Ann Surg Treat Res.
2022 Apr;102(4):205-213. 10.4174/astr.2022.102.4.205.
Chronological trends in patients undergoing cholecystectomy in Korea: a nationwide health insurance claims study
- Affiliations
-
- 1Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Artificial Intelligence and Big-Data Convergence Center, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 3Department of Preventive Medicine, Gachon University College of Medicine, Incheon, Korea
- 4Center for Public Healthcare, Gachon University Gil Medical Center, Incheon, Korea
- KMID: 2527837
- DOI: http://doi.org/10.4174/astr.2022.102.4.205
Abstract
- Purpose
The incidence of gallstone disease and cholecystectomy is increasing worldwide. The aim of this study was to determine trends in the incidence of cholecystectomy in Korea.
Methods
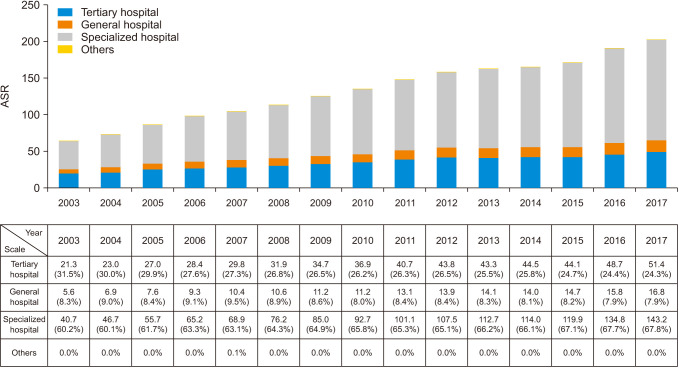
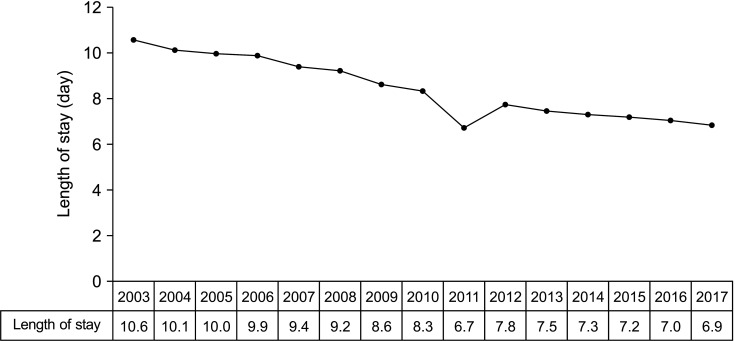
The National Health Insurance Services database was used to determine patterns in proportion of cholecystectomy and cholecystostomy in the total population of Korea from 2003 to 2017. The age-standardized rate (ASR) was calculated to compare the cholecystectomy and cholecystostomy according to changes in the population structure over time. The ASR was investigated according to patient age, sex, socioeconomic status, use of computed tomography, and type of hospital to identify trends.
Results
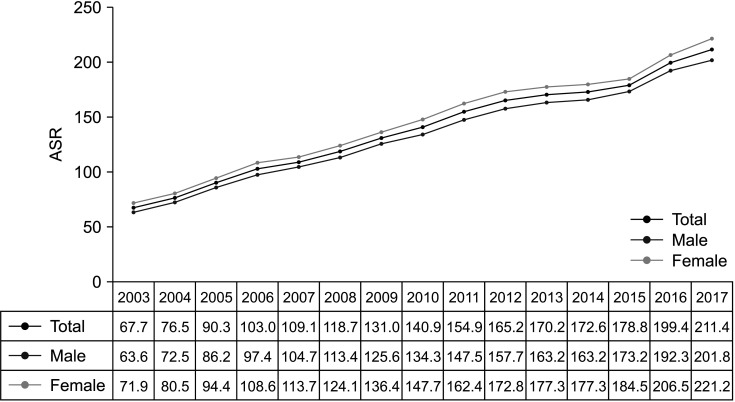
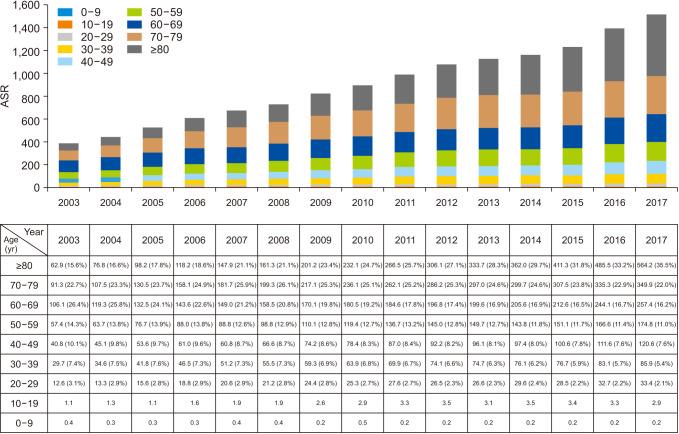
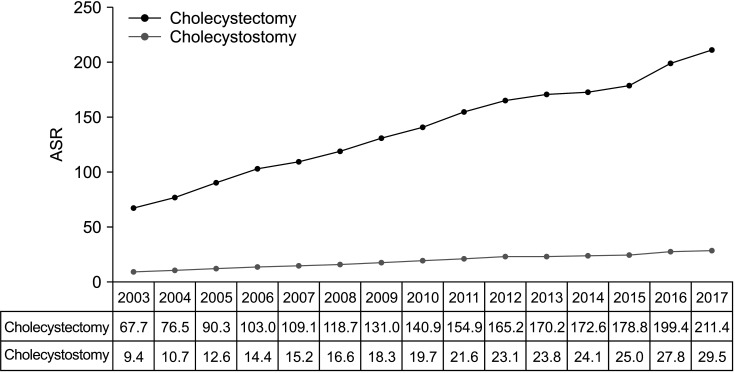
The ASR per 100,000 based on the 2010 population of cholecystectomy cases increased markedly from 67.7 to 211.4 between 2003 and 2017. The ASR was consistently higher in female than male (71.9 vs. 63.6 in 2003, 221.8 vs. 201.8 in 2017). Furthermore, the ASR for cholecystectomy increased with age, and surgery for gallstone disease was performed more often at a specialized center than at other medical facilities. The length of hospital stay of cholecystectomy decreased steadily from 10.6 days in 2003 to 6.9 days in 2017.
Conclusion
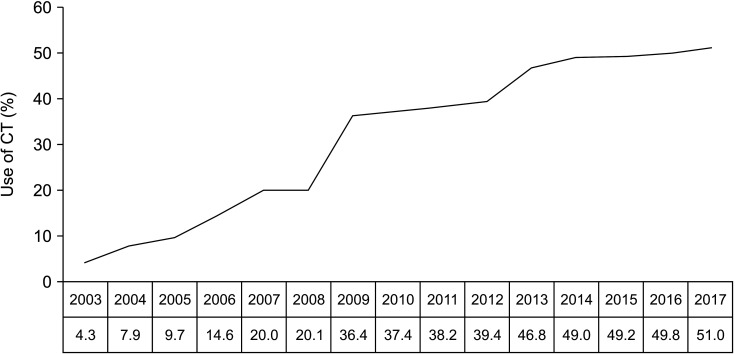
This study shows that the incidence of cholecystectomy and cholecystostomy has steadily increased over the years in Korea, with a trend toward older age and higher socioeconomic status in patients undergoing cholecystectomy. Increasing use of computed tomography investigations could be a primary cause for this trend. An integrated strategy is needed to manage the increase in older patients undergoing cholecystectomy and shorten their hospital stay with medical safety.
Keyword
Figure
Reference
-
1. Shaffer EA. Gallstone disease: epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006; 20:981–996. PMID: 17127183.2. Park YH, Park SJ, Jang JY, Ahn YJ, Park YC, Yoon YB, et al. Changing patterns of gallstone disease in Korea. World J Surg. 2004; 28:206–210. PMID: 14708060.
Article3. Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002; 97:249–254. PMID: 11866258.
Article4. Johnson AG. Reduced postoperative hospitalization after laparoscopic cholecystectomy. Br J Surg. 1991; 78:1019.
Article5. Health Insurance Review & Assessment Service (HIRA). National Health Insurance Service (NHIS). 2019 National Health Insurance statistical yearbook. Wonju: HIRA, NHIS;2020.6. Health Insurance Review & Assessment Service (HIRA). National Health Insurance Service (NHIS). 2005 National Health Insurance statistical yearbook. Wonju: HIRA, NHIS;2006.7. Kim HS, Cho SK, Kim CS, Park JS. Big data and analysis of risk factors for gallbladder disease in the young generation of Korea. PLoS One. 2019; 14:e0211480. PMID: 30794560.
Article8. Zhao J, Kim H, Han Y, Choi YJ, Byun Y, Kwon W, et al. Chronological changes in epidemiologic features of patients with gallstones over the last 20 years in a single large-volume Korean center. Ann Surg Treat Res. 2019; 97:136–141. PMID: 31508394.
Article9. Lee YJ, Park KS, Cho KB, Kim ES, Jang BK, Chung WJ, et al. Shifting prevalence of gallbladder polyps in Korea. J Korean Med Sci. 2014; 29:1247–1252. PMID: 25246743.
Article10. Chang YR, Jang JY, Kwon W, Park JW, Kang MJ, Ryu JK, et al. Changes in demographic features of gallstone disease: 30 years of surgically treated patients. Gut Liver. 2013; 7:719–724. PMID: 24312714.
Article11. Lee W, Roh YH, Kang SH, Kim CY, Choi Y, Han HS, et al. The chronological change of indications and outcomes for single-incision laparoscopic cholecystectomy: a Korean multicenter study. Surg Endosc. 2021; 35:3025–3032. PMID: 32583067.
Article12. Wadhwa V, Jobanputra Y, Garg SK, Patwardhan S, Mehta D, Sanaka MR. Nationwide trends of hospital admissions for acute cholecystitis in the United States. Gastroenterol Rep (Oxf). 2017; 5:36–42. PMID: 27174434.
Article13. Talseth A, Lydersen S, Skjedlestad F, Hveem K, Edna TH. Trends in cholecystectomy rates in a defined population during and after the period of transition from open to laparoscopic surgery. Scand J Gastroenterol. 2014; 49:92–98. PMID: 24354967.
Article14. Pak M, Lindseth G. Risk factors for cholelithiasis. Gastroenterol Nurs. 2016; 39:297–309. PMID: 27467059.
Article15. Kim CS, Ko SH, Kwon HS, Kim NH, Kim JH, Lim S, et al. Prevalence, awareness, and management of obesity in Korea: data from the Korea national health and nutrition examination survey (1998-2011). Diabetes Metab J. 2014; 38:35–43. PMID: 24627826.
Article16. Nam GE, Kim YH, Han K, Jung JH, Rhee EJ, Lee SS, et al. Obesity fact sheet in Korea, 2019: prevalence of obesity and abdominal obesity from 2009 to 2018 and social factors. J Obes Metab Syndr. 2020; 29:124–132. PMID: 32581145.
Article17. Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011; 34:1323–1328. PMID: 21505206.18. Lim S, Jang HC, Park KS, Cho SI, Lee MG, Joung H, et al. Changes in metabolic syndrome in American and Korean youth, 1997-2008. Pediatrics. 2013; 131:e214–e222. PMID: 23209102.
Article19. Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017; 389:1323–1335. PMID: 28236464.
Article20. Hong N, Kim KJ, Lee SJ, Kim CO, Kim HC, Rhee Y, et al. Cohort profile: Korean Urban Rural Elderly (KURE) study, a prospective cohort on ageing and health in Korea. BMJ Open. 2019; 9:e031018.
Article21. Pisano M, Ceresoli M, Cimbanassi S, Gurusamy K, Coccolini F, Borzellino G, et al. 2017 WSES and SICG guidelines on acute calcolous cholecystitis in elderly population. World J Emerg Surg. 2019; 14:10. PMID: 30867674.
Article22. Han SR, Kim HJ, Kim NH, Shin S, Yoo RN, Kim G, et al. Inguinal hernia surgery in Korea: nationwide data from 2007-2015. Ann Surg Treat Res. 2019; 97:41–47. PMID: 31297352.
Article23. Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, et al. Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. 2015; 18:196–204. PMID: 25958296.
Article24. Jensen KK, Roth NO, Krarup PM, Bardram L. Surgical management of acute cholecystitis in a nationwide Danish cohort. Langenbecks Arch Surg. 2019; 404:589–597. PMID: 31297607.
Article25. Ryan JM, O’Connell E, Rogers AC, Sorensen J, McNamara DA. Systematic review and meta-analysis of factors which reduce the length of stay associated with elective laparoscopic cholecystectomy. HPB (Oxford). 2021; 23:161–172. PMID: 32900611.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sensitivity of Medical Insurance Claims Data Using Population-based Cancer Registry Data
- Trends and Clinical Characteristics of Next-Generation Sequencing–Based Genetic Panel Tests: An Analysis of Korean Nationwide Claims Data
- Clinical Study Using Healthcare Claims Database
- A Comparison of Laparoscopic Cholecystectomy with Open Cholecystectomy in a Korean Hospital
- Response: Trends in Hyperglycemic Crisis Hospitalizations and in- and out-of-Hospital Mortality in the Last Decade Based on Korean National Health Insurance Claims Data (Endocrinol Metab 2019;34:275–81, Ji Hong You et al.)