Acute Crit Care.
2022 Feb;37(1):53-60. 10.4266/acc.2021.01389.
Association between the National Health Insurance coverage benefit extension policy and clinical outcomes of ventilated patients: a retrospective study
- Affiliations
-
- 1Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Pusan National University Hospital, Busan, Korea
- 2Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea
- KMID: 2527907
- DOI: http://doi.org/10.4266/acc.2021.01389
Abstract
- Background
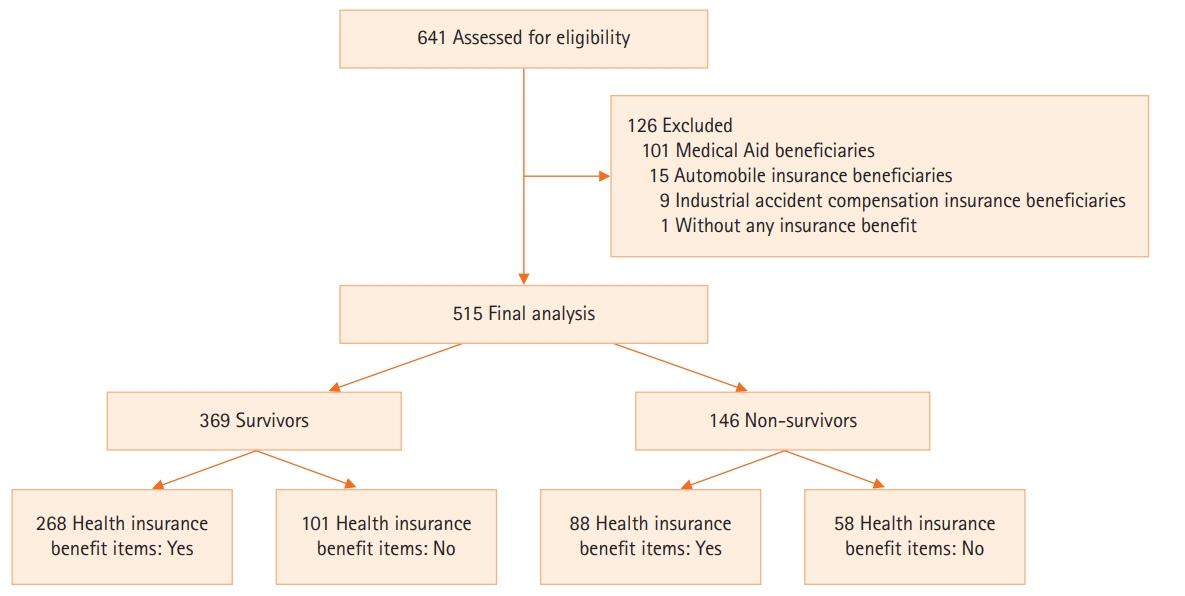
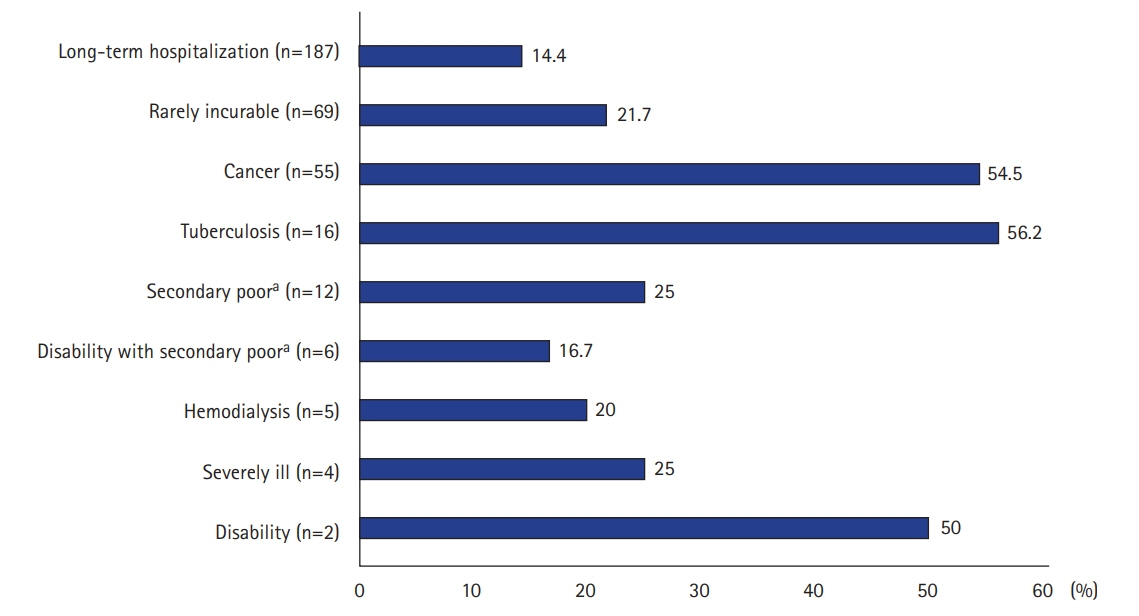
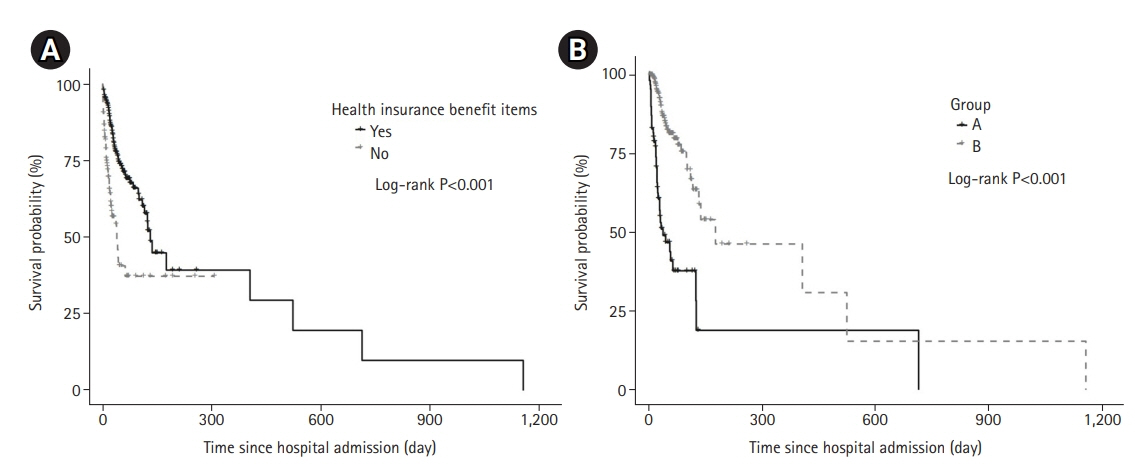
This study aimed to investigate the association between the Korean National Health Insurance coverage benefit extension policy and clinical outcomes of patients who were ventilated owing to various respiratory diseases. Methods: Data from 515 patients (male, 69.7%; mean age, 69.8±12.1 years; in-hospital mortality rate, 28.3%) who were hospitalized in a respiratory intensive care unit were retrospectively analyzed over 5 years. Results: Of total enrolled patients, 356 (69.1%) had one benefit items under this policy during their hospital stay. They had significantly higher medical expenditure (total: median, 23,683 vs. 12,742 U.S. dollars [USD], P<0.001), out-of-pocket (median, 5,932 vs. 4,081 USD; P<0.001), and a lower percentage of out-of-pocket medical expenditure relative to total medical expenditure (median, 26.0% vs. 32.2%; P<0.001). Patients without benefit items associated with higher in-hospital mortality (hazard ratio [HR], 2.794; 95% confidence interval [CI], 1.980–3.941; P<0.001). In analysis of patients with benefit items, patients with three items (“cancer,” “tuberculosis,” and “disability”) had significantly lower out-of-pocket medical expenditure (3,441 vs. 6,517 USD, P<0.001), and a lower percentage of out-of-pocket medical expenditure relative to total medical expenditure (17.2% vs. 27.7%, P<0.001). They were associated with higher in-hospital mortality (HR, 3.904; 95% CI, 2.533–6.039; P<0.001). Conclusions: Our study showed patients with benefit items had more medical resources and associated improved in-hospital survival. Patients with the aforementioned three benefit items had lower out-of-pocket medical expenditure due to the implementation of this policy, but higher in-hospital mortality.
Figure
Cited by 1 articles
-
The effect of socioeconomic status, insurance status, and insurance coverage benefits on mortality in critically ill patients admitted to the intensive care unit
Moo Suk Park
Acute Crit Care. 2022;37(1):118-119. doi: 10.4266/acc.2022.00129.
Reference
-
1. Ministry of Health and Welfare. Social security system in Korea [Internet]. Sejong: Ministry of Health and Welfare;2021. [cited 2021 May 25]. Available from: http://www.mohw.go.kr/eng/pl/pl0101.jsp?PAR_MENU_ID=1003&MENU_ID=100324.2. Lee WY, Shaw I. The impact of out-of-pocket payments on health care inequity: the case of National Health Insurance in South Korea. Int J Environ Res Public Health. 2014; 11:7304–18.
Article3. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–28.
Article4. An J, Kim S. Medical cost trends under national health insurance benefit extension in Republic of Korea. Int J Health Plann Manage. 2020; 35:1351–70.
Article5. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–8.
Article6. Bahk J, Kang HY, Khang YH. Trends in life expectancy among medical aid beneficiaries and National Health Insurance beneficiaries in Korea between 2004 and 2017. BMC Public Health. 2019; 19(1):1137.
Article7. Welfare services at a glance [Internet]. Seoul: Ministry of Health and Welfare and Korea Social Security Information Service;2021. [cited 2021 May 25]. Available from: https://www.bokjiro.go.kr/ssis-teu/index.do.8. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29.9. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure: on behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–10.
Article10. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying10 prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.11. Kutzin J, Sparkes SP. Health systems strengthening, universal health coverage, health security and resilience. Bull World Health Organ. 2016; 94:2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Health insurance policies for magnetic resonance imaging tests in Korea
- How to develop social consensus for the uninsured benefit in the social insurance system
- Moving toward Universal Coverage of Health Insurance in Vietnam: Barriers, Facilitating Factors, and Lessons from Korea
- Changes in dental care access upon health care benefit expansion to include scaling
- Towards universal coverage: an evaluation of the benefit enhancement plan for four major conditions in Korean National Health Insurance