Changes in dental care access upon health care benefit expansion to include scaling
- Affiliations
-
- 1Department of Health Policy and Management, Korea University College of Health Sciences, Seoul, Korea. junhlee@korea.ac.kr
- 2BK21 PLUS Program in Embodiment: Health-Society Interaction, Department of Public Health Sciences, Korea University Graduate School, Seoul, Korea.
- 3Department of Periodontology, Seoul National University School of Dentistry, Seoul, Korea.
- KMID: 2362906
- DOI: http://doi.org/10.5051/jpis.2016.46.6.405
Abstract
- PURPOSE
This study aimed to evaluate the effects of a policy change to expand Korean National Health Insurance (KNHI) benefit coverage to include scaling on access to dental care at the national level.
METHODS
A nationally representative sample of 12,794 adults aged 20 to 64 years from Korea National Health and Nutritional Examination Survey (2010-2014) was analyzed. To examine the effect of the policy on the outcomes of interest (unmet dental care needs and preventive dental care utilization in the past year), an estimates-based probit model was used, incorporating marginal effects with a complex sampling structure. The effect of the policy on individuals depending on their income and education level was also assessed.
RESULTS
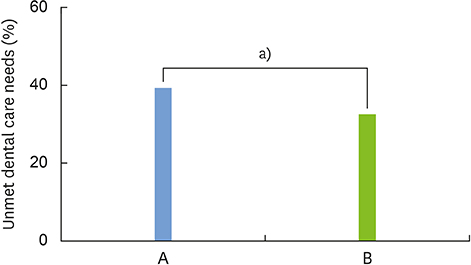
Adjusting for potential covariates, the probability of having unmet needs for dental care decreased by 6.1% and preventative dental care utilization increased by 14% in the post-policy period compared to those in the pre-policy period (2010, 2012). High income and higher education levels were associated with fewer unmet dental care needs and more preventive dental visits.
CONCLUSIONS
The expansion of coverage to include scaling demonstrated to have a significant association with decreasing unmet dental care needs and increasing preventive dental care utilization. However, the policy disproportionately benefited certain groups, in contrast with the objective of the policy to benefit all participants in the KNHI system.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Trends in the incidence of tooth extraction due to periodontal disease: results of a 12-year longitudinal cohort study in South Korea
Jae-Hong Lee, Jin-Young Oh, Jung-Kyu Choi, Yeon-Tae Kim, Ye-Sol Park, Seong-Nyum Jeong, Seong-Ho Choi
J Periodontal Implant Sci. 2017;47(5):264-272. doi: 10.5051/jpis.2017.47.5.264.Trends in the utilization of dental outpatient services affected by the expansion of health care benefits in South Korea to include scaling: a 6-year interrupted time-series study
Hee-Jung Park, Jun Hyup Lee, Sujin Park, Tae-Il Kim
J Periodontal Implant Sci. 2018;48(1):3-11. doi: 10.5051/jpis.2018.48.1.3.Factors associated with the persistence of unmet dental care needs
Xianhua Che, Hee-Jung Park
J Korean Acad Oral Health. 2018;42(4):152-158. doi: 10.11149/jkaoh.2018.42.4.152.The relationship between precarious work and unmet dental care needs in South Korea: focus on job and income insecurity
Xianhua Che, Hee-Jung Park
J Korean Acad Oral Health. 2018;42(4):167-174. doi: 10.11149/jkaoh.2018.42.4.167.
Reference
-
1. Kim S, Kwon S. Impact of the policy of expanding benefit coverage for cancer patients on catastrophic health expenditure across different income groups in South Korea. Soc Sci Med. 2015; 138:241–247.
Article2. Kim HS, Kim MK, Shin HS. Expenditure in ambulatory dental care and factors related to its spending. Health Policy Manag. 2012; 22:207–224.
Article3. Yeo JY, Jeong HS. Determinants of dental screening and unmet dental needs: interaction effect between geographical accessibility and economic affordability. Korean J Health Econ Policy. 2012; 18:109–126.4. Albandar JM. Global risk factors and risk indicators for periodontal diseases. Periodontol 2000. 2002; 29:177–206.
Article5. Buchwald S, Kocher T, Biffar R, Harb A, Holtfreter B, Meisel P. Tooth loss and periodontitis by socio-economic status and inflammation in a longitudinal population-based study. J Clin Periodontol. 2013; 40:203–211.
Article6. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANES VI-1). Cheongju: Korea Centers for Disease Control and Prevention;2014.7. Lee MY, Chang SJ, Kim CB, Chung WG, Choi EM, Kim NH. Community periodontal treatment needs in South Korea. Int J Dent Hyg. 2015; 13:254–260.
Article8. Park HJ, Lee JH. The Effect of socioeconomic status, oral health consciousness and behaviors on the periodontal-health disparities among Korean adults. J Korean Soc Health Educ Promot. 2010; 27:61–69.9. Kim DW, Park JC, Rim TT, Jung UW, Kim CS, Donos N, et al. Socioeconomic disparities of periodontitis in Koreans based on the KNHANES IV. Oral Dis. 2014; 20:551–559.
Article10. Borrell LN, Crawford ND. Socioeconomic position indicators and periodontitis: examining the evidence. Periodontol 2000. 2012; 58:69–83.
Article11. Grossman M. On the concept of health capital and the demand for health. J Polit Econ. 1972; 80:223–255.
Article12. Phelps CE, Newhouse JP. Coinsurance, the price of time, and the demand for medical services. Rev Econ Stat. 1974; 56:334–342.
Article13. Long SK, Stockley K. The impacts of state health reform initiatives on adults in New York and Massachusetts. Health Serv Res. 2011; 46:365–387.
Article14. Wang H, Norton EC, Rozier RG. Effects of the State Children’s Health Insurance Program on access to dental care and use of dental services. Health Serv Res. 2007; 42:1544–1563.
Article15. Mofidi M, Rozier RG, King RS. Problems with access to dental care for medicaid-insured children: what caregivers think. Am J Public Health. 2002; 92:53–58.
Article16. Nasseh K, Vujicic M. The impact of medicaid reform on children’s dental care utilization in Connecticut, Maryland, and Texas. Health Serv Res. 2015; 50:1236–1249.
Article17. Calvasina P, Muntaner C, Quiñonez C. Factors associated with unmet dental care needs in Canadian immigrants: an analysis of the longitudinal survey of immigrants to Canada. BMC Oral Health. 2014; 14:145.
Article18. Andersen RM, Davidson PL. Ethnicity, aging, and oral health outcomes: a conceptual framework. Adv Dent Res. 1997; 11:203–209.
Article19. World Health Organization. Oral health surveys: basic methods. 4th ed. Geneva: World Health Organization;1997.20. Dubin JA, Rivers D. Selection bias in linear regression, logit and probit models. Sociol Methods Res. 1989; 18:360–390.
Article21. Choi MK. The impact of medicaid insurance coverage on dental service use. J Health Econ. 2011; 30:1020–1031.
Article22. Chen L, Yip W, Chang MC, Lin HS, Lee SD, Chiu YL, et al. The effects of Taiwan’s National Health Insurance on access and health status of the elderly. Health Econ. 2007; 16:223–242.
Article23. Wagstaff A. Social health insurance reexamined. Health Econ. 2010; 19:503–517.
Article24. Giedion U, Alfonso EA, Diaz Y. The impact of universal coverage schemes in the developing world: a review of the existing evidence. Washington, D.C.: The World Bank;2013.25. Singhal A, Caplan DJ, Jones MP, Momany ET, Kuthy RA, Buresh CT, et al. Eliminating medicaid adult dental coverage in California led to increased dental emergency visits and associated costs. Health Aff (Millwood). 2015; 34:749–756.
Article26. Chen CS, Liu TC, Chen LM. National Health Insurance and the antenatal care use: a case in Taiwan. Health Policy. 2003; 64:99–112.
Article27. Lorant V, Boland B, Humblet P, Deliège D. Equity in prevention and health care. J Epidemiol Community Health. 2002; 56:510–516.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An exploratory study on development policy and the status of oral health care in the North Korea during the Kim Jong-Un era
- Awareness and satisfaction survey regarding national health insurance dental scaling
- Trends in the utilization of dental outpatient services affected by the expansion of health care benefits in South Korea to include scaling: a 6-year interrupted time-series study
- Disparities in High-cost Outpatient Imaging Test Utilization between Private Health Insurance Subscribers and Non-subscribers: Changes Following the National Health Insurance Benefit Expansion Policy
- Analysis of Some Online Questions with High Frequency about Dental Treatment in Korea