J Cerebrovasc Endovasc Neurosurg.
2022 Mar;24(1):63-72. 10.7461/jcen.2022.E2021.07.002.
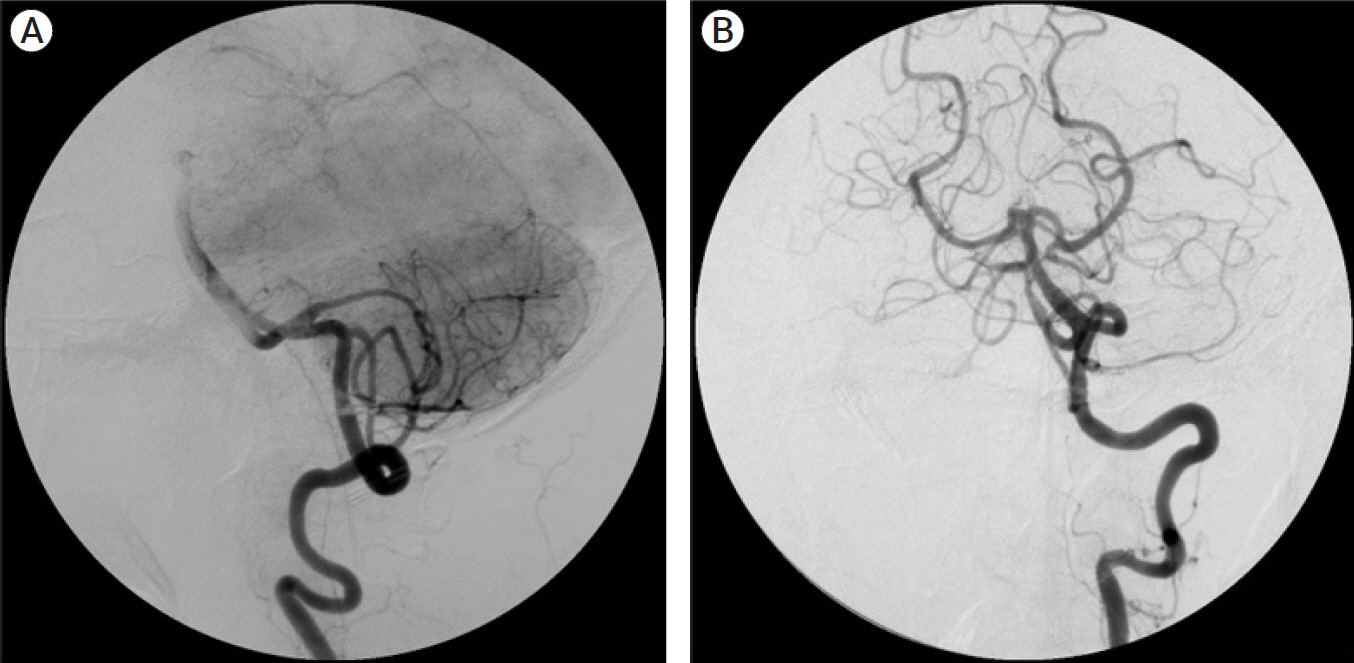
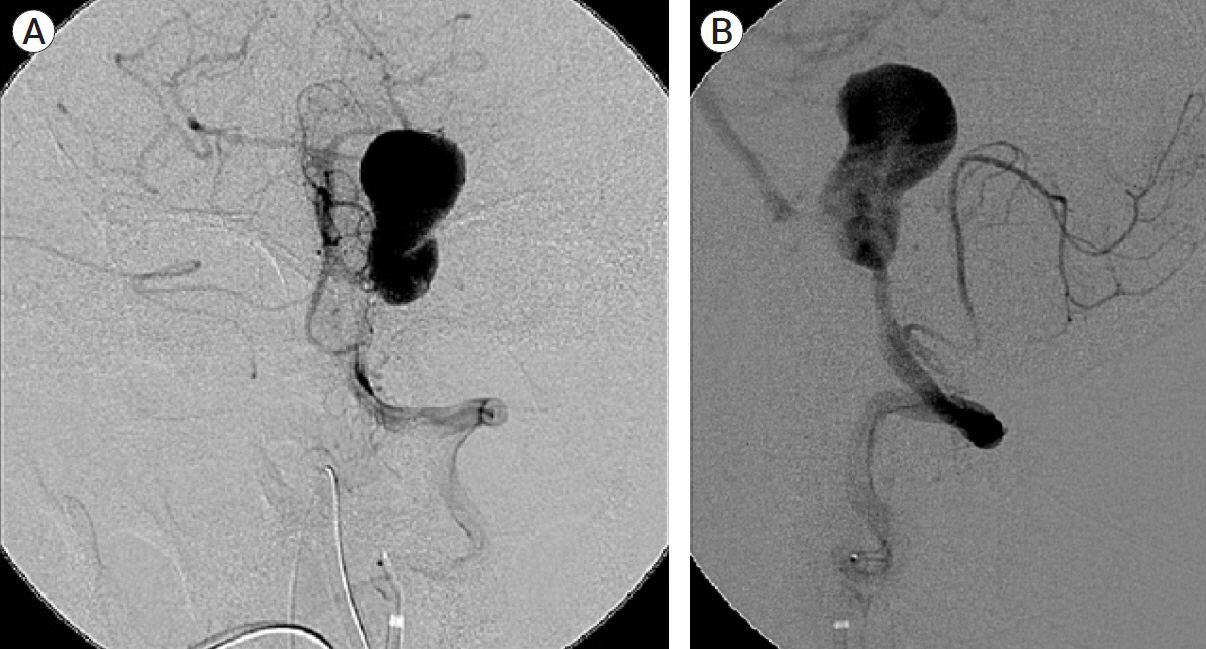
Giant vertebral artery aneurysms presenting acutely with WFNS grade five subarachnoid haemorrhage, report of 4 cases treated with endovascular or surgical proximal parent artery occlusion achieving good functional outcome
- Affiliations
-
- 1Consultant Neurosurgeon, Mount Elizabeth Medical Centre, Singapore 228510, Singapore
- KMID: 2527597
- DOI: http://doi.org/10.7461/jcen.2022.E2021.07.002
Abstract
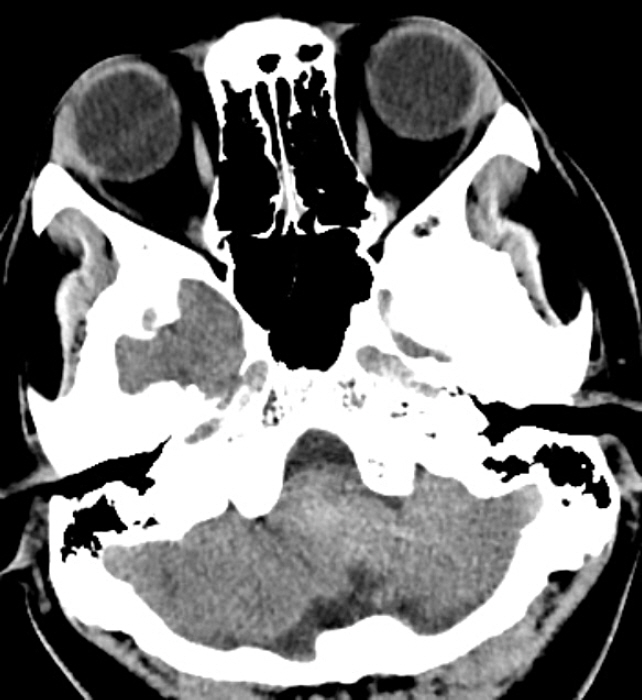
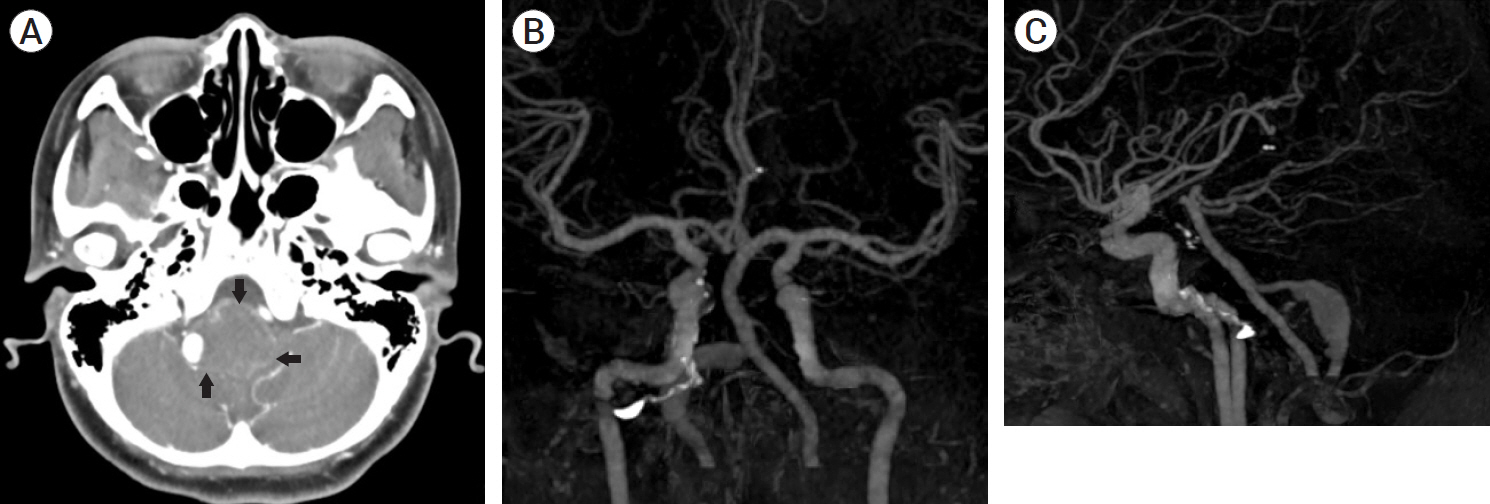
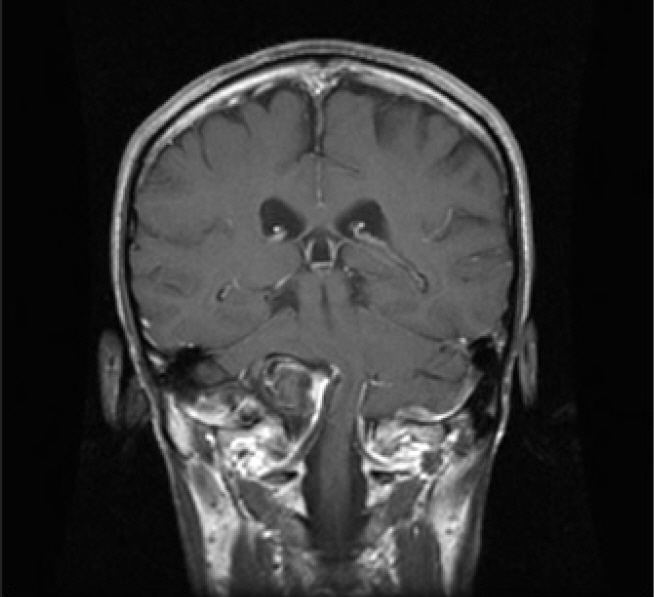
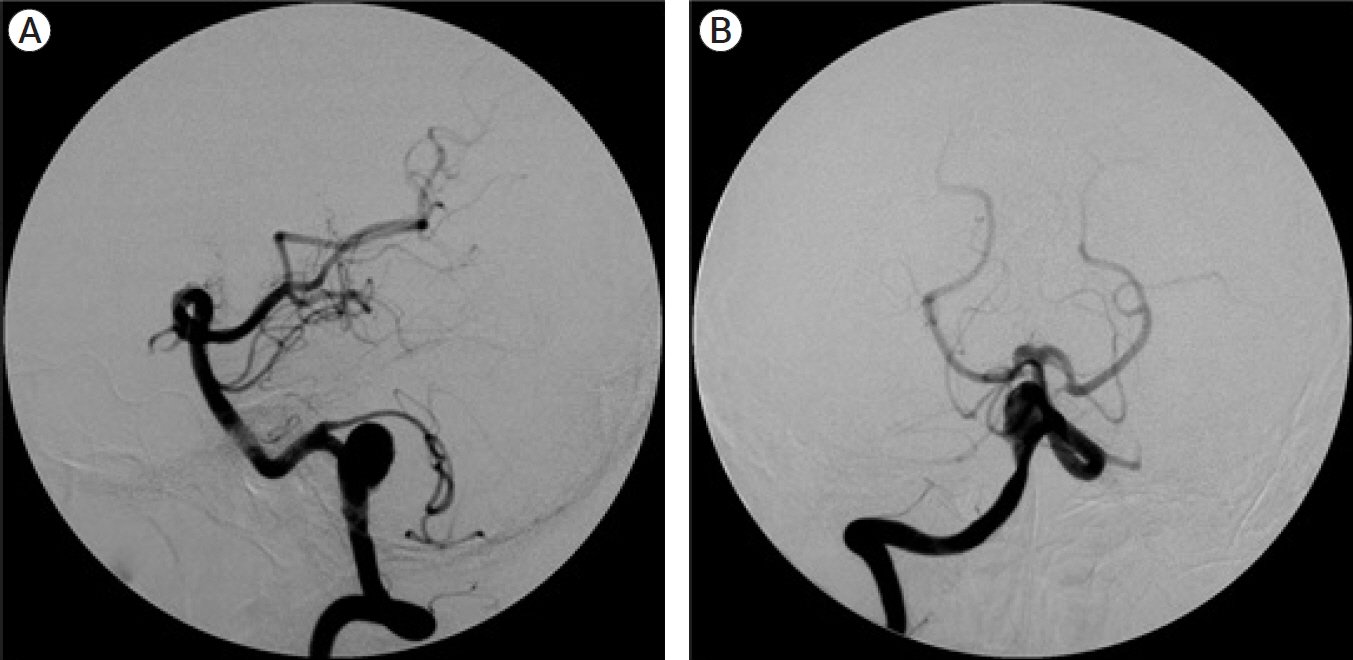
- Ruptured giant aneurysms in the posterior circulation with poor grade subarachnoid haemorrhage (SAH) are associated with poor outcome. In this report four patients with ruptured giant vertebral artery aneurysms who presented acutely with World Federation of Neurosurgical Societies (WFNS) grade five SAH are reviewed. All 4 cases required intubation and ventilation on arrival. Brainstem reflexes were intact in all of them. Early endovascular parent artery coil occlusion was done in two cases. Two other cases were treated with early surgical proximal parent artery clip occlusion. Two cases required ventriculoperitoneal shunting. All cases achieved good recovery with full functional independent outcome at two years follow up. MR angiogram at two years documented resolution of aneurysms. In conclusion good outcome may be possible in some cases of ruptured giant vertebral artery aneurysms with WFNS grade five SAH.
Figure
Reference
-
1. Batjer H. Giant aneurysms of the posterior circle of Willis and its branches. In : Awad I, Barrow D, editors. Giant Intracranial Aneurysms. American Association of Neurological Surgeons;1995. p. 175–96.2. Brinjikji W, Piano M, Fang S, Pero G, Kallmes DF, Quilici L, et al. Treatment of ruptured complex and large/giant ruptured cerebral aneurysms by acute coiling followed by staged flow diversion. J Neurosurg. 2016; Jul. 125(1):120–7.
Article3. Cagnazzo F, Mantilla D, Rouchaud A, Brinjikji W, Lefevre PH, Dargazanli C, et al. Endovascular treatment of very large and giant intracranial aneurysms: comparison between reconstructive and deconstructive techniques-a meta-analysis. AJNR Am J Neuroradiol. 2018; May. 39(5):852–8.
Article4. Campos JK, Ball BZ, II BC, Sweidan AJ, Hasjim BJ, Hsu FPK, et al. Multimodal management of giant cerebral aneurysms: review of literature and case presentation. Stroke and Vascular Neurology. 2020; Mar. 5(1):22–8.
Article5. Gmeiner M, Gruber A. Current strategies in the treatment of intracranial large and giant aneurysms. Acta Neurochir Suppl. 2021; 132:19–26.
Article6. Hamilton M, Kraus G, Daspit P, Spetzler R. Giant aneurysm of the vertebrobasilar trunk. In : Awad I, Barrow D, editors. Giant Intracranial Aneurysms. American Association of Neurological Surgeons;1995. p. 197–222.7. Molyneux A, Kerr R, Yu L, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005; Sep. 366(9488):809–17.
Article8. Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, Hashimoto N, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. New England Journal of Medicine. 2012; Jun. 366(26):2474–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rupture of the Giant Vertrbrobasilar Aneurysm After Hunterian Vertebral Artery Occlusion
- Fusiform “True” Posterior Communicating Artery Aneurysm with Basilar Artery Occlusion: A Case Report
- Salvage flow diverter stent across the posterior communicating artery for persistent retrograde filling of a giant internal carotid artery aneurysm after parent vessel occlusion
- Growing Thrombosed Dissecting Aneurysm of the Vertebral Artery after Endovascular Proximal Artery Occlusion: the Role of the Vasa Vasorum
- Bilateral Vertebral Artery Dissecting Aneurysms: A Long Term Follow-up Results of Microsurgical Trapping and Proximal Occlusion