (score, 0-8.0) to predict 3-month survival based on the multivariate analysis. Patients who scored ≥4.0 points had a short survival of less than 3 months (p<0.001). The discriminating ability of the prognostic model using the area under the receiver operating characteristic curve (AUC) was 0.88.
Conclusion
The prognostic model using ECOG performance status, chemotherapy status, anorexia, lymphocytes, LDH, and mid-arm circumference can predict 3-month survival in medical oncology outpatients. It can alert oncologists to refer patients to palliative care specialists before it is too late.
Keyword
Figure
Reference
-
References
1. Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA. 2009; 302:741–9.
Article2. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010; 363:733–42.
Article3. Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014; 383:1721–30.
Article4. Ferrell BR, Temel JS, Temin S, Alesi ER, Balboni TA, Basch EM, et al. Integration of palliative care Into standard oncology vare: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017; 35:96–112.
Article5. NHPCO facts and figures [Internet]. Alexandria, VA: National Hospice and Palliative Care Organization;2020. [cited 2020 Nov 29]. Available from: https://www.nhpco.org/wp-content/uploads/NHPCO-Facts-Figures-2020-edition.pdf .6. Hospice UK. Hospice care in the UK [Internet]. London: Hospice UK;2016. [cited 2020 Nov 29]. Available from: https://www.hospiceuk.org/docs/default-source/What-We-Offer/publications-documents-and-files/hospice-care-in-the-uk-2016.pdf?sfvrsn=0 .7. National Cancer Center. Hospice and Palliative Care [Internet]. Goyang: National Cancer Center;2020. [cited 2020 Nov 29]. Available from: http://hospice.cancer.go.kr/pain/stat.do?menu_no=634&brd_mgrno= .8. Dalal S, Bruera S, Hui D, Yennu S, Dev R, Williams J, et al. Use of palliative care services in a tertiary cancer center. Oncologist. 2016; 21:110–8.
Article9. Hui D, Kim SH, Kwon JH, Tanco KC, Zhang T, Kang JH, et al. Access to palliative care among patients treated at a comprehensive cancer center. Oncologist. 2012; 17:1574–80.
Article10. Hui D, Kim SH, Roquemore J, Dev R, Chisholm G, Bruera E. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer. 2014; 120:1743–9.
Article11. Hui D, Kilgore K, Park M, Liu D, Kim YJ, Park JC, et al. Pattern and predictors of outpatient palliative care referral among thoracic medical oncologists. Oncologist. 2018; 23:1230–5.
Article12. Petrillo LA, El-Jawahri A, Nipp RD, Lichtenstein MR, Durbin SM, Reynolds KL, et al. Performance status and end-of-life care among adults with non-small cell lung cancer receiving immune checkpoint inhibitors. Cancer. 2020; 126:2288–95.
Article13. Bruera E, Hui D. Conceptual models for integrating palliative care at cancer centers. J Palliat Med. 2012; 15:1261–9.
Article14. Cho JH, Yan US. Standard values for nutritional assessment by anthropometry in healthy Korean adults. Korean J Med. 1999; 56:560–8.15. Kruser TJ, Kruser JM, Gross JP, Moran M, Kaiser K, Szmuilowicz E, et al. Medical oncologist perspectives on palliative care reveal physician-centered barriers to early integration. Ann Palliat Med. 2020; 9:2800–8.
Article16. Ehrlich BS, Movsisyan N, Batmunkh T, Kumirova E, Borisevich MV, Kirgizov K, et al. Barriers to the early integration of palliative care in pediatric oncology in 11 Eurasian countries. Cancer. 2020; 126:4984–93.
Article17. Anderson F, Downing GM, Hill J, Casorso L, Lerch N. Palliative performance scale (PPS): a new tool. J Palliat Care. 1996; 12:5–11.
Article18. Pirovano M, Maltoni M, Nanni O, Marinari M, Indelli M, Zaninetta G, et al. A new palliative prognostic score: a first step for the staging of terminally ill cancer patients. Italian Multicenter and Study Group on Palliative Care. J Pain Symptom Manage. 1999; 17:231–9.19. Morita T, Tsunoda J, Inoue S, Chihara S. The Palliative Prognostic Index: a scoring system for survival prediction of terminally ill cancer patients. Support Care Cancer. 1999; 7:128–33.
Article20. Suh SY, Choi YS, Shim JY, Kim YS, Yeom CH, Kim D, et al. Construction of a new, objective prognostic score for terminally ill cancer patients: a multicenter study. Support Care Cancer. 2010; 18:151–7.
Article21. Glare PA, Eychmueller S, McMahon P. Diagnostic accuracy of the palliative prognostic score in hospitalized patients with advanced cancer. J Clin Oncol. 2004; 22:4823–8.
Article22. Tassinari D, Montanari L, Maltoni M, Ballardini M, Piancastelli A, Musi M, et al. The palliative prognostic score and survival in patients with advanced solid tumors receiving chemotherapy. Support Care Cancer. 2008; 16:359–70.
Article23. Barbot AC, Mussault P, Ingrand P, Tourani JM. Assessing 2-month clinical prognosis in hospitalized patients with advanced solid tumors. J Clin Oncol. 2008; 26:2538–43.
Article24. Chow E, Abdolell M, Panzarella T, Harris K, Bezjak A, Warde P, et al. Predictive model for survival in patients with advanced cancer. J Clin Oncol. 2008; 26:5863–9.
Article25. Tredan O, Ray-Coquard I, Chvetzoff G, Rebattu P, Bajard A, Chabaud S, et al. Validation of prognostic scores for survival in cancer patients beyond first-line therapy. BMC Cancer. 2011; 11:95.
Article26. Bourgeois H, Grude F, Solal-Celigny P, Dupuis O, Voog E, Ganem G, et al. Clinical validation of a prognostic tool in a population of outpatients treated for incurable cancer undergoing anticancer therapy: PRONOPALL study. Ann Oncol. 2017; 28:1612–7.
Article27. Paiva CE, Paiva BS, de Paula Pantano N, Preto DD, de Oliveira CZ, Yennurajalingam S, et al. Development and validation of a prognostic nomogram for ambulatory patients with advanced cancer. Cancer Med. 2018; 7:3003–10.
Article28. Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013; 31:1539–47.
Article29. Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Decreased muscle mass and increased central adiposity are independently related to mortality in older men. Am J Clin Nutr. 2007; 86:1339–46.
Article30. Soler-Cataluna JJ, Sanchez-Sanchez L, Martinez-Garcia MA, Sanchez PR, Salcedo E, Navarro M. Mid-arm muscle area is a better predictor of mortality than body mass index in COPD. Chest. 2005; 128:2108–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Barriers to Early Palliative Care
- Doctor's Perception and Referral Barriers toward Palliative Care for Advanced Cancer Patients
- Hospice and Palliative Care for Patients in the Intensive Care Unit: Current Status in Countries Other than Korea
- Changes of End of Life Practices for Cancer Patients and TheirAssociation with Hospice Palliative Care Referral over 2009-2014:A Single Institution Study
- Understanding of Changes to Hospice & Palliative Care Brought by the Enforcement of the Act on Hospice & Palliative Care and Dying Patient Determination of Life Sustaining Treatments