J Cerebrovasc Endovasc Neurosurg.
2021 Jun;23(2):123-129. 10.7461/jcen.2021.E2020.09.002.
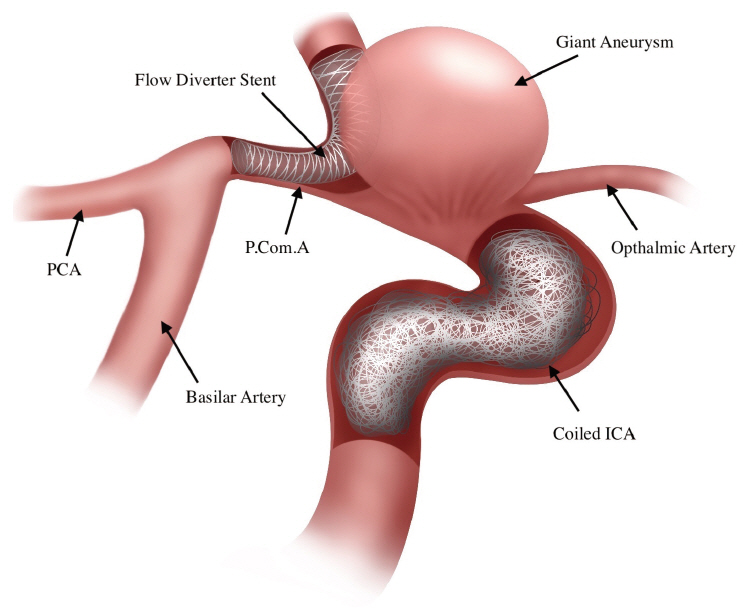
Salvage flow diverter stent across the posterior communicating artery for persistent retrograde filling of a giant internal carotid artery aneurysm after parent vessel occlusion
- Affiliations
-
- 1Department of Radiology, King Fahad Medical City, Riyadh, Saudi Arabia
- 2Department of Neurosurgery, King Abdulaziz Speciality Hospital, Taif, Saudi Arabia
- 3Department of Adult Neurosurgery, National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia
- KMID: 2517025
- DOI: http://doi.org/10.7461/jcen.2021.E2020.09.002
Abstract
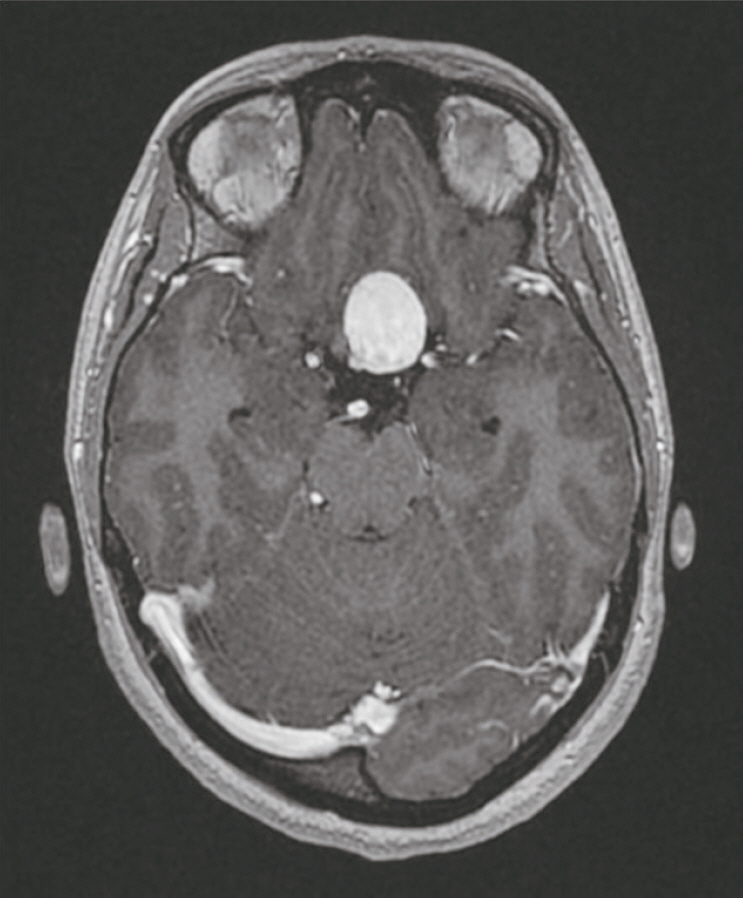
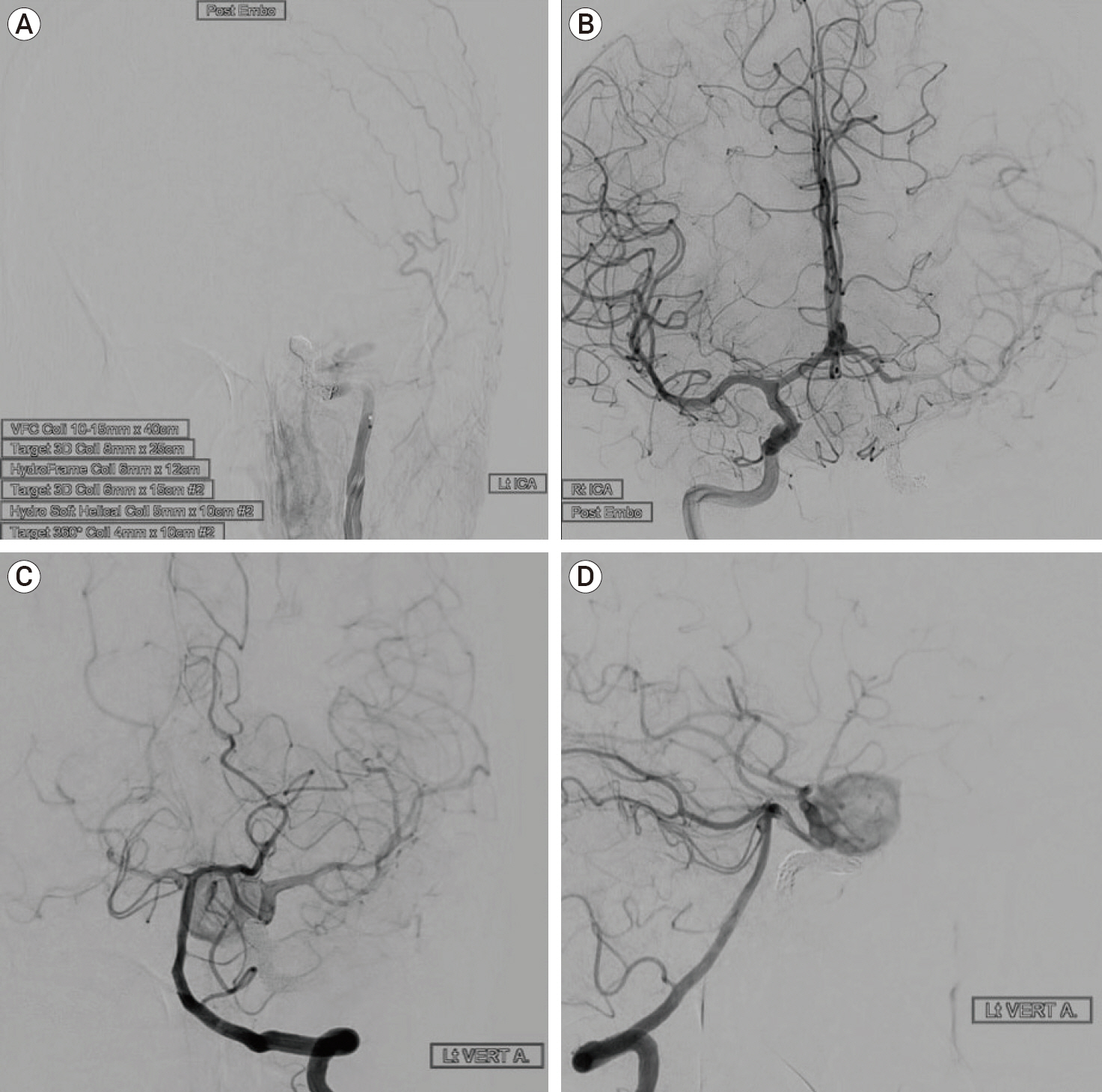
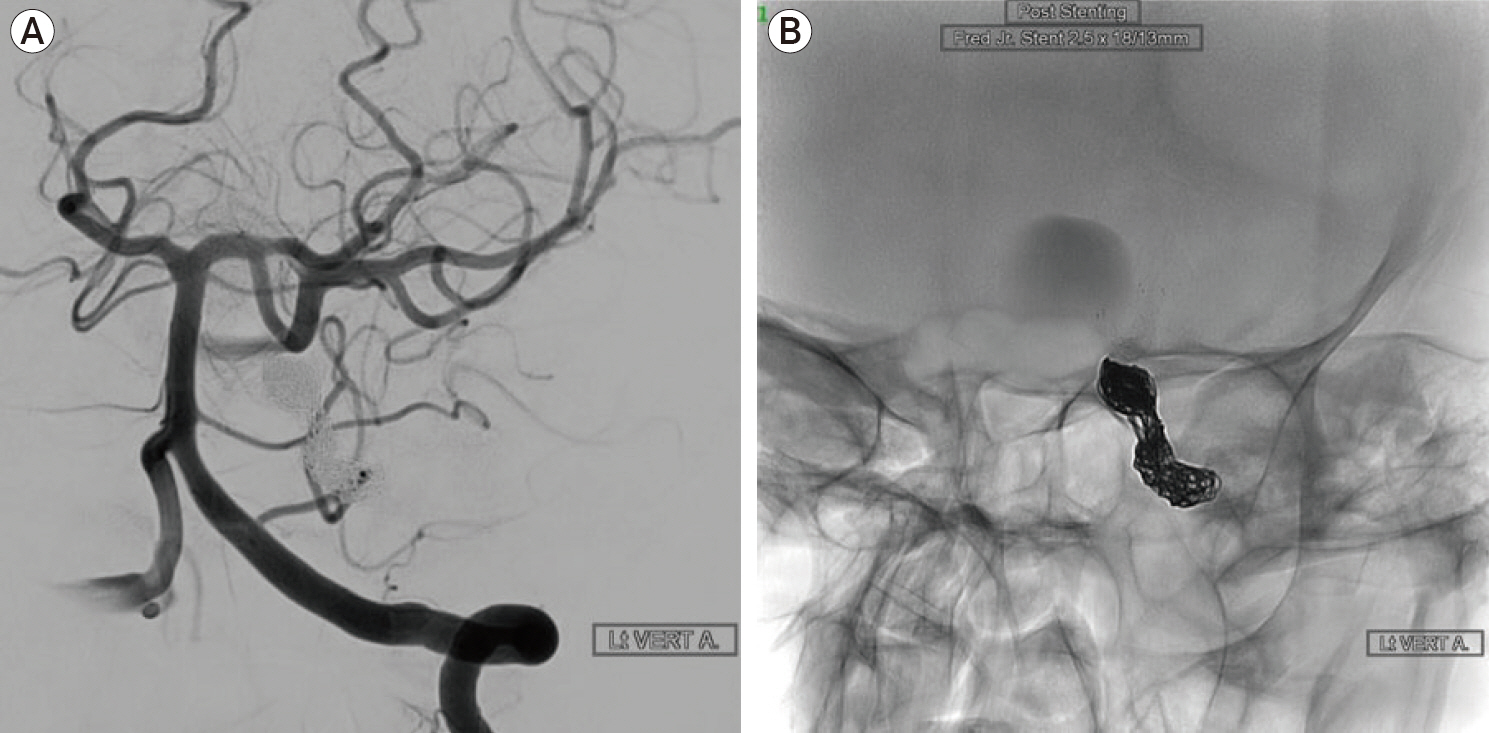
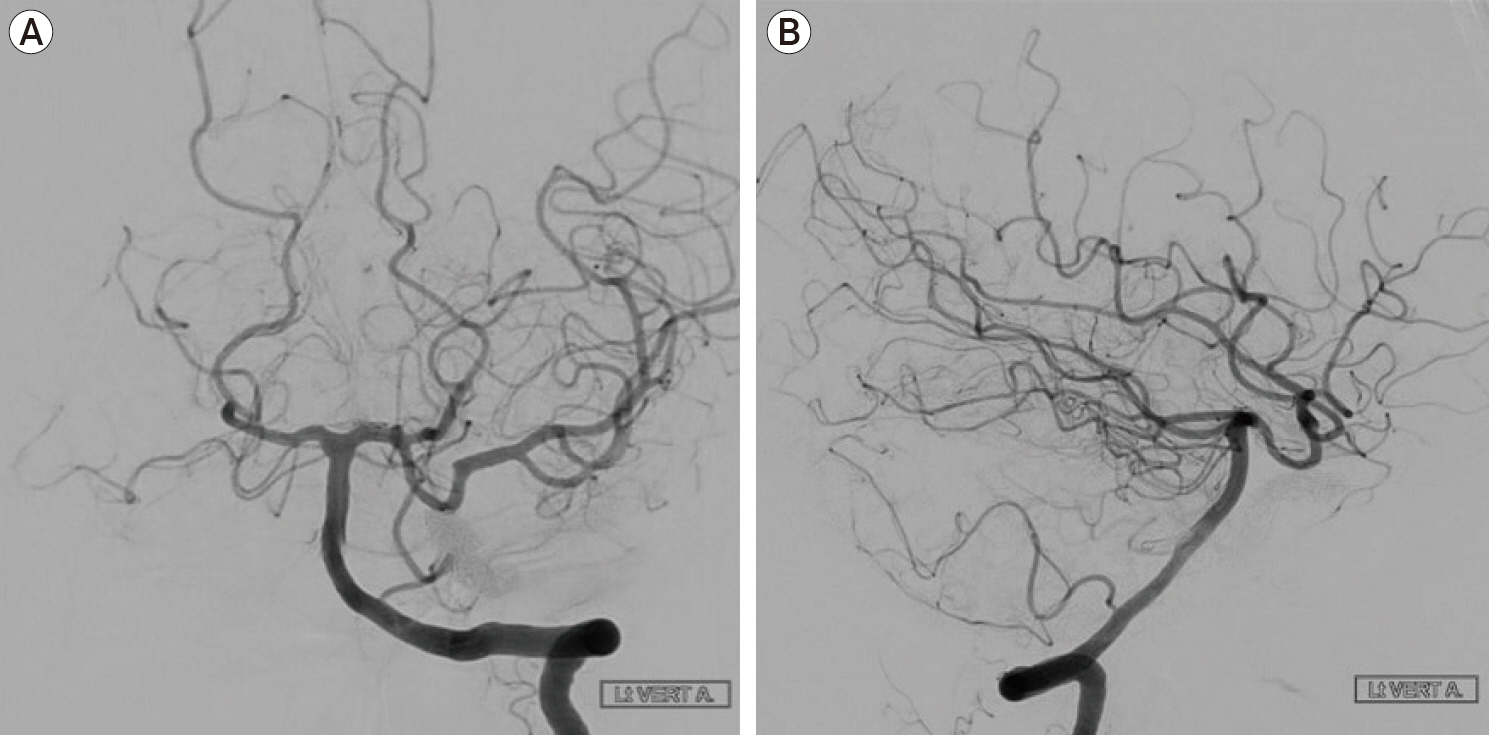
- Giant internal carotid artery (ICA) aneurysms are complex vascular lesions which are difficult to treat with open as well as endovascular surgery. Parent vessel occlusion is a well-established treatment option for such aneurysms. However, there have been a few reported cases of ruptured aneurysms related to the persistent retrograde filling after parent vessel occlusion. We report a case which highlights the usage of the flow diverter stent as a potential treatment strategy for the management of retrograde filling of aneurysms. A 54-year-old female was found to have a giant left ICA aneurysm on a brain magnetic resonance imaging during workup for headaches. She underwent occlusion of the left ICA proximal to the aneurysm using multiple coils. However, follow up angiograms after 6 months and 2 years demonstrated persistent retrograde filling of the left ICA aneurysm through the posterior communicating (PCOM) artery. Eventually, she was successfully treated with a flow diverter stent across the PCOM artery into the distal ICA. Follow up angiogram after 6 months showed patent flow in the PCOM artery and the distal ICA. with complete occlusion of the aneurysm. Using a flow diverter stent after insufficient parent vessel occlusion for giant intracranial aneurysms may be a feasible treatment option and an addition to the neurovascular treatment armamentarium.
Keyword
Figure
Reference
-
1. Adeeb N, Griessenauer CJ, Shallwani H, Shakir H, Foreman PM, Moore JM, et al. Pipeline embolization device in treatment of 50 unruptured large and giant aneurysms. World Neurosurg. 2017; Sep. 105:232–7.
Article2. Bechan RS, Majoie CB, Sprengers ME, Peluso JP, Sluzewski M, Van Rooij WJ. Therapeutic internal carotid artery occlusion for large and giant aneurysms: A single center cohort of 146. Am J Neuroradiol. 2016; 37(1):125–9.3. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013; Jun. 267(3):858–68.
Article4. Cui L, Peng Q, Ha W, Zhou D, Xu Y. Parent artery occlusion for intracranial aneurysms. Interv Neuroradiol. 2009; Sep. 15(3):309–15.
Article5. Gurian JH, Viñuela F, Gobin YP, Waston VE, Duckwiler GR, Gulielmi G. Aneurysm rupture after parent vessel sacrifice: treatment with Guglielmi detachable coil embolization via retrograde catheterization: case report. Neurosurgery. 1995; Dec. 37(6):1216–20. discussion 1220-1.6. Sluzewski M, Menovsky T, van Rooij WJ, Wijnalda D. Coiling of very large or giant cerebral aneurysms: long-term clinical and serial angiographic results. AJNR Am J Neuroradiol. 2003; Feb. 24(2):257–62.7. Solomon RA, Fink ME, Pile-Spellman J. Surgical management of unruptured intracranial aneurysms. J Neurosurg. 1994; Mar. 80(3):440–6.
Article8. van Rooij WJ, Sluzewski M, Metz NH, Nijssen PC, Wijnalda D, Rinkel GJ, et al. Carotid balloon occlusion for large and giant aneurysms: evaluation of a new test occlusion protocol. Neurosurgery. 2000; Jul. 47(1):116–21. discussion 122.
Article9. Vincent F, Weill A, Roy D, Raymond J, Guilbert F. Carotid ophthalmic aneurysm rupture after parent vessel occlusion. AJNR Am J Neuroradiol. 2005; Jun-Jul. 26(6):1372–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Kinking of Flow Diverter in a Giant Wide-Necked Supraclinoid Internal Carotid Artery Aneurysm
- Fusiform “True” Posterior Communicating Artery Aneurysm with Basilar Artery Occlusion: A Case Report
- Symptomatic Post Endarterectomy Common Carotid Artery Pseudoaneurysm Treated with Combination of Flow Diverter Implantation and Carotid Stenting
- Retreatment of a recurrent giant aneurysm of the internal carotid artery after treatment with a flow-diverting stent
- Intracranial Aneurysm Associated with Aplasia of the Internal Cartoid Artery